Summary
Abstract
Lacidipine (Caldine®, Lacimen®, Lacipil®, Midotens®, Motens®) is a once-daily, orally-administered, lipophilic dihydropyridine calcium antagonist with an intrinsically slow onset of activity, resulting in a lack of reflex tachycardia. It has a long duration of action and a high degree of vascular selectivity. In addition to calcium channel-modulated vasodilation, lacidipine displays antioxidant activity greater than that of other dihydropyridine calcium antagonists.
In randomised, well-controlled trials, lacidipine 2–6mg orally once daily had antihypertensive efficacy similar to that of other long-acting dihydropyridine calcium antagonists, thiazide diuretics, atenolol (a β-blocker) and enalapril (an ACE inhibitor). Lacidipine was effective in elderly patients (including those with isolated systolic hypertension), African Nigerian patients and patients with concurrent type 2 diabetes mellitus.
During long-term treatment for 4 or 5 years in patients with isolated systolic hypertension or essential hypertension, the incidence of cardiovascular events and mortality with lacidipine was similar to that with chlorthalidone or atenolol.
The European Lacidipine Study on Atherosclerosis (ELSA), in which 2334 patients with hypertension were randomised to 4 years of therapy with lacidipine 4–6 mg/day or the β-blocker atenolol 50–100 mg/day, demonstrated significantly lower atherosclerotic progression and plaque formation with lacidipine compared with atenolol in patients completing the full 4 years of the study. Between-group differences in favour of lacidipine for the primary efficacy variable (mean change in carotid artery intima-media thickness) did not reach statistical significance in the intent-to-treat population.
The tolerability profile of lacidipine (headache, flushing, pedal oedema, dizziness and palpitations) is similar to that of other dihydropyridine calcium antagonists, but with a lower incidence of peripheral oedema. Data from the ELSA study suggest that the incidence of serious adverse events during long-term lacidipine therapy is similar to that with atenolol.
Conclusion: Lacidipine is an effective, well tolerated, once-daily, oral antihypertensive agent that can be used in a wide variety of patients. As with other members of its class, lacidipine has shown potentially beneficial antiatherosclerotic effects, although definitive data with respect to possible superiority over other drug classes are still required. Therefore, lacidipine is an attractive therapy for the long-term management of essential hypertension.
Pharmacodynamic Properties
Lacidipine is a once-daily, orally-administered lipophilic 1,4-dihydropyridine calcium antagonist with an intrinsically slow onset of activity and long duration of action. The lipophilic nature of the drug results in the accumulation of lacidipine in membrane lipid bilayers from which it is slowly and continuously released. Lacidipine blocks voltage-dependent L-type calcium channels, producing vasodilation, and thereby reduces total peripheral vascular resistance, resulting in a reduction in blood pressure (BP). In addition, lacidipine has antioxidant activity that is considered to play a role in reducing endothelial dysfunction induced by oxidative stress. The antioxidant activity of lacidipine is greater than that of other dihydropyridine calcium antagonists.
The onset of the antihypertensive effect occurs 0.5–1.0 hours post-dose, and is maintained throughout a 24-hour period during multiple dosing. Lacidipine administration once daily in the morning reduces BP over 24 hours as demonstrated by ambulatory BP monitoring, although night-time BP is reduced to a lesser extent than day-time BP. Trough to peak plasma concentration ratios of 65% or more are commonly observed, indicating that once-daily administration is appropriate. The slow onset of activity means that lacidipine causes little or no reflex tachycardia or sympathetic activation during long-term administration. The high vascular selectivity of lacidipine results in little or no cardiodepression. Lacidipine also improves left ventricular function and, in animal models, exhibits vasoprotective properties in both the cardiovascular and cerebrovascular circulation.
Lacidipine has natriuretic and diuretic effects and is metabolically neutral, having no adverse effects on glucose or lipid metabolism. Lacidipine displays some renal protective properties in animal models, but to a lesser extent than inhibitors of the renin-angiotensin system.
There is pharmacodynamic evidence from in vitro and animal experiments to suggest that lacidipine may have antiatherosclerotic activity that is at least partly independent of BP lowering activity.
Pharmacokinetic Properties
After single-dose oral administration of lacidipine 2–6mg to healthy volunteers, mean peak plasma concentrations (Cmax) of 1.2–6.9 μg/L occurred at a median time of 1.0–1.8 hours post-dose, with high inter-individual variability. Administration of lacidipine 2–6mg once daily for 8 days produced mean steady-state Cmax values of 1.2–5.2 μg/L. Plasma concentrations are increased in the elderly and in patients with hepatic impairment. Lacidipine undergoes extensive first-pass hepatic metabolism and has a mean absolute bioavailability of approximately 10% (range 3–59%). Lacidipine is >90% bound to plasma proteins, mainly albumin. During multiple-dose administration, the terminal elimination half-life of lacidipine 2–6 mg/day was 13.2–18.7 hours. Lacidipine is completely metabolised in the liver by cytochrome P450 3A4 (CYP3A4) to pharmacologically inactive metabolites that are mainly eliminated by the biliary route and excreted in the faeces. Despite being metabolised by CYP3A4, pharmacokinetic interactions with grapefruit juice, simvastatin and digoxin are not considered clinically significant.
