Summary
Abstract
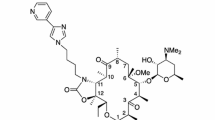
Azithromycin is a macrolide antibacterial agent. The novel microspheres oral extended-release formulation (Zmax™) is the first antibacterial drug approved in the US for administration as a single dose in adult patients with mild to moderate acute bacterial sinusitis (ABS) or community-acquired pneumonia (CAP). It has a broad spectrum of in vitro antibacterial activity against Gram-positive, Gram-negative and atypical pathogens that cause ABS and CAP infections (including Streptococcus pneumoniae), and achieves good tissue penetration. Azithromycin extended release is an effective and generally well tolerated treatment in patients with ABS or CAP. The clinical cure rates of a single 2.0g dose of azithromycin extended release were noninferior to those obtained with a 10-day regimen of levofloxacin in patients with ABS, and with 7-day regimens of clarithromycin extended release or levofloxacin in patients with CAP. With a pharmacodynamic and pharmacokinetic profile well suited to administration as a single-dose regimen that may offer the advantage of improved compliance and convenience compared with once-daily longer-course regimens, azithromycin extended release is a new option in the empirical treatment of adult patients with mild or moderate ABS or CAP in the US.
Pharmacological Properties
Azithromycin inhibits microbial protein synthesis. In North American surveillance studies, azithromycin showed variable in vitro bacteriostatic activity against clinical isolates of S. pneumoniae and good activity against those of Haemophilus influenzae and Moraxella catarrhalis. Azithromycin also demonstrated good activity against selected strains and/or clinical isolates of Chlamydophila pneumoniae and Mycoplasma pneumoniae. In time-kill studies azithromycin demonstrated bactericidal activity against selected strains and/or clinical isolates of M. catarrahlis, S. pneumoniae and H. influenzae, and a prolonged post-antibiotic effect against the latter two pathogens.
Recent surveillance studies indicate that rates of resistance to azithromycin are similar to those of other macrolides in clinical isolates of S. pneumoniae (≈28–30%) and have been stable in recent years. There was a high level of co-resistance between penicillin- and azithromycin-resistant S. pneumoniae isolates. However, susceptibility of clinical isolates of H. influenzae to azithromycin is generally very high (≈99%).
In animal models of S. pneumoniae infection, the pharmacokinetic/pharmacodynamic parameter best predictive of azithromycin clinical efficacy was the area under the concentration-time curve from time zero to 24 hours to minimum drug inhibitory concentration ratio (AUC24: MIC ratio), and the curative effect of oral azithromycin administered as a single dose or a simulated extended-release dose was generally superior to that of once-daily 2- to 5-day regimens of the drug.
The microsphere extended-release formulation of azithromycin is a powder reconstituted with water for oral administration as a single 2.0g dose. Sustained release of the drug is achieved via diffusion from the microspheres, with the majority of the administered dose released in the lower gastrointestinal tract. Time to peak serum concentration is 5 hours. Azithromycin extended release is well absorbed; the mean maximum serum concentration is 0.82 µg/mL and the AUC24 is about 8.62 µg · h/mL. Absorption of azithromycin extended release 2.0g was greater in the fed than in the fasted state; thus, azithromycin extended release should be taken on an empty stomach to ensure slower absorption. Azithromycin is excreted predominantly as unchanged drug in the faeces. The terminal elimination half-life of azithromycin extended release is 59 hours.
A single 2.0g dose of azithromycin extended release is not pharmacokinetically bioequivalent to, or interchangeable with, the immediate-release oral formulations (tablets or powder for oral suspension) of azithromycin. Azithromycin extended release achieves higher intracellular concentrations in mononuclear and polymorphonuclear leukocyte and alveolar cells, and higher tissue/fluid concentrations in lung serum, lung tissue and lung epithelial lining fluid than in serum. Moreover, azithromycin concentrations in these compartments were generally greater than those achieved with the immediate-release formulation.
Therapeutic Use
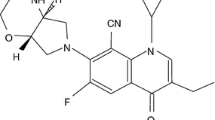
In three phase III non-inferiority trials (n = 427–538), a single 2.0g dose of oral azithromycin extended release was no less effective in producing a clinical cure at the test of cure visit (primary efficacy endpoint) in adult patients with ABS than a 10-day regimen of oral levofloxacin 500mg once daily, or in adult patients with mild to moderate CAP than 7-day regimens of oral levofloxacin 500mg once daily or oral clarithromycin extended release 1.0g once daily.
