Summary
Synopsis
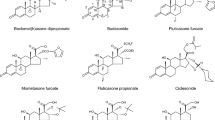
Budesonide is an inhaled corticosteroid that is used prophylactically to reduce the underlying inflammation and consequent airways narrowing associated with asthma. Widespread clinical experience has shown that inhaled budesonide is effective and well tolerated, and its use is well established in the management of adult and childhood asthma.
In developed countries, asthma is a major health problem and consumes a large proportion of healthcare resources. Both the prevalence and severity of asthma appear to be increasing. Additionally, asthma-related mortality has been reported to have gradually increased since the mid-to late-1970s in many countries, possibly due to undertreatment and/or suboptimal management of the disease. Current guidelines recommend a shift away from initial treatment with oral bronchodilators, such as theophylline, or regular use of β2-agonist inhalers, toward the earlier use of more expensive inhalers containing corticosteroids. Inhaled bronchodilators are still used as indicated for treatment acacute attacks.
Data suggest that the acquisition cost of budesonide is more than offset by decreased morbidity and reductions in costs associated with acme asthma exacerbations. Both once-daily administration and its administration in dry powder form via Turbuhaler® appear to be well accepted by patients; these factors may potentially improve patient compliance with therapy. Budesonide appears to have positive effects on some quality-of-life indices, although studies using validated quality-of-life instruments are needed to confirm these conclusions. Modelling studies would be helpful in order to assess the possible economic benefits to society through reduction of the considerable direct and indirect costs of asthma and cost-effectiveness comparisons with other inhaled corticosteroids are needed to clarify its relative positioning in this regard. Until then, the available data provide an encouraging pharmacoeconomic rationale for budesonide as firstline asthma therapy, and a good basis for future pharmacoeconomic analysis of asthma management.
Phormocoeconomic Benefits and Costs
Recent studies have estimated the costs of asthma in the US, Australia (New South Wales) and Sweden at $US6.2 billion (1990 dollars), $A209 million (1989 dollars) and SEK2.6 billion (1991 Swedish kronor), respectively. In these studies, total direct medical costs associated with hospitalisation, emergency care and asthma drug therapy generally represented the largest proponion of the total costs related to asthma. Substantial indirect costs were associated with loss of school days in children, loss of outside employment or housekeeping (either due of asthma or the need to care for children with asthma), and premature death. It is difficult to assign a monetary value to intangible costs: however, the negative impact of asthma on quality of life is likely to be one of the major perceived costs from the perspective of the patient or caregiver of a child with asthma.Accordingly, in 1 study, children rated respiratory symptoms, emotional function.physical activity limitations, and drug-related problems as ‘bothersome’ features of their disease; parents rated emotional items (worry and concern about various aspects of the disease) higher than items related to interference with daily activities.
Pharmocoeconomic Considerations
Although cost estimates were not included, budesonide markedly reduced oral prednisolone requirements, hospital admissions, and days spent in clinic in patients with asthma who were dependent on oral conicosteroids. In a large Swedish retrospective pooled regression analysis, a significant negative correlation between consumption of inhaled eonieosteroids and duration of hospitalisation was reponed. The cost of inhaled conicosteroids was covered by a reduction in hospitalisation costs in the sub-models evaluated in this study.
In 2 placebo-controlled double-blind studies which used symptom-free days as one of the composite measures of clinical efficacy, cost-effectiveness ratios were in favour of inhaled budesonide recipients. The use of the symptom-free day as an end-point in phannacocconomic evaluations has been criticised, and therefore more well-designed trials are required to validate th is outcome measurement. Studies arc also needed to assess the marginal cost effectiveness of budesonide relative to clinically relevant asthma treatments, particularly other inhaled conicosteroids.
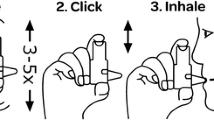
In 2 large noncomparative studies, inhaled budesonide demonstrated some improvements in sleep and lifestyle indices relative to baseline in patients with mild to moderate asthma. The majority of patients in I study reponed improvements in feeling rested upon waking, limitation of physical activity by asthma, ability to perfonn hard physical work, and overall satisfaction with lifestyle.Inhaled budesonide administered once daily at night in dry powder fonn via Turbuhaler® was associated with significant improvements in patient scores at 4 and 8 weeks relative to baseline scores for some measures of lifestyle indices. 100% of physicians and patients judged the Turbuhaler® easy to usc and 97% of patients preferred once-daily administration to previous multiple-dose regimens: both of these factors may improve patient compliance with treatment. While non-validated quality-of-life surveys were used to assess the effects of budesonide on patients’ lifestyles, suggesting that the results of these studies must be interpreted with caution. the findings have been consistent. In addition. comparative studies are needed to demonstrate any quality-of-life benefits of budesonide relative to other asthma treatments.