Therapeutic Efficacy
Dose-response studies have demonstrated that the effective therapeutic antihypertensive range of lacidipine is 2–6mg once daily, while dose-titration studies have shown that ≥77% of patients with mild-to-moderate hypertension achieve satisfactory BP control with this dose range.
In randomised, controlled trials, the antihypertensive efficacy of lacidipine 2-6mg once daily for 1–48 months in patients with mild-to-moderate essential hypertension was similar to that of other long-acting dihydropyridine calcium antagonists (sustained-release nifedipine, nifedipine gastrointestinal therapeutic system, sustained-release isradipine, nitrendipine, felodipine, amlodipine, manidipine and lercanidipine), the thiazide diuretic hydrochlorothiazide, the β-blocker atenolol and the ACE inhibitor enalapril, without affecting heart rate. Lacidipine was as effective as chlorthalidone and hydrochlorothiazide in the treatment of elderly patients with isolated systolic hypertension. In addition to its use as firstline therapy, lacidipine has value as add-on therapy in patients whose BP is inadequately controlled by other antihypertensive therapies. Lacidipine further reduced BP in patients whose hypertension was uncontrolled by β-blockers, thiazide diuretics or ACE inhibitors. Lacidipine is also effective in African Nigerians with hypertension, and in hypertensive patients with concurrent type 2 diabetes mellitus.
The European Lacidipine Study on Atherosclerosis (ELSA), the largest study of its kind to date, was designed to compare the effects of lacidipine 4–6 mg/day with those of atenolol 50–100 mg/day for 4 years on the progression of carotid artery intima-media thickness (IMT) as an index of atherosclerosis in patients with hypertension. After 4 years of therapy, the mean change in IMT was lower in lacidipine- than atenolol-treated patients, but the difference did not reach statistical significance in the intent-to-treat (ITT) population. However, the mean change in JMT was significantly (p < 0.01) lower in lacidipine-than atenolol-treated patients for the population of patients completing the full 4 years of the study (completers). Analysis of estimated treatment effect (lacidipine minus atenolol) showed significant (p < 0.0001) differences favouring lacidipine for both the ITT and completer populations. Plaque formation was also significantly (p < 0.05) less frequent in the lacidipine-treated patients.
In the long-term treatment of elderly patients with isolated systolic hypertension, the incidence of cardiovascular events (stroke, sudden death, myocardial infarction, congestive heart failure or transient ischaemic attacks) with lacidipine was similar to that with chlorthalidone over 5 years. Similarly, in the ELSA study, there was no significant difference between the lacidipine and atenolol treatment groups in the incidence of cardiovascular events and death during 4 years of treatment.
Tolerability
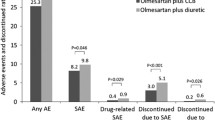
The tolerability profile of lacidipine is similar to that of other dihydropyridine calcium antagonists; although, in some studies, the incidence of pedal oedema was lower with lacidipine than with other dihydropyridine calcium antagonists. The most common adverse effects are generally attributable to the drug’s vasodilatory actions and consist of headache, flushing, pedal oedema, dizziness and palpitations. Overall, approximately 32% of patients reported adverse events in controlled therapeutic trials. Adverse events tend to occur in the first 6 months of therapy and diminish during long-term use. In the ELSA study, the incidence of serious adverse events during long-term therapy with lacidipine was small and was similar to that seen with atenolol.
Dosage and Administration
Although the most common effective oral dosage of lacidipine in clinical trials has been 4 mg/day, the recommended starting dose in the UK and many European countries in which the drug is approved is usually 2mg orally once daily, increased after 3–4 weeks to 4mg once daily. If necessary, the dosage may be further increased to 6mg once daily. However, in other countries, such as France, the recommended starting dosage is 4mg once daily, increasing to 6mg once daily after 6 weeks if BP is not adequately controlled with the starting dosage. Lacidipine should be taken at the same time each day, preferably in the morning.
The recommended initial dosage in elderly hypertensive patients is 2mg once daily. Dosage adjustment is not required in patients with renal impairment in France, but the manufacturer does not recommend the use of lacidipine in patients with severe renal impairment. Caution is required in patients with hepatic impairment and those with cardiac conduction abnormalities or reduced cardiac reserve.








Similar content being viewed by others
Notes
Use of trade names is for product identification purposes only and does not imply endorsement.