Azithromycin extended release and comparator antibacterial agents all demonstrated clinical efficacy against the most common causative pathogens isolated from patients at baseline, including S. pneumoniae, H. influenzae and M. catarrhalis. In the trials in patients with CAP, 91–92% of patients receiving azithromycin extended release, levofloxacin or clarithromycin extended release experienced a bacteriological response (presumed or assessed via eradication).
Tolerability
A single 2.0g dose of azithromycin extended release was generally well tolerated in adult patients with ABS or mild to moderate CAP, with the majority of adverse events being of mild to moderate severity. The most frequent treatment-related adverse event was diarrhoea/loose stools. In trials in patients with CAP, the incidence of treatment-related adverse events in patients receiving azithromycin extended release was significantly higher than in those receiving levofloxacin, but did not differ from that in recipients of clarithromycin extended release. Serious adverse events and rates of discontinuation from treatment because of an adverse event were infrequent with azithromycin extended release or comparator agents.






Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Peters DH, Friedel HA, McTavish D. Azithromycin: a review of its antimicrobial activity, pharmacokinetic properties and clinical efficacy. Drugs 1992; 44 (5): 750–99
Gunasekara NS, Barman Balfour JA. Management of community-acquired pneumonia: defining the role of azithromycin. Dis Manage Health Outcomes 1999 Jan; 5: 41–54
Dunn CJ, Barradell LB. Azithromycin: a review of its pharmacological properties and use as 3-day therapy in respiratory tract infections. Drugs 1996; 51 (3): 483–505
Langtry HD, Balfour JA. Azithromycin: a review of its use in paediatric infectious diseases [published erratum appears in Drugs 1998; 56 (2): 1046]. Drugs 1998 Aug; 56: 273–97
Pfizer Inc. Pfizer’s Zithromax receives FDA approval as a once-daily, three-day treatment for acute bacterial sinusitis [online]. Available from URL: http://www.pfizer.com [Accessed 2006 Feb 15]
Pfizer Inc. Zmax™ (azithromycin extended release) for oral suspension [online]. Available from URL: http://www.pfizer.com [Accessed 2006 Feb 15]
Drehobl MA, De Salvo MC, Lewis DE, et al. Single-dose azithromycin microspheres vs clarithromycin extended release for the treatment of mild-to-moderate community-acquired pneumonia in adults. Chest 2005 Oct; 128 (4): 2230–7
D’Ignazio J, Camere MA, Lewis DE, et al. Novel, single-dose microsphere formulation of azithromycin versus 7-day levofloxacin therapy for treatment of mild to moderate community-acquired pneumonia in adults. Antimicrob Agents Chemother 2005 Oct; 49 (10): 4035–41
Pfizer Inc. Zithromax® (azithromycin tablets) and (azithromycin for oral suspension) [online]. Available from URL: http://www.pfizer.com [Accessed 2006 Feb 15]
Blondeau JM. A review of the comparative in-vitro activities of 12 antimicrobial agents, with a focus on five new ‘respiratory quinolones’. J Antimicrob Chemother 1999; 43 Suppl. B: 1–11
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; sixteenth informational supplement. CLSI document M100-S16 [ISBN 1-56238-588-7]. Wayne (PA): Clinical and Laboratory Standards Institute, 2006 Jan
Roblin PM, Kutlin A, Reznik T, et al. In vitro activity of grepafloxacin, levofloxacin, moxifloxacin, trovafloxacin, clarithromycin, and azithromycin against recent clinical isolates of Chlamydia pneumoniae [abstract no. a-94]. 99th General Meeting American Society for Microbiology; 1999 May 30–Jun 3; Chicago (IL), 20
Waites KB, Crabb DM, Duffy LB. Comparative in vitro susceptibilities and bactericidal activities of investigational fluoroquinolone ABT-492 and other antimicrobial agents against human mycoplasmas and ureaplasmas. Antimicrob Agents Chemother 2003 Dec; 47 (12): 3973–5
Jacobs MR, Felmingham D, Appelbaum PC, et al. The Alexander Project 1998–2000: susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother 2003; 52: 229–46
