Summary
Abstract
Agalsidase beta (Fabrazyme®) is a recombinant human α-galactosidase A enzyme approved for intravenous use in the treatment of Fabry disease. Fabry disease is a progressive, multisystemic, potentially life threatening disorder caused by a deficiency of α-galactosidase A. This deficiency results in accumulation of glycosphingolipids, particularly globotriaosylceramide (GL-3), in the lysosomes of various tissues. This accumulation is the underlying driver of disease progression. Agalsidase beta provides an exogenous source of α-galactosidase A.
Intravenous agalsidase beta is effective and well tolerated in patients with Fabry disease. In a phase III trial, agalsidase beta was shown to clear GL-3 from various target cells and, in a subsequent extension of this trial, prevent GL-3 reaccumulation. In a post-approval trial, agalsidase beta was shown to provide significant clinical benefit by reducing the risk of a major clinical event. Thus, agalsidase beta represents an important advance in the treatment of Fabry disease, and agalsidase beta therapy should be strongly considered in patients with Fabry disease who are suitable candidates.
Pharmacological Properties
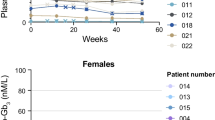
The amino acid sequence of agalsidase beta is the same as that of native α-galactosidase A. Agalsidase beta is taken up (via receptor-mediated endocytosis) by vascular endothelial and parenchymal cells into lysosomes, where it catalyses the hydrolysis of GL-3 (and other glycosphingolipids) to ceramide dihexoside and galactose. Intravenous agalsidase beta reduced plasma GL-3 levels (measured by ELISA) in a rapid, dose-dependent manner in a dose-ranging study in 15 men with classic Fabry disease. Two of three patients receiving agalsidase beta 1 mg/kg every other week (i.e. bi-weekly) [the recommended regimen] had undetectable GL-3 levels (i.e. <1.2 ng/μL) after the first infusion. GL-3 clearance from tissues was generally also dose dependent.
Mean plasma concentrations reached 80% of the peak concentration 90 minutes into the infusion with intravenous agalsidase beta 1 mg/kg with an area under the plasma concentration-time curve of =500 μg · min/mL. Agalsidase beta is thought to be metabolically degraded via peptide hydrolysis and is cleared from the circulation by both saturable and nonsaturable pathways. The terminal elimination half-life was 45–102 minutes.
Therapeutic Efficacy
The efficacy of intravenous agalsidase beta 1 mg/kg bi-weekly has been evaluated in Fabry disease in randomised, double-blind, placebo-controlled, multicentre, phase III (n = 58) and post-approval (n = 82) trials.
Agalsidase beta cleared GL-3 from the renal microvascular endothelium in patients with classic Fabry disease in the pivotal phase III trial. Kidney specimens revealed that at week 20, significantly more agalsidase beta than placebo recipients were free of microvascular endothelial GL-3 deposits (69% vs 0% had a score of 0) [primary endpoint]. Heart and skin specimens were free of microvascular endothelial GL-3 deposits in 72% and 100% of agalsidase beta recipients versus 3% and 3% of placebo recipients. At week 20, significant improvements from baseline in the McGill Pain Questionnaire score and aspects of health-related quality of life (HR-QOL) were seen in both agalsidase beta and placebo recipients.
At the end of the 20-week double-blind treatment period, patients continued in an extension phase during which all patients received intravenous agalsidase beta 1 mg/kg bi-weekly. Agalsidase beta further reduced GL-3 deposits, and prevented their reaccumulation, in the longer term. Renal function was stable throughout 54 months of open-label treatment with agalsidase beta in all but six patients.
In the pivotal post-approval trial, the risk of a clinically significant renal, cardiac or cerebrovascular event or death (primary endpoint) in the per-protocol analysis (n = 74) was significantly reduced by 61%, after adjustment for baseline proteinuria, with intravenous agalsidase beta 1 mg/kg bi-weekly versus placebo (median duration of treatment 18.5 months; patients had advanced Fabry disease and mild to moderate renal impairment at baseline). Indeed, the extent of proteinuria at baseline appeared to predict the risk of patients experiencing a clinically significant event.