References
Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA 2003 May 21; 289(19): 2560–72
National Center for Health Statistics. Health, United States, 2002; table 68, p 210 [online]. Available from URL: http://www.cdc.gov/nchs/data/hus/tables/2002/02hus068.pdf [Accessed 2003 May 14]
Guidelines Committee. 2003 European Society of Hypertension — European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003; 21(8): 1011–53
Haller H, Cosentino F, Lüscher TF. Endothelial dysfunction, hypertension and atherosclerosis: a review of the effects of lacidipine. Drugs RD 2002; 3(5): 311–23
Alderman M, Arakawa K, Beilin L, et al. 1999 World Health Organization — International Society of Hypertension Guidelines for the Management of Hypertension. Blood Press 1999; 8 Suppl. 1: 9–43
Ramsay LE, Williams B, Johnston GD, et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens 1999 Sep; 13: 569–92
Joint National Committee on Prevention, Detection, Evaluation, and, Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1997 Nov 24; 157: 2413–46
Lee CR, Bryson HM. Lacidipine: a review of its pharmacodynamic and pharmacokinetic properties and therapeutic potential in the treatment of hypertension. Drugs 1994; 48(2): 274–96
Mason RP. Mechanisms of plaque stabilization for the dihydropyridine calcium channel blocker amlodipine: review of the evidence. Atherosclerosis 2002 Dec; 165(2): 191–9
Henderson J, Fox KM. Can calcium antagonists reverse atherosclerosis? Eur Heart J 1999; 20(13): 927–9
Simon A, Levenson J. Effects of calcium channel blockers on atherosclerosis: new insights. Acta Cardiol 2002; 57(4): 249–55
Elliott WJ, Black HR. Calcium antagonists in hypertension. Blood Press 2001; 10(5–6): 387–97
van Zwieten PA. The pharmacological properties of lipophilic calcium antagonists. Blood Press 1998; 7 Suppl. 2: 5–9
Angelico P, Guarneri L, Leonardi A, et al. Comparative in vitro studies on vasoselectivity of lercanidipine [poster 10]. 3rd European Meeting on Calcium Antagonists; 1997 Oct 29; Amsterdam
Taddei S, Virdis A, Ghiadoni L, et al. Effects of antihypertensive drags on endothelial dysfunction: clinical implications. Drugs 2002; 62(2): 265–84
Cominacini L, Fratta Pasini A, Garbin U, et al. Antioxidant activity of different dihydropyridines. Biochem Biophys Res Commun 2003 Mar 21; 302(4): 679–84
Toniolo R, Di Narda F, Bontempelli G, et al. An electroanalytical investigation on the redox properties of lacidipine supporting its anti-oxidant effect. Bioelectrochemistry 2000 Jun; 51(2): 193–200
Taddei S, Virdis A, Ghiadoni L, et al. Lacidipine restores endothelium-dependent vasodilation in essential hypertensive patients. Hypertension 1997 Dec; 30(6): 1606–12
Taddei S, Virdis A, Ghiadoni L, et al. Effect of calcium antagonist or beta blockade treatment on nitric oxide-dependent vasodilation and oxidative stress in essential hypertensive patients. J Hypertens 2001 Aug; 19(8): 1379–86
Soboleva GN, Rogoza AN, Kobilyansky AG, et al. Is the effect of different hypotensive drags on nitric oxide activity equivalent in patients with essential hypertension? [abstract no. 182]. J Hypertens 2001 Jun; 19 Suppl. 2: S294–5
Agabiti-Rosei E. The cardiac and vascular effects of lacidipine. J Cardiovasc Pharmacol 1995; 25 Suppl. 3: Sl–5
Marone C, Weidmann P, Krontiris D, et al. Acute antihypertensive efficacy of channel blockade with lacidipine, a new dihydropyridine. Curr Ther Res 1991 Dec; 50(6): 842–56
Rossi L, Costa B, Tomei R, et al. Antihypertensive effects of lacidipine during effort in mild to moderate hypertension. J Cardiovasc Pharmacol 2002 Aug; 40(2): 315–21
Masuo K, Ogihara T. Effect of lacidipine, new Ca channel blocker, on circadian rhythm of blood pressure in patients with essential hypertension: 24hrs consecutive measurement of BP [in Japanese]. Rinsho Iyaku 1993; 9(11): 2539–52
Zito M, Abate G, Cervone C, et al. Effects of antihypertensive therapy with lacidipine on ambulatory blood pressure in the elderly. J Hypertens 1991; 9 Suppl. 3: S79–83
Galderisi M, Petrocelli A, Garofalo M, et al. Comparative evaluation of the antihypertensive efficacy of once-daily sustained-release isradipine and lacidipine using 24-hour ambulatory blood-pressure monitoring. J Int Med Res 1995 Jul; 23(4): 234–43
Heber ME, Broadhurst PA, Brigden GS, et al. Effectiveness of the once-daily calcium antagonist, lacidipine, in controlling 24-hour ambulatory blood pressure. Am J Cardiol 1990 Nov 15; 66: 1228–32