Hoban DJ, Doern GV, Fluit AC, et al. Worldwide prevalence of antimicrobial resistance in Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis in the SENTRY antimicrobial surveillance program, 1997–1999. Clin Infect Dis 2001; 32 Suppl. 2: S81–93
Johnson DM, Sader HS, Fritsche TR, et al. Susceptibility trends of Haemophilus influenzae and Moraxella catarrhalis against orally administered antimicrobial agents: five-year report from the SENTRY antimicrobial surveillance program. Diagn Microbiol Infect Dis 2003; 47: 373–6
Hoban D, Waites K, Felmingham D. Antimicrobial susceptibility of community-acquired respiratory tract pathogens in North America in 1999–2000: findings of the PROTEKT surveillance study. Diagn Microbiol Infect Dis 2003; 45: 251–9
Jenkins SG, Farrell DJ, Patel M, et al. Trends in anti-bacterial resistance among Streptococcus pneumoniae isolated in the USA, 2000–2003: PROTEKT US years 1–3. J Infect 2005; 51: 355–63
Brown SD, Rybak MJ. Antimicrobial susceptibility of Streptococcus pneumoniae, Streptococcus pyogenes and Haemophilus influenzae collected from patients across the USA, in 2001–2002, as part of the PROTEKT US study. J Antimicrob Chemother 2004; 54 Suppl. 1: i7–15
Doern GV, Brown SD. Antimicrobial susceptibility among community-acquired respiratory tract pathogens in the USA: data from PROTEKT US 2000–01. J Infect 2004; 48: 56–65
Felmingham D, Reinert RR, Hirakata Y, et al. Increasing prevalence of antimicrobial resistance among isolates of Streptococcus pneumoniae from the PROTEKT surveillance study, and comparative in vitro activity of the ketolide, telithromycin. J Antimicrob Chemother 2002; 50 Suppl. 1: 25–37
Karlowsky JA, Thornsberry C, Jones ME, et al. Factors associated with relative rates of antimicrobial resistance among Streptococcus pneumoniae in the United States: results from the TRUST surveillance program (1998–2002). Clin Infect Dis 2003; 36: 963–70
Thornsberry C, Sahm DF, Kelly LJ, et al. Regional trends in antimicrobial resistance among clinical isolates of Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis in the United States: results from the TRUST surveillance program, 1999–2000. Clin Infect Dis 2002; 34 Suppl. 1: S4–16
Thornsberry C, Jones ME, Hickey ML, et al. Resistance surveillance of Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis isolated in the United States, 1997–1998. J Antimicrob Chemother 1999; 44: 749–59
Sahm DF. Resistance issues and community-acquired respiratory infections. Clinical Cornerstone 2003; Suppl. 3: S4–11
Zhanel GG, Palatnick L, Nichol KA, et al. Antimicrobial resistance in respiratory tract Streptococcus pneumoniae isolates: results of the Canadian Respiratory Organism Susceptibility Study, 1997 to 2002. Antimicrob Agents Chemother 2003 Jun; 47 (6): 1867–74
Zhanel GG, Palatnick L, Nichol KA, et al. Antimicrobial resistance in Haemophilus influenzae and Moraxella catarrhalis respiratory tract isolates: results of the Canadian Respiratory Organism Susceptibility Study, 1997 to 2002. Antimicrob Agents Chemother 2003 Jun; 47 (6): 1875–81
Roblin PM, Kutlin A, Hammerschlag MR. In vitro activity of trovafloxacin against Chlamydia pneumoniae. Antimicrob Agents Chemother 1997 Sep; 41 (9): 2033–4
Roblin PM, Hammerschlag MR. In vitro activity of a new ketolide antibiotic, HMR 3647, against Chlamydia pneumoniae. Antimicrob Agents Chemother 1998 Jun; 42 (6): 1515–6
Roblin PM, Reznik T, Kutlin A, et al. In vitro activities of rifamycin derivatives ABI-1648 (Rifalazil, KRM-1648), ABI-1657, and ABI-1131 against Chlamydia trachomatis and recent clinical isolates of Chlamydia pneumoniae. Antimicrob Agents Chemother 2003 Mar; 47 (3): 1135–6
Kohlhoff SA, Roblin PM, Reznik T, et al. In vitro activity of a novel diaminopyrimidine compound, iclaprim, against Chlamydia trachomatis and C. pneumoniae. Antimicrob Agents Chemother 2004 May; 48 (5): 1885–6
Strigl S, Roblin PM, Reznik T, et al. In vitro activity of ABT 773, a new ketolide antibiotic, against Chlamydia pneumoniae. Antimicrob Agents Chemother 2000 Apr; 44 (4): 1112–3
