Abstract
Objective: To examine the effect of abciximab treatment on intensive care length of stay for patients undergoing percutaneous coronary intervention (PCI).
Design and setting: A retrospective study conducted in a naturalistic setting.
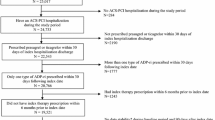
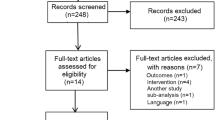
Methods: A 2-stage econometric model was used to control for the influence of possible selection bias across categories of patients and for both observable and unobservable factors correlated with each patient’s treatment selection and length of stay in intensive care. Multivariate analysis was applied to control for a wide range of factors (patient demographics, insurance provider, health conditions, admission and discharge information, and hospital characteristics) that may influence intensive care length of stay. Retrospective data were obtained from HCIA’s Clinical Pathways Database.
Participants: Patients (n = 13 364) who were hospitalised in any of 87 hospitals across the US over the period from October 1, 1995 to December 1, 1996.
Results: After controlling for high-risk indications and selection bias, results indicated that administration of abciximab was associated with a significantly shorter length of stay in intensive care compared with not administering a GPIIb/IIIa inhibitor (0.45 fewer days; p ≤ 0.0001). In a subgroup analysis of patients having an acute myocardial infarction (n = 4793), administration of abciximab was also associated with a significantly shorter intensive care stay (0.27 fewer days; p < 0.0001).
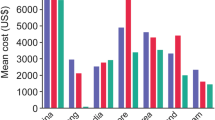
Conclusion: Results of this study indicate that the administration of abciximab is associated with a reduction in the length of stay in intensive care. This reduction implies potential cost offsets for patients undergoing PCI who receive abciximab.


Similar content being viewed by others
References
Mak KH, Challapalli R, Eisenberg MJ, et al. Effect of platelet glycoprotein IIb/IIIa receptor inhibition on distal embolization during percutaneous revascularization of aortocoronary sapheneous vein grafts. Am J Cardiol 1997; 80: 985–8
Lefkovitz J, Ivanhoe RJ, Califf RM, et al. Effects of platelet glycoprotein IIb/IIIa receptor blockade by a chimeric monoclonal antibody (abciximab) on acute and six-month outcomes after percutaneous transluminal coronary angioplasty for acute myocardial infarction. Am J Cardiol 1996; 70: 1045–51
Califf RM, Lincoff AM, Tcheng JE, et al. An overview of the results of the EPIC trial. Eur Heart J 1995; 16 Suppl. L: 43–9
Topol EJ, Ferguson JJ, Weisman HF, et al. Long-term protection from myocardial ischemic events in a randomized trial of brief integrin beta3 blockade with percutaneous coronary intervention. JAMA 1997; 278: 479–84
Adgey AAJ. An overview of the results of clinical trials with glycoprotein IIb/IIIa inhibitors. Eur Heart J 1998; 19 Suppl. D: D10-D21
EPILOG Investigators. Platelet glycoprotein IIb/IIIa receptor blockade and low-dose heparin during percutaneous coronary revascularization. N Engl J Med 1997; 336 (24): 1689–96
Tcheng JE. Glycoprotein IIb/IIIa receptor inhibitors: putting the EPIC, IMPACT II, RESTORE, and EPILOG trials into perspective. Am J Cardiol 1996; 31: 35–40
Topol EJ, Mark DB, Lincoff AM, et al. Outcomes at 1 year and economic implications of platelet glycoprotein IIb/IIIa blockade in patients undergoing coronary stenting: results from a multicentre randomised trial. Lancet 1999; 354: 2019–24
CAPTURE Study. Randomised placebo-controlled trial of abciximab before and during coronary intervention in refractory unstable angina: the CAPTURE study. Lancet 1997; 349: 1429–35
Kereiakes DJ, Lincoff AM, Miller DP, et al. Abciximab therapy and unplanned coronary stent deployment: favorable effects on stent use, clinical outcomes, and bleeding complications. Circulation 1998; 97: 857–64
Edbrooke D, Hibbert C, Ridley S, et al. The development of a method for comparative costing of individual intensive care units. Anesthesia 1999; 54: 110–20
Halpern NA, Bettes L, Greenstein R. Federal and nationwide intensive care units and healthcare costs: 1986–1992. Crit Care Med 1994; 22: 2001–7
Weissman C. Analyzing intensive care unit length of stay data: problems and possible solutions. Crit Care Med 1997; 25: 1594–600
Knaus WA, Wagner DP, Zimmerman JE, et al. Variations in mortality and length of stay in intensive care units. Ann Intern Med 1993; 118 (10): 755–61