Palatini P, Penzo M, Guzzardi G, et al. Ambulatory blood pressure monitoring in the assessment of antihypertensive treatment: 24-h blood pressure control with lacidipine once a day. J Hypertens 1991; 9 Suppl. 3: S61–6
Zhu LM, Wang XY, Jin CY. The efficacy of once-daily bisoprolol, lacidipine and lisinopril on 24-hour blood pressure in patients with essential hypertension [in Chinese]. Chin J Cardiol 1998; 26(1): 41–4
Yoshinaga K, Iimura O, Abe K, et al. Lacidipine (SN-305), a calcium channel blocker, its long-lasting antihypertensive effect and the effect on circadian rhythm in patients with essential hypertension [in Japanese]. Rinsho Iyaku 1993; 9(11): 2523–38
Wing LMH, Amolda LF, Harvey PJ, et al. Lacidipine, hydrochlorothiazide and their combination in systolic hypertension in the elderly. J Hypertens 1997 Dec; 15 (12 Pt 1): 1503–10
van Montfrans GA, Schelling A, Buurke EJ, et al. Dosing time of lacidipine and the circadian blood pressure curve: the MOTJME study. J Hypertens 1998 Dec; 16 Suppl. 9: S15–9
Meredith PA. Effectiveness and tolerability of lacidipine in the treatment of mild-to-moderate hypertension in general practice. J Cardiovasc Pharmacol 1997; 30 Suppl. 2: S10–4
Costa B, Zerbini O, Nacci P, et al. Relationship between doses of 1, 2, 4, and 6 mg lacidipine and blood pressure response in a randomised, double blind, parallel-group placebo-controlled, comparative study. J Hypertens 1998 Dec; 16 Suppl. 9: S45–50
Frattola A, Parati G, Castiglioni P, et al. Lacidipine and blood pressure variability in diabetic hypertensive patients. Hypertension 2000 Oct; 36(4): 622–8
Ueda S, Donnelly R, Panfilov V, et al. Lacidipine: effects on vascular pressor responses throughout the dosage interval in normotensive subjects. Br J Clin Pharmacol 1998; 46(2): 127–32
Messerli FH, Ketelhut R. Left ventricular hypertrophy: an independent risk factor. J Cardiovasc Pharmacol 1991; 17Suppl.4: S59–67
van Zwieten PA. The influence of antihypertensive drug treatment on the prevention and regression of left ventricular hypertrophy. Cardiovasc Res 2000; 45(1): 82–91
Kuschnir E. Impact of calcium antagonists on the cardiovascular system: experience with lacidipine. Drags 1999; 57 Suppl. 1: 11–7
Leonetti G, Fogari R, Mazzola C, et al. Comparison of the effects on blood pressure and left ventricular hypertrophy of lacidipine and hydrochlorothiazide in hypertensive patients. J Hypertens 1991; 9 Suppl. 3: S29–31
Sheiban I, Arosio E, Montesi G, et al. Remodeling of left ventricular geometry and function induced by lacidipine and nifedipine SR in mild-to-moderate hypertension. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S68–74
Armas-Hernández MJ, Hernández-Hernández R, Armas-Padilla MC, et al. Lacidipine on hypertension in association with lisinopril its effects on blood pressure and left ventricular mass [abstract no. P31.065]. J Hypertens 1998; 16 Suppl. 2: S243
Cristofori P, Terron A, Micheli D, et al. Vascular protection of lacidipine in salt-loaded Dahl-S rats at nonsustained antihypertensive doses. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S75–86
Gaviraghi G, Micheli D, Terron A, et al. Lacidipine: prevention of vascular damage induced by hypertension. J Cardiovasc Pharmacol 1991; 18 Suppl. 11: S7–12
Lyons D, Fowler G, Webster J, et al. An assessment of lacidipine and atenolol in mild to moderate hypertension. Br J Clin Pharmacol 1994; 37: 45–51
Yoshinaga K, Iimura O, Abe K, et al. Late phase II study of calcium channel blocker lacidipine (SN-305) in patients with essential hypertension-open study: monotherapy [in Japanese]. Rinsho Iyaku 1993; 9(12): 2789–808
Yoshinaga K, Iimura O, Abe K, et al. Early phase II study of calcium channel blocker lacidipine (SN-305) in patients with essential hypertension: pilot study [in Japanese]. Rinsho Iyaku 1993; 9(11): 2507–21
Salako BL, Kadiri S, Walker O, et al. Evaluation of lacidipine (a calcium blocker) in the treatment of hypertension in black African people: a double-blind comparison with hydrochlorothiazide. Afr J Med Med Sci 1998 Mar; 27(1–2): 73–5
Guedon J, Herrero G, Salvi S. Assessment of lacidipine, a new long-acting 1,4 dihydropyridine calcium antagonist, for the primary care of elderly hypertensive patients. Cardiol Elder 1993 Apr; 1(2): 141–8