Waites KB, Reddy NB, Crabb DM, et al. Comparative in vitro activities of investigational peptide deformylase inhibitor NVP LBM-415 and other agents against human mycoplasmas and ureaplasmas. Antimicrob Agents Chemother 2005 Jun; 49 (6): 2541–2
Pankuch G, Appelbaum PC. Post-antibiotic effects of LBM415 and other agents against S. pneumoniae and H. influenzae [abstract no. A-1833]. 45th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2005 Dec 16–19; Washington DC, 32
Browne FA, Bozdogan B, Clark C, et al. Antipneumococcal activity of DK-507K, a new quinolone, compared with the activities of 10 other agents. Antimicrob Agents Chemother 2003 Dec; 47 (12): 3815–24
Matic V, Kosowska K, Bozdogan B, et al. Antipneumococcal activities of two novel macrolides, GW 773546 and GW 708408, compared with those of erythromycin, azithromycin, clarithromycin, clindamycin, and telithromycin. Antimicrob Agents Chemother 2004 Nov; 48 (11): 4103–12
Davies TA, Ednie LM, Hoellman DM, et al. Antipneumococcal activity of ABT-773 compared to those of 10 other agents. Antimicrob Agents Chemother 2000 Jul; 44 (7): 1894–9
Credito KL, Lin G., Pankuch GA, et al. Susceptibilities of Haemophilus influenzae and Moraxella catarrhalis to ABT-773 compared to their susceptibilities to 11 other agents. Antimicrob Agents Chemother 2001 Jan; 45 (1): 67–72
Bergman KL, Olsen KM, Peddicord TE, et al. Antimicrobial activities and postantibiotic effects of clarithromycin, 14-hydroxy-clarithromycin, and azithromycin in epithelial cell lining fluid against clinical isolates of Haemophilus influenzae and Streptococcus pneumoniae. Antimicrob Agents Chemother 1999 May; 43: 1291–3
Pankuch G, Lin G, Appelbaum PC. Time-kill activities of ceftobiprole and eight other agents against H. influenzae and M. catarrhalis [abstract no. E-305]. 45th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2005 Dec 16–19; Washington DC, 157
Kosowska K, Credito K, Pankuch GA, et al. Activities of two novel macrolides, GW 773546 and GW 708408 compared with those of telithromycin, erythromycin, azithromycin, and clarithromycin against Haemophilus influenzae. Antimicrob Agents Chemother 2004 Nov; 48 (11): 4113–9
Klugman KP, Lonks JR. Hidden epidemic of macrolide-resistant pneumococci. Emerg Infect Dis 2005 Jun; 11 (6): 802–7
Garau J. The hidden impact of antibacterial resistance in respiratory tract infection. Clinical failures: the tip of the iceberg? Respir Med 2001 Jun; 95 Suppl. A: S5–11
Lonks JR, Garau J, Gomez L, et al. Failure of macrolide antibiotic treatment in patients with bacteremia due to erythromycin-resistant Streptococcus pneumoniae. Clin Infect Dis 2002 Sep 1; 35 (5): 556–64
Waterer GW, Wunderink RG, Jones CB. Fatal pneumococcal pneumonia attributed to macrolide resistance and azithromycin monotherapy [letter]. Chest 2000 Dec; 118 (6): 1839–40
Kelley MA, Weber DJ, Gilligan P, et al. Breakthrough pneumococcal bacteremia in patients being treated with azithromycin and clarithromycin. Clin Infect Dis 2000 Oct; 31 (4): 1008–11
Fogarty C, Goldschmidt R, Bush K. Bacteremic pneumonia due to multidrug-resistant pneumococci in 3 patients treated unsuccessfully with azithromycin and successfully with levofloxacin. Clin Infect Dis 2000 Aug; 31 (2): 613–5
Peric M, Bozdogan B, Jacobs MR, et al. Effects of an efflux mechanism and ribosomal mutations on macrolide susceptibility of Haemophilus influenzae clinical isolates. Antimicrob Agents Chemother 2003 Mar; 47 (3): 1017–22
Jacobs MR. Streptococcus pneumoniae: epidemiology and patterns of resistance. Am J Med 2004 Aug 2; 117 Suppl. 3A: 3–15S
Farrell DJ, Jenkins SG, Brown SD, et al. Emergence and spread of Streptococcus pneumoniae with erm(B) and mef(A) resistance. Emerg Infect Dis 2005 Jun; 11 (6): 851–8
Farrell DJ, Jenkins SG. Distribution across the USA of macrolide resistance and macrolide resistance mechanisms among Streptococcus pneumoniae isolates collected from patients with respiratory tract infections: PROTEKT US 2001–2002. J Antimicrob Chemother 2004 Aug; 54 Suppl. 1: i17–22
Farrell DJ, Jenkins SG, Patel M, et al. Antimicrobial resistance patterns among Streptococcus pneumoniae isolated from elderly patients: data from the PROTEKT U.S. study years 1–4 [abstract no. C2-231]. 45th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2005 Dec 16–19; Washington DC, 91