Clinical benefits were also seen with agalsidase beta therapy in several noncomparative trials in patients with Fabry disease. Agalsidase beta was effective in paediatric patients and Japanese patients with Fabry disease, improved left ventricular (LV) hypertrophy and aspects of LV function in patients with Fabry cardiomyopathy, and improved small nerve fibre function in patients with Fabry neuropathy. In addition, renal function remained stable, gastrointestinal and other symptoms were ameliorated and improvements in HR-QOL were seen.
Tolerability
Intravenous agalsidase beta 1 mg/kg bi-weekly was reasonably well tolerated in patients with Fabry disease in the well designed phase III and post-approval trials. In the post-approval trial, mild to moderate infusion-related reactions (most commonly rigors and fever) occurred in 55% of agalsidase beta recipients and 23% of placebo recipients. In the phase III trial, transient infusion-related reactions of mild to moderate intensity occurred in 59% of patients during the double-blind and initial 6-month open-label treatment periods; these reactions were controlled by reducing the infusion rate and/or administering preventive medications. The initial infusion reaction often coincided with seroconversion and the frequency of infusion reactions decreased with continued use of agalsidase beta. During the 20-week double-blind treatment period of the phase III trial, agalsidase beta recipients were significantly more likely than placebo recipients to experience treatment-related rigors and fever. By month 54 of the extension study, IgG seroconversion had occurred in 90% of agalsidase beta recipients. Over time, nine patients who seroconverted tolerised, and antibody titres decreased at least 4-fold in 32 patients. Seroconversion did not appear to have an impact on efficacy in the pivotal phase III trial or during the 54-month open-label extension phase.





Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Desnick RJ, Brady R, Barranger J, et al. Fabry disease, an under-recognized multisystemic disorder: expert recommendations for diagnosis, management, and enzyme replacement therapy. Ann Intern Med 2003 Feb 18; 138 (4): 338–46
Hopkin RJ, Bissler J, Grabowski GA. Comparative evaluation of α-galactosidase A infusions for treatment of Fabry disease. Genet Med 2003 May/Jun 30; 5 (3): 144–53
MacDermot KD, Holmes A, Miners AH. Anderson-Fabry disease: clinical manifestations and impact of disease in a cohort of 60 obligate carrier females. J Med Genet 2001; 38: 769–807
MacDermot KD, Holmes A, Miners AH. Anderson-Fabry disease: clinical manifestations and impact of disease in a cohort of 98 hemizygous males. J Med Genet 2001; 38: 750–60
Lee K, Jin X, Zhang K, et al. A biochemical and pharmacological comparison of enzyme replacement therapies for the glycolipid storage disorder Fabry disease. Glycobiology 2003 Apr; 13 (4): 305–13
Genzyme Corporation. Fabrazyme® (agalsidase beta) for intravenous infusion: prescribing information [online]. Available from URL: http://www.fabrazyme.com [Accessed 2005 Oct 5]
European Medicines Agency. Fabrazyme: summary of product characteristics [online]. Available from URL: http://www.emea.eu.int [Accessed 2007 Jan 3]
Ioannou YA, Zeidner KM, Gordon RE, et al. Fabry disease: preclinical studies demonstrate the effectiveness of α-galactosidase A replacement in enzyme-deficient mice. Am J Hum Genet 2001; 68: 14–25
Blom D, Speijer D, Linthorst GE, et al. Recombinant enzyme therapy for Fabry disease: absence of editing of human α-galactosidase A mRNA. Am J Hum Genet 2003 Jan; 72 (1): 23–31
Eng CM, Banikazemi M, Gordon RE, et al. A phase 1/2 clinical trial of enzyme replacement in Fabry disease: pharmacokinetic, substrate clearance, and safety studies. Am J Hum Genet 2001 Mar; 68 (3): 711–22