Leonetti G, Magnani B, Pessina AC, et al. Tolerability of longterm treatment with lercanidipine versus amlodipine and lacidipine in elderly hypertensives. COHORT Study Group. Am J Hypertens 2002 Nov; 15(11): 932–40
Fogari R, Zoppi A, Corradi L, et al. Effects of different dihydropyridine calcium antagonists on plasma norepinephrine in essential hypertension. J Hypertens 2000 Dec; 18(12): 1871–5
Armas-Padilla MC, Armas-Hernández MJ, Hernandez-Hernandez R, et al. Effect of lacidipine and nifedipine GITS on platelet function in patients with essential hypertension. J Hum Hypertens 2000 Apr; 14 Suppl. 1: S91–5
Leonetti G. Comparative study of lacidipine and nifedipine SR in the treatment of hypertension: an Italian multicenter study. Northern Italian Study Group of Lacidipine in Hypertension. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S31–4
Zanchetti A, Bond MG, Hennig M, et al. Calcium antagonist lacidipine slows down progression of asymptomatic carotid atherosclerosis: principal results of the European Lacidipine Study on Atherosclerosis (ELSA), a randomized, double-blind, long-term trial. Circulation 2002; 106(19): 2422–7
Malacco E, Mancia G, Rappelli A, et al. Treatment of isolated systolic hypertension: the SHELL study results. Blood Press 2003; 12: 160–7
Epstein M. Role of a third generation calcium antagonist in the management of hypertension. Drugs 1999; 57 Suppl. 1: 1–10
de Vries RJ, Dunselman PHJM, Chin Kon Sung UG, et al. Effects of lacidipine on peak oxygen consumption, neurohormones and invasive haemodynamics in patients with mild to moderate chronic heart failure. Heart 1996; 75(2): 159–64
Lucini D, Strappazzon P, Colombo F, et al. Maintained autonomic responses to moderate exercise in hypertensive patients treated with lacidipine. J Hypertens 1997; 15 (12 Pt 2): 1751–4
Malhotra S, Kumari S, Pandhi P. Effect of calcium antagonists on stress-induced rise in blood pressure and heart rate: a double-blind, placebo-controlled study. Int J Clin Pharmacol Ther 2001 Jan; 39(1): 19–24
Rodicio JL, Ruilope LM. Assessing renal effects and renal protection. J Hypertens 1995; 13 Suppl. 4: S19–25
Sabbatini M, Leonardi A, Testa R, et al. Effect of calcium antagonists on glomerular arterioles in spontaneously hypertensive rats. Hypertension 2000 Mar; 35: 775–9
Carmines PK, Navar LG. Disparate effects of Ca channel blockade on afferent and efferent arteriolar responses to ANG II. Am J Physiol 1989 Jun; 256 (6 Pt 2): F1015–20
Hayashi K, Ozawa Y, Saruta T, et al. Renal hemodynamic effects of calcium antagonists. In: Epstein M, editor. Calcium Antagonists in Clinical Medicine. 3rd ed. Philadelphia (PA): Hanley & Belfus, Inc., 2002: 559–78
Weir MR. Appropriate use of calcium antagonists in hypertension [online]. Available from URL: http://www.hosppract.com/issues/2001/09/brweir.htm [Accessed 2003 Aug 6]
Epstein M. Calcium antagonists and the kidney: implications for renal protection. In: Epstein M, editor. Calcium Antagonists in Clinical Medicine. 3rd ed. Philadelphia (PA): Hanley & Belfus, Inc., 2002: 629–63
Agodoa LY, Appel L, Bakris GL, et al. Effect of ramipril vs amlodipine on renal outcomes in hypertensive nephrosclerosis: a randomized controlled trial. JAMA 2001; 285(21): 2719–28
Wright JT, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002 Nov 20; 288(19): 2421–31
Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effects of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001 Sep 20; 345(12): 851–60
Micheli D, Ratti E, Toson G, et al. Pharmacology of lacidipine, a vascular-selective calcium antagonist. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S1–8
Cosenzi A, Bernobich E, Plazzotta N, et al. Lacidipine reduces high blood pressure and the target organ damage induced by high fructose diet in rats. J Hypertens 1999 Jul; 17(7): 965–71
Cooper ME, Rumble JR, Gin T, et al. Diabetic renal microvascular disease: the role of hypertension and ACE inhibitors. Clin Exp Pharmaco Physiol 1992; 19 Suppl. 19: 23–7
Rappelli A, Baldinelli A, Zingaretti O, et al. The effects of antihypertensive therapy on renal function. J Hypertens 1991; 9 Suppl. 3: S37–40
Albertazzi A, Amoroso L, Del Rosso G. A multicentric trial on the long term efficacy and safety of lacidipine in hypertensive patients with chronic renal failure [abstract no. 2118]. J Hypertens 1994; 12 Suppl. 3: 120
Ruggenenti P, Perico N, Mosconi L, et al. Calcium channel blockers protect transplant patients from cyclosporine-induced daily renal hypoperfusion. Kidney Int 1993; 43: 706–11
