Abstract
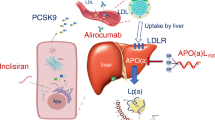
By inhibiting 3-hydroxy-3-methylglutaryl coenzyme-A (HMG-CoA) reductase, the statins reduce hepatocyte cholesterol levels, which results in up-regulation of low-density lipoprotein (LDL) receptors and, consequently, increased clearance of LDL-cholesterol (LDL-C) from the plasma. Structural differences among the available statins partially account for differences in their capacity to inhibit HMG-CoA reductase and their lipid-lowering efficacy, and for variability in other biological properties, such as their pharmacokinetic characteristics and their tolerability and propensity to interact with other drugs. In terms of pharmacokinetic properties, the synthetic (type II) HMG-CoA analogue atorvastatin exhibits a number of characteristics that are different to those of other members of the class, including a longer plasma half-life and metabolites that have an ability to inhibit HMG-CoA reductase equivalent to that of the parent drug. These characteristics are postulated to be responsible for a more prolonged inhibition of HMG-CoA reductase, and, hence, for the greater efficacy of atorvastatin in decreasing total and LDL-C levels relative to other statins (with the exception of rosuvastatin) noted in clinical trials in patients with dyslipidaemias. From the available clinical trial data, atorvastatin can be considered one of the most effective statins, not only by taking into account its effects on LDL-C and ability to meet recommended treatment guidelines for this parameter, but also its effect on triglyceride levels and capacity to modify lipoprotein composition in a non-atherogenic manner.
Clinical studies with atorvastatin have also shed some light on the question as to whether it is better to focus on obtaining maximal reduction of LDL-C in at-risk patients or on cardiovascular outcomes. Cardiovascular event rates have been shown to be substantially lower in patients attaining LDL-C levels between 1.0 and 1.6 mmol/L (40–60 mg/dL) or <1.0 mmol/L (<40 mg/dL) compared with higher levels (>2.1–2.6 mmol/L [>80-100 mg/dL]). This finding reinforces the update of the National Cholesterol Education Programme’s clinical practice guidelines, which recommend LDL-C levels <2.6 mmol/L (100 mg/dL) to be the goal of antihyperlipidaemic drug therapy in high-risk patients with CHD, with an optional therapeutic target of <1.8 mmol/L (70 mg/dL) in patients at very high risk.








Similar content being viewed by others
References
Vaughan CJ, Gotto AM Jr, Basson CT. The evolving role of statins in the management of atherosclerosis. J Am Coll Cardiol 2000; 35(1): 1–10
Igel M, Sudhop T, von Bergmann K. Pharmacology of 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (statins), including rosuvastatin and pitavastatin. J Clin Pharmacol 2002; 42(8): 835–45
Corsini A, Bellosta S, Baetta R, et al. New insights into the pharmacodynamic and pharmacokinetic properties of statins. Pharmacol Ther 1999; 84(3): 413–28
Malhotra HS, Goa KL. Atorvastatin: an updated review of its pharmacological properties and use in dyslipidaemia. Drugs 2001; 61(12): 1835–81
Davidson MH, Toth PP. Comparative effects of lipid-lowering therapies. Prog Cardiovasc Dis 2004; 47(2): 73–104
Mason RP, Walter MF, Day CA, et al. Intermolecular differences of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors contribute to distinct pharmacologic and pleiotropic actions. Am J Cardiol 2005; 96(5A): 11–23F
Istvan E. Statin inhibition of HMG-CoA reductase: a 3-dimensional view. Atherosclerosis 2003; 4 Suppl.: 3–8
Furberg CD. Natural statins and stroke risk. Circulation 1999; 99(2): 185–8
White CM. A review of the pharmacologic and pharmacokinetic aspects of rosuvastatin. J Clin Pharmacol 2002; 42(9): 963–70
Black AE, Hayes RN, Roth BD, et al. Metabolism and excretion of atorvastatin in rats and dogs. Drug Metab Dispos 1999; 27(8): 916–23
Lipitor: summary of product characteristics. New York: Pfizer Inc., 2006 Oct