Eng CM, Guffon N, Wilcox WR, et al. Safety and efficacy of recombinant human α-galactosidase A replacement therapy in Fabry’s disease. N Engl J Med 2001 Jul 5; 345 (1): 9–16
Kosch M, Koch H-G, Oliveira JP, et al. Enzyme replacement therapy administered during hemodialysis in patients with Fabry disease. Kidney Int 2004; 66 (3): 1279–82
European Medicines Agency. Fabrazyme: scientific discussion [online]. Available from URL: http://www.emea.eu.int [Accessed 2005 Oct 5]
Siamopoulos KC. Fabry disease: kidney involvement and enzyme replacement therapy. Kidney Int 2004 Feb; 65 (2): 744–53
Banikazemi M, Bultas J, Waldek S, et al. Agalsidase-beta therapy for advanced Fabry disease: a randomized trial. Ann Intern Med 2007 Jan 16; 146 (2): 77–86
Wilcox WR, Banikazemi M, Guffon N, et al. Long-term safety and efficacy of enzyme replacement therapy for Fabry disease. Am J Hum Genet 2004 Jul; 75 (1): 65–74
Germain DP, Waldek S, Banikazemi M, et al. Sustained, longterm renal stabilization after 54 months of agalsidase beta therapy in patients with Fabry disease. J Am Soc Nephrol. In press
Thurberg BL, Rennke H, Colvin RB, et al. Globotriaosylceramide accumulation in the Fabry kidney is cleared from multiple cell types after enzyme replacement therapy. Kidney Int 2002 Dec; 62 (6): 1933–46
Thurberg BL, Byers HR, Granter SR, et al. Monitoring the 3-year efficacy of enzyme replacement therapy in Fabry disease by repeated skin biopsies. J Invest Dermatol 2004 Apr; 122 (4): 900–8
Wraith J, on behalf of the AGAL-016 Study Investigators. Agalsidase beta (recombinant human a-galactosidase A) therapy in paediatric patients with Fabry disease [abstract]. 10th International Congress of Inborn Errors of Metabolism; 2006 Sep 12–16; Chiba
Eto Y, Ohashi T, Utsunomiya Y, et al. Enzyme replacement therapy in Japanese Fabry disease patients: the results of a phase 2 bridging study. J Inherit Metab Dis 2005; 28 (4): 575–83
Pisani A, Spinelli L, Sabbatini M, et al. Enzyme replacement therapy in Fabry disease patients undergoing dialysis: effects on quality of life and organ involvement. Am J Kidney Dis 2005 Jul; 46 (1): 120–7
Beer M, Weidemann F, Breunig F, et al. Impact of enzyme replacement therapy on cardiac morphology and function and late enhancement in Fabry’s cardiomyopathy. Am J Cardiol 2006; 97: 1515–8
Spinelli L, Pisani A, Sabbatini M, et al. Enzyme replacement therapy with agalsidase β improves cardiac involvement in Fabry’s disease. Clin Genet 2004 Aug; 66 (2): 158–65
Weidemann F, Breunig F, Beer M, et al. Improvement of cardiac function during enzyme replacement therapy in patients with Fabry disease: a prospective strain rate imaging study. Circulation 2003 Sep 16; 108 (11): 1299–301
Kalliokoski RJ, Kantola I, Kalliokoski KK, et al. The effect of 12-month enzyme replacement therapy on myocardial perfusion in patients with Fabry disease. J Inherit Metab Dis 2006; 29(1): 112–8
Mignani R, Panichi V, Giudicissi A, et al. Enzyme replacement therapy with agalsidase beta in kidney transplant patients with Fabry disease: a pilot study. Kidney Int 2004 Apr; 65 (4): 1381–5
Breunig F, Beer M, Knoll A, et al. Kidney function, myocardial mass and late enhancement in 17 patients with Fabry disease after 1 year of enzyme replacement therapy [abstract no. MP142]. 41st Congress of the European Renal Association and the European Dialysis and Transplant Association; 2004 May 15–18; Lisbon
Guffon N. Stabilisation of kidney function in a group of 15 patients diagnosed with Fabry disease and treated with Fabrazyme® for a year [abstract no. W272]. World Congress on Nephrology; 2003 Jun 8–12; Berlin
Hilz MJ, Brys M, Marthol H, et al. Enzyme replacement therapy improves function of C-, A6-, and Aβ-nerve fibers in Fabry neuropathy. Neurology 2004 Apr 13; 62 (7): 1066–72