Zimmerman JE, Shortell JM, Rousseau DM, et al. Improving intensive care: observations based on organizational case studies in nine intensive care units: a prospective, multicenter study. Crit Care Med 1993; 21 (10): 1443–51
Lee LF. Generalized models with selectivity. Econometrica 1983; 51: 507–12
Matsui K, Goldman L, Johnson PA, et al. Comorbidity as a correlate of length of stay for hospitalized patients with acute chest pain. J Gen Intern Med 1996; 11: 262–8
Every NR, Spertus J, Fihn SD, et al. Length of hospital stay after acute myocardial infarction in the myocardial infarction triage and intervention (MITI) project registry. J Am Coll Cardiol 1996; 28: 287–93
Greene WH. Econometric analysis. Upper Saddle River (NJ): Prentice-Hall, 1997
Heckman J. Sample selection bias as a specification error. Econometrica 1979; 47: 153–61
Barnow BS, Cain GG, Goldberger AS. Issues in the analysis of selectivity bias. In: Stromsdorfer EW, Farkas G, editors. Evaluation studies review annual. Vol. 5. Beverly Hills (CA): Sage Publications, 1980
Greene WH. LIMDEP. Version 7.0 user’s manual. Plainview (NY): Econometric Software, 1998
Melfi C, Holleman E, Arthur D, et al. Selecting a patient characteristic index for the prediction of medical outcomes using administrative claims data. J Clin Epidemiol 1995; 48: 917–26
Weitzman S, Cooper L, Chambless L, et al. Gender, racial, and geographic differences in the performance of cardiac diagnostic and therapeutic procedures for hospitalized acute myocardial infarction in four states. Am J Cardiol 1997: 79: 722–6
Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med 1991: 325: 221–5
Steingart RM, Packer M, Hamm P, et al. Sex differences in the management of coronary artery disease. N Engl J Med 1991: 325: 226–30
Maynard C, Every NR, Martin RS, et al. Long-term implications of racial differences in the use of revascularization procedures (the Myocardial Infarction Triage and Intervention Registry). Am Heart J 1997: 133 (6): 656–62
Peterson ED, Wright SM, Daley J, et al. Racial variation in cardiac procedure use and survival following myocardial infarction in the Department of Veterans Affairs. JAMA 1994: 271: 1175–80
Ayanian JZ, Udvarheyli IS, Gastonis CA, et al. Racial differences in the use of revascularization procedures after coronary angioplasty. JAMA 1993: 269: 2642–6
Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease inMassachusetts. JAMA 1989: 261: 253–7
Braunwald E, Maseri P, Armstrong PW, et al. Rationale and clinical evidence for the use of GP IIb/IIIa inhibitors in acute coronary syndromes. Eur Heart J 1998; 19 Suppl. D: D22-D30
Lage MJ, Barber BL, Bowman L, et al. Shorter hospital stays for angioplasty patients who receive abciximab. J Invasive Cardiol 2000; 12: 179–86
van Hout BA, Bowman L, Zelinger DJ, et al. Costs and effects in therapy for acute coronary syndromes: the case of abciximab in high-risk patients undergoing percutaneous transluminal coronary angioplasty in the EPIC study. Eur Heart J 1998; 19 Suppl. D: D59-D66
Goklaney AK, Murphy JD, Hillegass WB. Abciximab therapy in percutaneous intervention: economic issues in the United States. Eur Heart J 1998; 19 Suppl. D: D52-D58
Becker RB, Zimmerman JE, Knaus WE, et al. The use of APACHE III to evaluate ICU length of stay, resource use, and mortality after coronary artery by-pass surgery. J Cardiovasc Surg 1995; 36: 1–11
McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality?: analysis using instrumental variables. JAMA1994; 272: 859–66
Takala J, Roukonen E. Cost and resource utilization in intensive care. In: Vincent JL, editor. Yearbook of intensive care and emergency medicine. Berlin, Heidelberg, New York (NY): Springer, 1997: 885–95
van Hout BA, Simoons ML. Costs and effects of c7E3 in high risk PTCA patients: an indirect analysis for the Netherlands. Eur Heart J 1995; 16 Suppl. L: 81–5
Lincoff AM, Califf RM, Anderson KM, et al. Evidence for prevention of death and myocardial infarction with platelet membrane glycoprotein IIb/IIIa receptor blockade by abciximab (c7E3 Fab) among patients with unstable angina undergoing percutaneous coronary revascularization. J Am Coll Cardiol 1997; 30: 149–56
Acknowledgements
Funding provided by Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lage, M.J., Barber, B.L., Bala, M. et al. Association between Abciximab and Length of Stay in Intensive Care for Patients Undergoing Percutaneous Coronary Intervention. Pharmacoeconomics 18, 581–589 (2000). https://doi.org/10.2165/00019053-200018060-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200018060-00005