Jones P, Kafonek S, Laurora I, et al. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study). Am J Cardiol 1998; 81(5): 582–7
Karalis DG, Ross AM, Vacari RM, et al. Comparison of efficacy and safety of atorvastatin and simvastatin in patients with dyslipidemia with and without coronary heart disease. Am J Cardiol 2002; 89(6): 667–71
Andrews TC, Ballantyne CM, Hsia JA, et al. Achieving and maintaining National Cholesterol Education Program low-density lipoprotein cholesterol goals with five statins. Am J Med 2001; 111(3): 185–91
Insull W, Kafonek S, Goldner D, et al. Comparison of efficacy and safety of atorvastatin (10mg) with simvastatin (10mg) at six weeks. ASSET Investigators. Am J Cardiol 2001; 87(5): 554–9
Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ 2003; 326(7404): 1423
Stalenhoef AF, Ballantyne CM, Sarti C, et al. A comparative study with rosuvastatin in subjects with metabolic syndrome: results of the COMETS study. Eur Heart J 2005; 26(24): 2664–72
Jukema JW, Liem AH, Dunselman PH, et al. LDL-C/HDL-C ratio in subjects with cardiovascular disease and a low HDL-C: results of the RADAR (Rosuvastatin and Atorvastatin in different Dosages And Reverse cholesterol transport) study. Curr Med Res Opin 2005; 21(11): 1865–74
Jones PH, Davidson MH, Stein EA, et al. Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR Trial). Am J Cardiol 2003; 92(2): 152–60
Bays HE, Ose L, Fraser N, et al. A multicenter, randomized, double-blind, placebo-controlled, factorial design study to evaluate the lipid-altering efficacy and safety profile of the ezetimibe/simvastatin tablet compared with ezetimibe and simvastatin monotherapy in patients with primary hypercholesterolemia. Clin Ther 2004; 26(11): 1758–73
Ballantyne CM, Abate N, Yuan Z, et al. Dose-comparison study of the combination of ezetimibe and simvastatin (Vytorin) versus atorvastatin in patients with hypercholesterolemia: the Vytorin Versus Atorvastatin (VYVA) study. Am Heart J 2005; 149(3): 464–73
Bakker-Arkema RG, Best J, et al. A brief review paper of the efficacy and safety of atorvastatin in early clinical trials. Atherosclerosis 1997; 131(1): 17–23
Naoumova RP, Dunn S, Rallidis L, et al. Prolonged inhibition of cholesterol synthesis explains the efficacy of atorvastatin. J Lipid Res 1997; 38(7): 1496–500
Athyros VG, Papageorgiou AA, Mercouris BR, et al. Treatment with atorvastatin to the National Cholesterol Educational Program goal versus ‘usual’ care in secondary coronary heart disease prevention: the GREek Atorvastatin and Coronary-heart-disease Evaluation (GREACE) study. Curr Med Res Opin 2002; 18(4): 220–8
Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005; 294(19): 2437–45
Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004; 350(15): 1495–504
Koren MJ, Hunninghake DB. Clinical outcomes in managed-care patients with coronary heart disease treated aggressively in lipid-lowering disease management clinics: the Alliance Study. J Am Coll Cardiol 2004; 44(9): 1772–9
Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemie events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA 2001; 285(13): 1711–8
Amarenco P, Bogousslavsky J, Callahan A 3rd, et al. High-dose atorvastatin after stroke or transient ischemie attack. N Engl J Med 2006; 355(6): 549–59
Wierzbicki AS, Mikhailidis DP. Dose-response effects of atorvastatin and simvastatin on high-density lipoprotein cholesterol in hypercholesterolaemic patients: a review of five comparative studies. Int J Cardiol 2002; 84(1): 53–7
Sivastin: summary of product characteristics. Pomezia: sigma tau, SPA, 2006 Apr
Pravaselect: summary of product characteristics. Grassina: Menarini, 2005 May
Crestor: summary of product characteristics. London: Astrazeneca Fairfax, 2006 Apr
Ginsberg HN. New perspectives on atherogenesis: role of abnormal triglyceride-rich lipoprotein metabolism. Circulation 2002; 106(16): 2137–42
Asztalos BF, Horvath KV, McNamara JR, et al. Comparing the effects of five different statins on the HDL subpopulation profiles of coronary heart disease patients. Atherosclerosis 2002; 164(2): 361–9