Shand BI, Gilchrist NL, Nicholls MG, et al. Effect of lacidipine on blood pressure, vasoactive hormones, and haemorheology in elderly patients with essential hypertension [letter]. J Hum Hypertens 2000 Jul; 14(7): 473–5
Sachias BS. Platelet-endothelial interactions in atherosclerosis. Curr Atheroscler Rep 2001 Sep; 3(5): 412–6
Cayatte AJ, Du Y, Oliver-Krasinski J, et al. The thromboxane receptor antagonist S18886 but not aspirin inhibits atherogenesis in apo E-deficient mice: evidence that eicosanoids other than thromboxane contribute to atherosclerosis. Arterioscler Thromb Vasc Biol 2000 Jul; 20(7): 1724–8
Soboleva GN, Rogoza AN, Konovalova GG, et al. Endothelin1, lipid peroxidation, nitric oxide and 24-hour blood pressure profile essential hypertension: corrections of revealed disturbances on long-term lacidipine therapy [abstract no. P3.79]. J Hypertens 2001 Jun; 19 Suppl. 2: S207
Ferri C, Desideri G, Giuliani E, et al. Lacidipine blunts early vascular activation in dyslipidemic hypertensives [abstract no. C012]. Am J Hypertens 1999 Apr; 12 (Pt 2): 179
Gisonni P, Marchegiano R, Iovino G, et al. Carotid vascular structural changes: effects of antihypertensive treatment [in Italian]. Rass Int Clin Ter 1994 Jul; 74: 289–97
Galeone F, Giuntoli F, Fiore G, et al. Antihypertensive and metabolic effects of lacidipine in patients with NIDDM and/or hypertension. J Cardiovasc Pharmacol 1994; 23 Suppl. 5: S105–7
Gulizia M, Valenti R, Platania F, et al. Calcium-antagonist antihypertensive treatment in non-insulin-dependent diabetics: efficacy and safety of lacidipine versus nifedipine SR. J Cardiovasc Pharmacol 1994; 23 Suppl. 5: S101–4
Spieker C, Zidek W. The impact of lacidipine, a novel dihydropyridine calcium antagonist, on carbohydrate and lipid metabolism. J Cardiovasc Pharmacol 1995; 25 Suppl. 3: S23–6
Kurashvili RB, Chumburidze VB, Kikalishvili TT, et al. Hypotensive effect of lacidipine vs lisinopril in hypertensive NIDDM patients [abstract no. 1013]. Am J Hypertens 1999 Apr; 12 (Pt 2): 70
Bonora E, Targher G, Alberiche M, et al. Effect of chronic treatment with lacidipine or lisinopril on intracellular partitioning of glucose metabolism in type 2 diabetes mellitus. J Clin Endocrinol Metab 1999 May; 84(5): 1544–50
Da Ros L, Squassante L, Milleri S. Dose linearity of lacidipine pharmacokinetics after single and repeated oral doses in healthy volunteers. Clin Pharmacokinet 2003; 42(1): 99–106
Da Ros L, Squassante L, Milleri S, et al. Effect of grapefruit juice on lacidipine pharmacokinetics [abstract no. P993]. J Hypertens 1996 Jun; 14 Suppl. 1: S221
Ziviani L, Da Ros L, Squassante L, et al. The effects of lacidipine on the steady/state plasma concentrations of simvastatin in healthy subjects. Br J Clin Pharmacol 2001; 51(2): 147–52
Boehringer Ingelheim International GmbH. Summary of the product characteristics: Midotens 2 mg, 4 mg film coated tablets. Ingelheim: Boehringer Ingelheim International GmbH, 2002
Hall ST, Harding SM, Evans GL, et al. Clinical pharmacology of lacidipine. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S9–13
Perelman M. Selection of initial and maintenance dosages for lacidipine, a new once-daily calcium antagonist for the treatment of hypertension. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S14–9
Lau C-P, Cheung BMY. Relative efficacy and tolerability of lacidipine and amlodipine in patients with mild-to-moderate hypertension: a randomized double-blind study. J Cardiovasc Pharmacol 1996 Aug; 28(2): 328–31
United Kingdom Lacidipine Study Group. A double-blind comparison of the efficacy and safety of lacidipine with atenolol in the treatment of essential hypertension. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S27–30
Chiariello M. on behalf of the Southern Italy Lacidipine Study Group. A double-blind comparison of the efficacy and safety of lacidipine and hydrochlorothiazide in essential hypertension. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S35–7
Meredith PA. Evaluation of an antihypertensive therapy utilising meta-analysis of a clinical trial database. J Cardiovasc Pharmacol 2000; 35 (3 Suppl. 1): S1–6
Tcherdakoff P. French large-scale study evaluating the tolerability and efficacy of lacidipine. Investigators of Study LAC-05-91. J Cardiovasc Pharmacol 1995; 25 Suppl. 3: S27–32