Similar content being viewed by others
References
Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med 1992 Mar 26: 326: 862–6
Mellis CM, Peat JK, Bauman AE. The cost of asthma in New South Wales. Med J Aust 1991 Oct 21: 155: 522–8
Lenney W, Wells NEJ, O’Neill BA. The burden of paediatric asthma. Eur Resp Rev 1994 Jan: 4: 49–62
Bauman A. Has the prevalence of asthma symptoms increased in Australian children? J Paediatr Child Health 1993 Dec: 29: 424–8
Yunginger JW, Reed CE, O’Connell EJ, e t al. A community based study of the epidemiology of asthma. Incidence rates,1964-1983. Am Rev Respir Dis 1992 Oct: 146: 888–94
Peat JK, van der Berg RH, Green WF, et al. Changing prevalence of asthma in Australian children. BMJ 1994 Jun 18: 308: 1591–6
Burr ML, Butland BK, King S, et al. Changes in asthma prevalence: two surveys 15 years apan. Arch Dis Child 1989 Oct: 64: 1452–6
Ayres JG, Noah ND, Fleming DM. Incidence of episodes of acute asthma and acute broochitis in general practice 1976-87. Br J Gen Pract 1993 Sep: 43: 361–4
Anderson HR, Butland BK, Strachan DP. Trends in prevalence and severity of childhood asthma. BMJ 1994 Jun 18; 308: 1600–4
Carlsen K-H. Epidemiology of childhood asthma. Eur Resp Rev 1994 Jan; 4: 5–9
Ehrlich RI, Weinberg EG. Increase in hospital admissions for acute childhood asthma in Cape Town, 1978-1990. S Afr Med J 1994 May: 84: 263–6
Hyndman SJ, Williams DRR, Merrill SL, et al. Rates of admission to hospital for asthma. BMJ 1994 Jun 18: 308: 1596–600
Horwood U, Dawson KP, Mogridge N. Admission patterns for childhood acute asthma: Christchurch 1974-1989. N Z Med J 1991 Jul 10; 104: 277–9
Mackay TW, Wathen CG, Sudlow MF, et al. Factors affecting asthma mortality in Scotland. Scot Med J 1992 Feb: 37: 5–7
Roth A. Hospital admissions of young children for status asthmaticus in Honolulu, Hawaii, 1986 to 1989. Ann Allergy 1993 Dec; 71: 533–6
Robertson CF, Heycock E, Bishop J, et al. Prevalence of asthma in Melboune schoolchildren: changes over 26 years. BMJ 1991 May 11: 302: 1116–8
Priflis K, Anagnostakis J, Harokopos E, et al. Time trends and seasonal variation in hospital admissions for childhood asthma in the Athens region of Greece: 1978-1988. Thorax 1993 Nov; 48: 1168–9
Gerdtham U-G, Hertzman P, Boman G, et al. Impact of inhaled corticosteroids on asthma hospitalization in Sweden: a pooled regression analysis. EFI Research Report, Stockholm School of Economics, October 1993.
Anderson HR. Is asthma really increasing? Paediatr Respir Med 1993; 1: 6–10
Beasley R, Smith K, Pearce N, e t al. Trends in asthma mortality in New zealand, 1908-1986. Med J Aust 1990 Jun 4: 152: 570–3
Campbell DA, McLennan G, Cootes JR, et al. Accuracy of death certificates in South Australia. Med J Aust 1992: 156: 860–3
Weiss KB, Wagener DK. Asthma surveillance in the United States. A review of current trends and knowledge gaps. Chest 1990 Nov; 98 Suppl. 5: 1795–845
Jackson R, Sears MR, Beaglehole R, et al. International trends in asthma mortality: 1970 to 1985. Chest 1988; 94: 914–9
Bauman A, Mitchell CA, Henry RL, et al. Asthma morbidity in Australia: an epidemiological study. Med J Aust 1992 Jun 15; 156: 827–31
Kaplan KM. Epidemiology of deaths from asthma in Pennsylvania, 1978-87. Public Health Rep 1993 Jan-Feb: 108: 66–9
Van den Brink G, Bollen CW, Van den Wall OEM, et al. A drug use review study in patients with obstructive lung disease. Assessment of the quality of drug therapy. Pharm Weekbl Sci 1992 Oct 16; 14: 311–5
Thompson JR, Lambert MA. Chronic persistent asthma presenting to an accident and emergency department compliance with B.T.S. guidelines. Arch Emerg Med 1993 Dec: 10: 347–53
Robertson CF, Rubinfeld AR, Bowes G. Deaths from asthma in Victoria: a 12–month survey. Med J Aust 1990 May 21: 152: 511–7