Mason RP. Inhibition of oxidative damage to human LDL and isolated membranes by atorvastatin and its active metabolite. J Am Coll Cardiol 2000; 35 Suppl. A: 317
Walter MF, Jacob RF, Weng Y, et al. Active hydroxy metabolite of atorvastatin increases resistance of human low-density lipoproteins to oxidative modification [abstract]. American College of Cardiology, 53rd Annual Scientific Session; 2004 Mar 7–10; New Orleans (LO)
Atalar E, Acil T, Aytemir K, et al. Effects of atorvastatin treatment on global fibrinolytic capacity, apoptosis, and leukocyte activation in patients with coronary artery disease [abstract]. J Am Coll Cardiol 2001; 37 Suppl. A: 267
Wiviott SD, Cannon CP, Morrow DA, et al. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol 2005; 46(8): 1411–6
Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004; 110(2): 227–39
LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 2005; 352(14): 1425–35
O’Keefe Jr JH, Cordain L, Harris WH, et al. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol 2004; 43(11): 2142–6
Cannon CP, Steinberg BA, Murphy SA, et al. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol 2006; 48(3): 438–45
Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366(9493): 1267–78
Robinson JG, Stone NJ. Identifying patients for aggressive cholesterol lowering: the risk curve concept. Am J Cardiol 2006; 98(10): 1405–8
Neaton JD, Blackburn H, Jacobs D, et al. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med 1992; 152(7): 1490–500
Verschuren WM, Jacobs DR, Bloemberg BP, et al. Serum total cholesterol and long-term coronary heart disease mortality in different cultures. Twenty-five-year follow-up of the seven countries study. JAMA 1995; 274(2): 131–6
The Scandinavian Simvastatin Survival Study (4S). Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994; 344(8934): 1383–9
Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996; 335(14): 1001–9
The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 1998; 339(19): 1349–57
de Lemos JA, Blazing MA, Wiviott SD, et al. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA 2004; 292(11): 1307–16
De Backer G. Evidence-based goals versus achievement in clinical practice in secondary prevention of coronary heart disease: findings in EUROASPIRE II. Atherosclerosis 2002; 2 Suppl.: 13–6
Fonarow GC, French WJ, Parsons LS, et al. Use of lipid-lowering medications at discharge in patients with acute myocardial infarction: data from the National Registry of Myocardial Infarction 3. Circulation 2001; 103(1): 38–44
Stenestrand U, Wallentin L. Early statin treatment following acute myocardial infarction and 1-year survival. JAMA 2001; 285(4): 430–6
Pearson TA, Laurora I, Chu H, et al. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med 2000; 160(4): 459–67
Avogaro A, Guida P, Giorda C, et al. The under-use of statin in type 2 diabetic patients attending diabetic clinics in Italy. Nutr Metab Cardiovasc Dis 2007; 17(1): 32–40
Di Martino M, Degli Esposti L, Ruffo P, et al. Underuse of lipid-lowering drugs and factors associated with poor adherence: a real practice analysis in Italy. Eur J Clin Pharmacol 2005; 61(3): 225–30
Acknowledgements
The preparation of this manuscript has been sponsored by Pfizer Italia, who proposed the initial idea of the review. Dr Andrea Poli has the responsibility of reported data as well as of their interpretation. The sponsor had no role in the approval of the manuscript. Dr Andrea Poli has served as consultant and/or received speaker honoraria from Pfizer, Schering Plough, Merck Sharp & Dhome, Bristol-Myers Squibb and AstraZeneca. Editorial support for the preparation of the manuscript was provided by Wolters Kluwer Health Medical Communications.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Poli, A. Atorvastatin. Drugs 67 (Suppl 1), 3–15 (2007). https://doi.org/10.2165/00003495-200767001-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200767001-00002