Hilz MJ, Marthol H, Brys M, et al. Treatment with recombinant human alpha-galactosidase A improves cerebral blood flow velocity in Fabry patients [abstract no. P29]. 4th European Round Table on Fabry Disease; 2003 Oct 17–18; Munich
Hilz MJ, Szczepanska H, Tutaj M, et al. Enzyme replacement therapy: stability of neurophysiological and autonomic function in Fabry patients within the infusion interval [abstract]. Second Symposium on Lysosomal Storage Disorders; 2005 Mar 2–4; Athens
Banikazemi M, Ullman T, Desnick RJ. Gastrointestinal manifestations of Fabry disease: clinical response to enzyme replacement therapy. Mol Genet Metab 2005 Aug; 85 (4): 255–9
Guffon N, Fouilhoux A. Clinical benefit in Fabry patients given enzyme replacement therapy: a case series. J Inherit Metab Dis 2004; 27 (2): 221–7
Torregrosa V, de Arriba G, Checa D, et al. Health related quality of life in patients wtih Fabry disease treated with agalsidase beta: a twelve months follow-up study [abstract no. P34]. Fabry 5th Round Table Meeting; 2004 Oct 22–23; Warsaw
Diitsch M, Marthol H, Stemper B, et al. Small fiber dysfunction predominates in Fabry neuropathy. J Clin Neurophysiol 2002; 19(6): 575–86
Cole A, Cousins A, Lee PJ. ERT infusion associated reactions in Fabry disease [abstract no. 338-P]. J Inherit Metab Dis 2004; 27 Suppl. 1: 172
Linthorst GE, Hollak CEM, Donker-Koopman WE, et al. Enzyme therapy for Fabry disease: neutralizing antibodies toward agalsidase alpha and beta. Kidney Int 2004 Oct; 66 (4): 1589–95
Desnick RJ. Enzyme replacement therapy for Fabry disease: lessons from two α-galactosidase A orphan products and one FDA approval. Expert Opin Biol Ther 2004 Jul; 4 (7): 1167–76
Hughes DA, Ramaswam U, Elliott P, et al. Guidelines for the diagnosis and management of Anderson-Fabry disease [online]. Available from URL: http://www.dh.gov [Accessed 2005 Nov 21]
Barbey F, Hayoz D, Widmer U, et al. Efficacy of enzyme replacement therapy in Fabry disease. Curr Med Chem Cardiovasc Hematol Agents 2004 Oct; 2 (4): 277–86
Eng CM, Germain DP, Banikazemi M, et al. Fabry disease: guidelines for the evaluation and management of multi-organ system involvement. Genet Med 2006 Sep; 8 (9): 539–48
Warnock DG. Fabry disease: diagnosis and management, with emphasis on the renal manifestations. Curr Opin Nephrol Hypertens 2005; 14 (2): 87–95
Breunig F, Weidemann F, Beer M, et al. Fabry disease: diagnosis and treatment. Kidney Int Suppl 2003; 63 Suppl. 84: S181–5
Brenner BM, Grünfeld J-P. Renoprotection by enzyme replacement therapy. Curr Opin Nephrol Hypertens 2004; 13 (2): 231–41
Aaron JA, Ansani NT. Agalsidase beta: enzyme replacement therapy for Fabry disease. PT 2005 Apr; 30 (4): 222–4
European Medicines Agency. Replagal: summary of product characteristics [online]. Available from URL: http://www.emea.eu.int [Accessed 2005 Oct 5]
Schiffmann R, Kopp JB, Austin HA III, et al. Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA 2001 Jun 6; 285 (21): 2743–9
Food and Drug Administration. Endocrinology and Metabolic Advisory Committee Meeting (14 January 2003) [online]. Available from URL: http://www.fda.gov [Accessed 2007 Feb 12]
Sakuraba H, Murata-Ohsawa M, Kawashima I, et al. Comparison of the effects of agalsidase alfa and agalsidase beta on cultured human Fabry fibroblasts and Fabry mice. J Hum Genet 2006; 51 (3): 180–8
Linthorst G, Hollak C, Ormel E, et al. A comparative trial of two enzyme preparations for Fabry disease [abstract]. European Study Group on Lysosomal Diseases Workshop; 2003 Sep 18–21; Podebrady
Wraith JE. The management of lysosomal disorders. Curr Paediatr 2004; 14 (5): 389–93
Breunig F, Wanner C. Enzyme replacement therapy for Fabry disease: proving the clinical benefit. Nephrol Dial Transplant 2003 Jan; 18: 7–9