Wierzbowski AK, Swedlow D, Nichol K, et al. Molecular characterization of macrolide resistant Streptococcus pneumoniae isolates containing both erm(B) and mef(A) genes isolated during 1997–2004 Canadian Respiratory Organism Susceptibility Study (CROSS) [abstract no. C2-235]. 45th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2005 Dec 16–19; Washington DC, 92
Pankuch GA, Jueneman SA, Davies TA, et al. In vitro selection of resistance to four beta-lactams and azithromycin in Streptococcus pneumoniae. Antimicrob Agents Chemother 1998 Nov; 42 (11): 2914–8
Davies TA, Dewasse BE, Jacobs MR, et al. In vitro development of resistance to telithromycin (HMR 3647), four macrolides, clindamycin, and pristinamycin in Streptococcus pneumoniae. Antimicrob Agents Chemother 2000 Feb; 44 (2): 414–7
Sahm DF, Weaver MK, Flamm RK, et al. Rates of antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States: results from the TRUST 7 (2002–2003) Surveillance Study [abstract no. 201 plus poster]. 41st Annual Meeting of the Infectious Diseases Society of America; 2003 9–12 Oct; San Diego (CA), 63
Felmingham D. Comparative antimicrobial susceptibility of respiratory tract pathogens. Chemotherapy 2004; 50 Suppl. 1: 3–10
Murray JJ, Emparanza P, Lesinskas E, et al. Efficacy and safety of a novel, single-dose azithromycin microsphere formulation versus 10 days of levofloxacin for the treatment of acute bacterial sinusitis in adults. Otolaryngol Head Neck Surg 2005 Aug; 133 (2): 194–200
Rothermel CD. Single-dose azithromycin for acute otitis media: a pharmacokinetic/pharmacodynamic rationale. Curr Ther Res Clin Exp 2003; 64 Suppl. A: A4–15
Craig WA, Kiem S, Andes DR, et al. Free drug 24-hr AUC/MIC is the PK/PD target that correlates with in vivo efficacy of macrolides, azalides, ketolides and clindamycin [abstract no. A-1264]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA), 14
Girard D, Finegan SM, Dunne MW, et al. Enhanced efficacy of single-dose versus multi-dose azithromycin regiments in preclinical infection models. J Antimicrob Chemother 2005; 56: 365–71
Abbott Laboratories. Biaxin® Filmtab® (clarithromycin tablets, USP) Biaxin® XL Filmtab® (clarithromycin extended-release tablets) Biaxin® Granules (clarithromycin for oral suspension, USP) [online]. Available from URL: http://www.rxabbott.com [Accessed 2006 Feb 14]
Anon JB, Jacobs MR, Poole MD, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis [published erratum appears in Otolaryngol Head Neck Surg 2004; 130 (6): 794-6]. Otolaryngol Head Neck Surg 2004 Jan; 130 (1 Suppl.): 1–45
Retsema JA. Susceptibility and resistance emergence studies with macrolides. Int J Antimicrob Agents 1999 Mar; 11 Suppl. 1: S15–21
Matute AJ, Schurink CA, Krijnen RM, et al. Double-blind, placebo-controlled study comparing the effect of azithromycin with clarithromycin on oropharyngeal and bowel microflora in volunteers. Eur J Clin Microbiol Infect Dis 2002 Jun; 21 (6): 427–31
Kamicker BJ, Bertsche CD, Medina IA. In rodent models a single dose of azithromycin was more effective than dosing split over 3 or 5 days [poster]. 44th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2004 Oct 30–Nov 2; Washington DC
Liu P, Allaudeen H, Chandra R, et al. Serum and white blood cell (WBC) pharmacokinetics (PK) of a novel, single-dose azithromycin (AZ) microsphere formulation [abstract no. A-23]. 45th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2005 Dec 16–19; Washington DC, 5
Danesi R, Lucchi M, Pasqualetti G, et al. Single-dose azithromycin microspheres (AZ-M) achieves improved lung pharmacokinetics versus azithromycin tablets (AZ-IR) [poster #A62]. 102nd International Conference of the American Thoracic Society; 2006 19–24 May; San Diego (CA), A150
Breen J, Chandra R, Herbig S, et al. Zmax: A novel microsphere-based azithromycin dosage form [poster]. American Association of Pharmaceutical Scientists Annual Meeting and Exposition; 2005 Nov 6–10; Nashville (TN)
Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336: 243–50