Fletcher HJ, Ibrahim SA, Speight N. Survey of asthma deaths in the Nottingham region, 1970-85. Arch Dis Child 1990 Feb; 65: 163–7
Neville RG, Clark RC, Hoskins G, et al. National asthma attack audit 1991-2. BMJ 1993 February 27; 306, 559–62
British Thoracic Society. Guidelines for management of asthma. Thorax 1993; 48 Suppl.. 51–524
National Hearth L and BI. International consensus report on diagnosis and treatment of asthma. Eur Respir J 1992; 5: 601–41
Warner JO, Gotz M, Landau KI, et al. Management of asthrna: a consensus statement. Arch Dis Child 1989; 64; 1065–79
Warner JO, Niejens HJ, Landau LI, et al. Asthma: a follow up Statement of an international paediatric asthma consensus group. Arch Dis Child 1992; 67: 240–8
Woolcock A, Rubinfeld AR, Scale JP, et al. Asthma management plan, 1989. Med J Aust 1989; 151; 650–2
Hargreave FE, Dolovich J, Newhouse MT, editors. The assessment and treatment of asthma: a conference report. J Allergy Clin Immunol 1990; 85: 1098–111
Mellis CM, Peat JK, Woolcock AJ, The cost of asthma: Can it be reduced? Pharmacoeconomics 1993 Mar; 3: 205–19
Brogden RN, McTavish D, Budesonide: an updated review of its pharmacological properties, and therapeutic efficacy in asthma and rhinitis. Drugs 1992; 44; 375–407
Barnes PJ, Pedersen S. Efficacy and safety of inhaled corticosteroids in asthma. Am Rev Respir Dis 1993; 148: 51–526
Agertoft L, Pedersen S. Importance of the inhalation device on the effect of budesonide. Arch Dis Child 1993; 69: 130–3
Brambilla C, Lacronique J, Allaert FA, et al. A 3–month comparative dose–reduction study with inhaled beclomethasone dipropionate and budesonide in the management of moderate to severe adult asthma. Drug Invest 1994; 8: 49–56
DeGraaff CS, van den Bergh JAHM, de Bree AF, et al. A double blind clinical comparison of budesonide and beclomethasone dipropionate (BDP) given as dry powder formulations in asthma [abstract]. Eur Respir J 1992; 5 Suppl. 15: 3595
Greefhorst APM. Budesonide and terbutaline delivered via Turbuhaler® compared to BDP and salbutamol delivered via Rotahaler [abstract]. Eur Respir J 1992; 5 Supp1. 15: 3605
Corris PA, Hardy CC, Richardson A, et al. The efficacy and acceptability of two hearth–actuated, multi–dose, dry–powder inhalers in the treatment of chronic asthma. Br J Clin Res 1992; 3; 139–50
Thorsson L, Edsbäcker S, Conradson T-B. Lung deposition of budesonide from Turbuhaler® is twice that from a pressurized metered–dose inhaler P–MDI. Eur Respir J 1994; 7: 1839–44
Selroos O, Backman R, Forsen K-O, et al. Clinical efficacy of budesonide Turbuhaler® compared with that of beclomethasone dipropionate pMDI with volumatic spacer. Allergy 1994; 49: 833–6
Andersson B, Comparative studies of budesonide inhaled by pressurised metered dose inhaler and Turbuhaler® In: Jackson B, editor. Budesonide Turbuhaler®: a workshop report. London: Harwell, 1993: 17–8
Jacobsson L, Lindgren B, Asthma: the economic cost [in Swedish]. Malmö: Lund University; Department of Community Health Services. Health Economics, 1994. Studies in Health Economics 8
Schulz RM, Dye J, Jolicoeur L, et al. Quality–of–life factors for parents of children with asthma. J Asthma 1994 May; 31: 209–19
Taylor WR, Newacheck PW. Impact of childhood asthma on health. Pediatrics 1992 Nov; 90: 657–62
Jones PW. Measurement of health in asthma and chronic obstructive airways disease. Pharm Med 1992 Mar; 6: 13–22
Townsend M, Feeny DH, Guyatt GH, et al. Evaluation of the burden of illness for pediatric asthmatic patients and their parents. Ann Allergy 1991 Oct; 67: 403–8
Ringsberg KC, Wiklund I, Wilhelmsen L. Education of adult patients at an asthmatic school: effects on equality of life knowledge and need for nursing. Eur Rupir J 1990 Jan; 3: 33–7
McSweeny AJ, Heaton RK, Grant I, et al. Chronic obstructive pulmonary disease; socioemotional adjustment and life quality. Chest 1980; 77 Suppl: 309–11