Genzyme. Clinical studies of Fabrazyme [online]. Available from URL: http://www.fabrazyme.com [Accessed 2005 Oct 5]
Germain DP. The Fabry registry: natural history of renal disease and effects of enzyme replacement therapy [abstract no. 334-P]. J Inherit Metab Dis 2004; 27 Suppl. 1: 170
Cho ME, Kopp JB. Fabry disease in the era of enzyme replacement therapy: a renal perspective. Pediatr Nephrol 2004; 19(6): 583–93
Mills K, Vellodi A, Morris P, et al. Monitoring the clinical and biochemical response to enzyme replacement therapy in three children with Fabry disease. Eur J Pediatr 2004 Oct; 163 (10): 595–603
Young E, Mills K, Morris P, et al. Is globotriaosylceramide a useful biomarker in Fabry disease? Acta Paediatr 2005; 94 Suppl. 447: 51–4
Goi G, Massaccesi L, Burlina AP, et al. Lysosomal leukocyte β-D-glucuronidase during enzyme replacement therapy in Fabry disease. Biochim Biophys Acta 2005; 1741: 300–6
Utsumi K, Mitsuhashi F, Asahi K, et al. Enzyme replacement therapy for Fabry disease: morphologic and histochemical changes in the urinary sediments. Clin Chim Acta 2005; 360: 103–7
Mehta A. New developments in the management of Anderson-Fabry disease. QJM 2002; 95 (10): 647–53
Cole A, Cousins A, Morgan S, et al. Hospital, home or independence for agalsidase β infusions - the patients view [abstract no. P25]. Fabry 5th Round Table Meeting; 2004 Oct 22–23; Warsaw
Linthorst GE, Vedder AC, Ormel EE, et al. Home treatment for Fabry disease: practice guidelines based on 3 years experience in The Netherlands. Nephrol Dial Transplant 2006; 21: 355–60
Waldek S, Germain DP. Burden of Fabry disease in females and the importance of early therapy: an analysis of Fabry registry data [abstract no. 327-O]. J Inherit Metab Dis 2005; 28 Suppl. 1: 165
Peterschmitt MJ, Vazquez LA, Lago NR, et al. Enzyme replacement therapy (ERT) in a pediatric patient with Fabry disease (FD) [abstract no. P18]. Fabry 5th Round Table Meeting; 2004 Oct 22–23; Warsaw
Puccini R, Andreini B, Manni E, et al. Thirty months treatment experience with agalsidase β in a young patient affected by Fabry’s disease [abstract no. P41]. 4th European Round Table on Fabry Disease; 2003 Oct 17–18; Munich
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: F. Breunig, University Hospital, Department of Medicine/Nephrology, Würzburg, Germany; G.A. Grabowski, The Children’s Hospital Research Foundation, Cincinnati Children’s Hospital Medical Center, Department of Pediatrics, University of Cincinnati, Cincinnati, Ohio, USA; P.J. Lee, Charles Dent Metabolic Unit, National Hospital for Neurology and Neurosurgery, London, England; G.E. Linthorst, Department of Internal Medicine, Academic Medical Center, Amsterdam, The Netherlands; R. Mignani, Renal Unit, Infermi Hospital, Rimini, Italy; S. Waldek, Manchester Lysosomal Storage Disease Centre, Hope Hospital, Salford, England; W.R. Wilcox, Division of Medical Genetics, Cedars-Sinai Medical Center, Los Angeles, California, USA.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘agalsidase beta’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Wolters Kluwer Health | Adis). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE search terms were ‘agalsidase beta’ or ‘alpha-galactosidase genzyme’. EMBASE and AdisBase search terms were ‘agalsidase-beta’. Searches were last updated 12 February 2006.
Selection: Studies in patients with Fabry disease who received agalsidase beta. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Agalsidase beta, Fabry disease, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
Keating, G.M., Simpson, D. Agalsidase Beta. Drugs 67, 435–456 (2007). https://doi.org/10.2165/00003495-200767030-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200767030-00007