Marple BF. Editorial commentary: Dilemma in trial design: do current study designs adequately evaluate effectiveness antibiotic in ABRS? Otolaryngol Head Neck Surg 2005 Aug; 133 (2): 200–1
Piccirillo JF. Clinical practice. Acute bacterial sinusitis. N Engl J Med 2004 Aug 26; 351 (9): 902–10
Niederman MS, Mandell LA, Anzueto A, et al. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 2001 Jun; 163 (7): 1730–54
National Institute of Allergy and Infectious Diseases. Sinusitis [online]. Available from URL: http://www.niaid.nih.gov/factsheets/sinusitis.htm [Accessed 2006 Feb 13]
Thibodeau KP, Viera AJ. Atypical pathogens and challenges in community-acquired pneumonia. Am Fam Physician 2004 Apr 1; 69 (7): 1699–706
National Institute of Allergy and Infectious Diseases. Pneumococcal pneumonia [online]. Available from URL: http://www.niaid.nih.gov/factsheets/pneumonia.htm [Accessed 2006 Feb 13]
Niederman MS. Review of treatment guidelines for community-acquired pneumonia. Am J Med 2004 Aug 2; 117 Suppl. 3A: 51–7S
Hickner JM, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for acute rhinosinusitis in adults: background. Ann Intern Med 2001; 134: 498–505
Snow V, Mottur-Pilson C, Hickner JM. Principles of appropriate antibiotic use for acute sinusitis in adults. Ann Intern Med 2001; 134: 495–7
Lutfiyya MN, Henley E, Chang LF, et al. Diagnosis and treatment of community-acquired pneumonia. Am Fam Physician 2006; 73: 442–50
Mandell LA, Bartlett JG, Dowell SF, et al. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis 2003 Dec 1; 37 (11): 1405–33
Doern GV. Antimicrobial use and the emergence of antimicrobial resistance with Streptococcus pneumoniae in the United States. Clin Infect Dis 2001 Sep 15; 33 Suppl. 3: S187–92
Edelstein PH. Predicting the emergence of antimicrobial resistance [letter]. Clin Infect Dis 2002 May 15; 34 (10): 1418; author reply 1418-9
Pfizer Inc. Pfizer’s single-dose antibiotic Zmax receives FDA approval [online]. Available from URL: http://www.zmaxinfo.com [Accessed 2006 Mar 30]
Ortho-McNeil Pharmaceutical Inc. Levaquin® (levofloxacin) tablets Levaquin® (levofloxaxin) oral solution Levaquin® (levlofloxacin) injection Levaquin® (levafloxacin in 5% dextrose) injection Prescribing Information [online]. Available from URL: http://www.levaquin.com [Accessed 2006 Jun 8]
Sorensen SV, Baker TM, Mallya UG, et al. Pharmacoeconomic evaluation of single dose azithromycin extended release for the treatment of community-acquired pneumonia [abstract no. CE1]. Value Health 2006 May 30; 9 (3): 7
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: M.C. De Salvo, Hospital Enrique Tornú, Buenos Aires, Argentina; H. Lode, Krankenhaus Zehlendorf/Heckeshorn, Freie Universitat Berlin, Berlin, Germany; M.N. Lutfiyya, Department of Family and Community Medicine, University of Illinois College of Medicine at Rockford, Rockford, Illinois, USA; A.P. MacGowan, Department of Microbiology, Southmead Health Services NHS Trust, Bristol Centre for Antimicrobial Research and Evaluation, Bristol, England; C.E. Nord, Karolinska Institute, Division of Clinical Bacteriology, Hudding University Hospital, Stockholm, Sweden; V. Snow, Clinical Programs and Quality of Care, American College of Physicians, Philadelphia, Pennsylvania, USA.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘azithromycin’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Wolters Kluwer Health | Adis). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE, EMBASE and Adisbase search terms were ‘azithromycin’ and ‘microspheres’. Searches were last updated 9 February 2007.
Selection: Studies in patients with acute bacterial sinusitis or community-acquired pneumonia who received azithromycin microspheres. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Azithromycin microspheres, antibacterials, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
Harrison, T.S., Keam, S.J. Azithromycin Extended Release. Drugs 67, 773–792 (2007). https://doi.org/10.2165/00003495-200767050-00010
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200767050-00010