Dean M, Bell E, Kershaw CR, et al. A short exercise and living course for asthmatics. Br J Dis Chest 1988; 82: 155–61
Weiss KB, Sullivan SD. The economic costs of asthma: a review and conceptual model. Pharmacoeconomics 1993 Jul: 4: 14–30
Bryan S, Buxton MJ. Economic evaluation of treatments for respiratory disease. Pharmacoeconomics 1992 Sep; 2: 207–18
Rutten-van Mölken MPMH, Van Doorslaer EKA, Runen FFH. Economic appraisal of asthma and COPD care: a literature review 1980-1991. Soc Sci Med 1992; 35: 161–75
Ädelroth E, Rosenhall L, Glennow C. High dose inhaled budesonide in the treatment of severe: steroid–dependent asthmatics. Allergy 1985; 40: 58–64
Karalus NC, Harrison AC. Inhaled high–dose beclomethasone in chronic asthma. N Z Med J 1987; 100: 305–8
Otulana BA, Varma N, Bullock A, et al. High dose nebulized steroid in the treatment of chronic steroid–dependent asthma. Respir Mod 1992; 86: 105–8
Ädelroth E, Thompson S. Advantages of high–dose inhaled budesonide [letter]. Lancet 1988; 2: 476
Connett GJ, Lenney W, McConchie SM. The cost effectiveness of budesonide in severe asthmatics aged one to three years. Br J Med Econ 1993; 6: 127–34
Rutten-van Molken MPMH, Van DEKA, Jansen MCC. Cost effectiveness of inhaled corticosteroid plus bronchodilator therapy versus bronchodilator monotherapy in children with asthma. Pharmacoeconomics 1993; 4: 257–70
Connett GJ, Warde C, Wooler E, et al. Use of budesonide in severe asthmatics aged 1-3 years. Arch Dis Child 1993 Sep; 69: 351–5
Zbrozek AS. Episode–free days as end–points in economic evaluations of asthma therapy [letter]. Pharmacoeconomics 1994 Jan; 5: 78–9
Stålhammar N-O. The cost per treatment success [letter]. Pharmacoeconomics 1994 Apr: 5: 351-2
Sculpher M, Buxton M. Episode–free days as end–points in economic evaluations of asthma therapy. Reply [Ietter]. Pharmacoeconomics 1994 Jan; 5: 78–9
McCarthy TP, Taylor MD, Richardson PDI. The management of asthma using clinical protocols: is it cost effective, and does it improve patients’ lifestyles? Br J Med Econ 1992; 2: 13–24
Hyland ME. Quality–of–life assessment in respiratory disease. An examination of the content and validity of four questionnaires. Pharmacoeconomics 1992; 2: 43–53
Gay AL, Richardson PDI, Howarth NJ. The influence of budesonide (Pulmicort) on patients’ lifestyle in the management of asthma. Clin Trials J 1989; 26: 175–80
Nankani JN, Northfield M, Beran YM, et al. Changes in asthmatic patients’ symptoms and lifestyles on institution of inhaled budesonide therapy. Curr Med Res Opin 1990; 12 (3): 198–206
Campbell LM, Watson DG, Venables TL, et al. Once daily budesonide Turbohaler® compared with placebo as initial prophylactic therapy for asthma. Br J Clin Res 1991: 2: 111–22
Goren A, Noviski N, Springer C, et al. The ability of young children to use a powder inhalation device (Bricanyl Turbuhaler®) efficiently. Eur Respir J 1991; 4 Suppl. 14: 2425
Duncan J, Ning AC, Crompton GK, Clinical assessment of a new multidose nonpressurised metered–dose–inhaler. Drug Invest 1990: 2: 136–7
Seddon PC, Hear DP. How well do children use dry powder inhalers? Thorn 1990: 45: 818
Hultqvuist C, Ahlström H, Kjellman NHM, et al. A double–blind comparison between a new multi–dose powder (Turbuhaler®) and metered dose inhaler in children with asthma. Allergy 1989: 44: 467–70
Sinninghe Damsté HEJ, Turbuhaler®, a clinical overview. In: Turbuhaler® a non–CFC metered dose inhaler. Report of a symposium held at the 8th Congress of the International society for Aerosols in Medicine, Davos, Switzerland, April 1991. Amsterdam: Excerpta Medica, 1992: 12–3
Engel T, Heinig JH, Malling H-J, et al. Clinical comparison of inhaled budesonide delivered eiher via pressurized metered dose: inhaler or Turbuhaler®, Allergy 1989: 44: 220–5