Nami R, Rizzini P, Buracchi P, et al. Long-term antihypertensive treatment with lacidipine, a new long-acting calcium antagonist. J Cardiovasc Pharmacol 1991; 18 Suppl. 11: S22–5
Yoshinaga K, Iimura O, Abe K, et al. Clinical evaluation of calcium channel blocker lacidipine (SN-305) in patients with severe hypertension [in Japanese]. Rinsho Iyaku 1994; 10(1): 149–68
Andrésdóttir MB, van Hamersvelt HW, van Helden MJ, et al. Ankle edema formation during treatment with the calcium channel blockers lacidipine and amlodipine: a single-centre study. J Cardiovasc Pharmacol 2000; 35 (3 Suppl. 1): S25–30
Reyes AJ, Alcocer L, Velasco M, et al. Lacidipine and nifedipine GITS as fixed-dose monopharmacotherapies in essential hypertension over sixteen weeks: main results of the LASTLHY [abstract no. E007]. Am J Hypertens 1998 Apr; 11 (Pt 2): 97
Okeahialam BN, Isamade EI, Ibrahim TM, et al. The effect of lacidipine on patients with mild to moderate hypertension and the effect of a combination of lacidipine and hydrochlorothiazide in the treatment of hypertension uncontrolled after four weeks of lacidipine treatment: an open study. West Afr J Med 1998 Jan–1998 31; 17(1): 42–6
Okeahialam BN, Thacher TD, Ibrahim TM, et al. Lacidipine in the treatment of hypertension in black African people: antihypertensive, biochemical and haematological effects. Curr Med Res Opin 2000; 16(3): 184–9
Yoshinaga K, Iimura O, Abe K, et al. Late phase II study of calcium channel blocker lacidipine (SN-305) in patients with essential hypertension — open study: concurrent therapy [in Japanese]. Rinsho Iyaku 1993; 9(12): 2809–29
Stergiou GS, Malakos JS, Achimastos AD, et al. Additive hypotensive effect of a dihydropyridine calcium antagonist to that produced by a thiazide diuretic: a double-blind placebocontrolled crossover trial with ambulatory blood pressure monitoring. J Cardiovasc Pharmacol 1997 Mar; 29(3): 412–6
Pelc A, Cachin JC, Frelon JH. Hypertensive patients treated with lacidipine: costs and outcomes. Results from a French study in general practice. J Hypertens 1998 Dec; 16 Suppl. 9: S25–30
Lindholm LH, Tcherdakoff P, Zanchetti A. Safety aspects of treatment with lacidipine — a slow-onset, long-acting calcium antagonist. Blood Press 1996 Jul; 5(4): 241–9
Rizzini P, Castello C, Salvi S, et al. Efficacy and safety of lacidipine, a new long-lasting calcium antagonist, in elderly hypertensive patients. J Cardiovasc Pharmacol 1991; 17 Suppl. 4: S38–44
Leonetti G, Salvi S. A long-term study comparing lacidipine and nifedipine SR in hypertensive patients: safety data. J Cardiovasc Pharmacol 1994; 23 Suppl. 5: S108–10
Yoshinaga K, Iimura O, Abe K, et al. Efficacy and safety of Ca channel blocker, lacidipine (SN-305), in the treatment of hypertension with renal impairment [in Japanese]. Rinsho Iyaku 1994; 10(2): 403–23
Bailey RR, Shand BI, Smith AH, et al. Effect of lacidipine, a dihydropyridine calcium antagonist on renal function of hypertensive patients with renal insufficiency. Clin Nephrol 1997 Oct; 48(4): 224–9
British National Formulary. WeBNF No. 44: Lacidipine [online]. Available from URL: http://www.bnf.org/WeBNF/ [Accessed 2003 Jul 10]
Banque de Données Automatisée sur les Médicaments. Caldine 4 mg comprimés pelliculés sécables [online]. Available from URL: http://www.biam2.org [Accessed 2003 Aug 1]
Hernández-Hernández R, Velasco M, Armas-Hernandez MJ, et al. Update on the use of calcium antagonists on hypertension. J Hum Hypertens 2002; 16 Suppl. 1: S114–7
Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997 Sep 13; 350(9080): 757–64
Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity: the Swedish Trial in Old Patients with Hypertension-2 study. Lancet 1999 Nov 20; 354(9192): 1751–6
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288(23): 2981–97
Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet 2000 Jul 29; 356(9227): 366–72
Staessen JA, Wang J-G, Thijs L. Cardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003. J Hypertens 2003; 21(6): 1055–76
Kozakova M, Buralli S, Palombo C, et al. Surrogate end points of antihypertensive treatment: left ventricular hypertrophy and structural alteration of carotid arteries. Heartdrug 2001; 1(2): 89–95
Simon A, Gariepy J, Chironi G, et al. Intima-media thickness: a new tool for diagnosis and treatment of cardiovascular risk. J Hypertens 2002; 20(2): 159–69
Tang R, Hennig M, Thomasson B, et al. Baseline reproducibility of B-mode ultrasonic measurement of carotid artery intimamedia thickness: the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens 2000 Feb; 18(2): 197–201
Zanchetti A. Prevalence of carotid atherosclerosis in hypertension: preliminary baseline data from the European Lacidipine Study on Atherosclerosis (ELSA). Blood Press 1996; 5 Suppl. 4: 30–5
Zanchetti A, Bond MG, Hennig M, et al. Risk factors associated with alterations in carotid intima-media thickness in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis. J Hypertens 1998 Jul; 16(7): 949–61
Zanchetti A. Intermediate endpoints for atherosclerosis in hypertension. Blood Press 1997; 6(2): 97–102
Borhani NO, Mercuri M, Borhani PA, et al. Final outcome results of the Multicenter Isradipine Diuretic Atherosclerosis Study (MIDAS): a randomized controlled trial. JAMA 1996 Sep 11; 276(10): 785–91
Zanchetti A, Rosei EA, Palù CD, et al. The Verapamil in Hypertension and Atherosclerosis Study (VHAS): results of long-term randomized treatment with either verapamil or chlorthalidone on carotid intima-media thickness. J Hypertens 1998 Nov; 16(11): 1667–76
Simon A, Gariépy J, Moyse D, et al. Differential effects of nifedipine and co-amilozide on the progression of early carotid wall changes. Circulation 2001 Jun 19; 103: 2949–54
Pitt B, Byington RP, Furberg CD, et al. Effect of amlodipine on the progression of atherosclerosis and the occurrence of clinical events. Circulation 2000 Sep 26; 102: 1503–10
Lichtlen PR, Hugenholtz PG, Rafflenbeul W, et al. Retardation of angiographic progression of coronary artery disease by nifedipine. Results of the International Nifedipine Trial on Antiatherosclerotic Therapy (INTACT). Lancet 1990 May 12; 335(8698): 1109–13
Psaty BM, Heckbert SR, Koepsell TD, et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995 Aug 23; 274(8): 620–5
Furberg CD, Psaty BM, Meyer JV. Nifedipine. Dose-related increase in mortality in patients with coronary heart disease. Circulation 1995 Sep 1; 92(5): 1326–31
Pahor M, Guralnik JM, Corti MC, et al. Long-term survival and use of antihypertensive medications in older persons. J Am Geriatr Soc 1995 Nov; 43(11): 1191–7
Pahor M, Guralnik JM, Furberg CD, et al. Risk of gastrointestinal haemorrhage with calcium antagonists in hypertensive persons over 67 years old. Lancet 1996; 347(9008): 1061–5
Pahor M, Guralnik JM, Salive ME, et al. Do calcium channel blockers increase the risk of cancer? Am J Hypertens 1996 Jul; 9(7): 695–9
Kizer JR, Kimmel SE. Epidemiological review of the calcium channel blocker drugs: an up-to-date perspective on the proposed hazards. Arch Intern Med 2001 May 14; 161: 1145–58
van Zwieten PA, Hansson L. Calcium antagonists and safety: the turning of the tide. Blood Press 1999; 8(1): 5–8
Epstein M. Safety of calcium antagonists as antihypertensive agents: an update. In: Epstein M, editor. Calcium Antagonists in Clinical Medicine. 3rd ed. Philadelphia (PA): Hanley & Belfus, Inc., 2002: 807–32
Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet 2000 Jul 29; 356(9227): 359–65
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: M.C. Armas-Padilla, Universidad Centroccidental Lisandro Alvarado, Barquisimeto, Venezuela; M. Epstein, University School of Medicine, Miami, Florida, USA; P.A. Meredith, Gardiner Institute, Western Infirmary, Glasgow, Scotland; B. Pitt, University of Michigan Medical Center, Ann Arbor, Michigan, USA; A. Simon, Centre de Médecine Préventive Cardiovasculaire, Hôpital Broussais, Paris, France; S. Taddei, University of Pisa, Pisa, Italy; P.A. van Zwieten, University of Amsterdam, Amsterdam, The Netherlands.
Data Selection
Sources: Medical literature published in any language since 1980 on lacidipine, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: The Medline and EMBASE search term was ‘lacidipine’. AdisBase search terms were ‘lacidipine’ or ‘GR 43569’ or ‘GX 1048’ or ‘SN 305’. Searches were last updated 25 August 2003.
Selection: Studies in patients with essential hypertension who received lacidipine. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Lacidipine, hypertension, atherosclerosis, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
McCormack, P.L., Wagstaff, A.J. Lacidipine. Drugs 63, 2327–2356 (2003). https://doi.org/10.2165/00003495-200363210-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200363210-00008