Ringdal N, Vilsvik JS, Albreksten T. Acceptability of different inhalation systems: metered dose inhaler (MDl) and multiple dose powder inhaler (MDPI) [abstract]. Eur Respir J 1990; 3 Suppl.10: 4175
Anani A, Higgins AJ, Crompton GK. Breath–actuated inhalers: comparison of terbutaline Turbohaler® with salbutamoI Rotahaler®. Eur Respir J 1989: 2: 640–2
Tjwa MKT, Bindels H. Budesonide Turbuhaler® versus beclomethasone dipropionate Rotahaler®; their effects on PC20–histamine, FEV 1 and symptoms [abstract]. Eur Respir J 1990: 3 Suppl. 10: 499
Petrie GR, Choo-Kang YFJ, Clark RA, et al. An assessment of the acceptability of two breath–actuated conicosteroid inhalers:comparison of Turbohaler® with Diskhaler®. Drug Invest 1990: 2: 129–31
Jones AH, Langdon CG, Lee PS, et al. Pulmicort Turbohaler® once daily as initial prophylactic therapy for asthma. Respir Mcd 1994: 88: 293–9
Waalkens HJ, Van Essen-Zandvliet EE, Hughes MD, et al. Cessation of long–term treatment with inhaled conicosteroid (budesonide) in children with asthma results in deterioration. Am Rev Respir Dis 1993: 148: 1252–7
Kraan J, Kaeter GH, Van der Mark TW, et al. Changes in bronchial hyperreactivity induced by 4 weeks treatment with antihistaminic drugs in patients with alIergic asthma: a comparison between budesonide and terbutaline. J Allergy Clin Immunol 1985: 76: 628–36
Vathenen AS, Knox AJ, Wisniewski A, et al. Time course of change in bronchial reactivity with an inhaled corticosteroid in asthma. Am Rev Respir Dis 1991: 143: 1317–21
Bel EH, Timmers MC, Zwinderman AH, et al. The effect of inhaled conicosteroids on the maximal degree of airway narrowing to methacholine in asthmatic subjects. Am Rev Respir Dis 1991: 143: 109–13
Dutoit JI, Salome CM, Woolcock AJ, Inhaled corticosteroids reduce the severity of bronchial hyperresponsiveness in asthma but oral theophylline does not. Am Rev Respir Dis 1987: 136: 1174–8
Svendsen UG, Frolund L, Madsen F, et al. A comparison of the effects of nedocromil sodium and beclomehtasone dipropionate on pulmonary function, symptoms, and bronchial responsiveness in patients with asthma. J Allergy Clin Immunol 1989; 84: 224–31
Haahtela T, Järvinen M, Kava T. et aI. Effects of reducing or discontinuing inhaled budesonide in patients with mild asthma. N Engl J Med 1994; 331: 700–5
Barnes PJ, Fan Chung K. Difficult asthma. BMJ 1989: 299: 695–8
Worth H. Patient education in aduIt asthmatics. Lung 1990: 1 Suppl.: 463–8
Brewis RAL. Patient education self–management plans and peak flow measurement. Respir Med 1991; 85: 457–62
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: U.C. Gerdtham, Center for Health Economics, Stockholm, Sweden; M.E. Hyland, Department of Psychology, University of Plymouth, Plymouth, England; M. Krahn, Department of Medicine, Toronto Hospital, Toronto, Ontario, Canada; C.M. Mellis, Department of Respiratory Medicine, Royal Alexandra Hospital for Children, Camperdown, New South Wales, Australia; M. Rutten, Department of Health Economics, University of Limburg, Maastricht, The Netherlands; M.J. Schulpher, Health Economics Research Group, Brunei University. Uxbridge. England; S.D. Sullivan, Departments of Pharmacy and Health Services, University of Washington, Seattle, Washington, USA; C. Trautner, Department of Biometrics and Epidemiology, Diabetes Research Institute at Düsseldorf, Düsseldorf, Germany; K.B. Weiss, Center for Health Services Research, Rush Primary Care Institute, Chicago, Illinois, USA; A.S. Zbrozek, Office of Clinical Economics, University of Texas Medical Branch, Galveston, Texas, USA.
Rights and permissions
About this article
Cite this article
Davis, R., McTavish, D. Budesonide. Pharmacoeconomics 7, 457–470 (1995). https://doi.org/10.2165/00019053-199507050-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-199507050-00009