Summary
Abstract
Rabeprazole is an inhibitor of the gastric proton pump. It causes dose-dependent inhibition of acid secretion.
In 8-week studies, among patients with gastro-oesophageal reflux disease (GORD), rabeprazole 20 mg/day or 10mg twice daily was as effective as omeprazole and superior to ranitidine in the healing of GORD. Symptom relief with rabeprazole was superior to that provided by placebo and ranitidine and similar to omeprazole. In long-term trials rabeprazole 10 mg/day was similar to omeprazole 20 mg/day in a 2-year study and superior to placebo in 1-year studies, in both the maintenance of healing and prevention of symptoms in patients with healed GORD.
In nonerosive GORD, 4-week studies have shown rabeprazole to be more effective than placebo in relieving heartburn and various other gastrointestinal symptoms. Data among patients with Barrett’s oesophagus suggest rabeprazole 20 mg/day may be more effective than placebo in maintaining healing of associated oesophagitis after 1 year of treatment.
One-week triple Helicobacter pylori eradication therapy with rabeprazole plus clarithromycin and amoxicillin achieved eradication rates of ≥85%. Rabeprazole is as effective as omeprazole and lansoprazole when included as part of a triple-therapy regimen for the eradication of H. pylori. Eradication rates of >90% were achieved when rabeprazole 20 to 40 mg/day was included as part of a quadruple eradication regimen.
As monotherapy for peptic ulcer healing and symptom relief, 4- to 8-week studies have shown rabeprazole 10 to 40 mg/day to be superior to placebo and ranitidine and have similar efficacy to omeprazole. Preliminary 1-year data among 16 patients with Zollinger-Ellison syndrome suggest rabeprazole 60 to 120 mg/day can resolve and prevent the recurrence of symptoms and endoscopic lesions associated with this condition.
In clinical trials of up to 2 years’ duration the tolerability of rabeprazole is similar to that of placebo, ranitidine and omeprazole. Common adverse events assigned to rabeprazole have been diarrhoea, headache, rhinitis, nausea, pharyngitis and abdominal pain. Histological changes and increases in serum gastrin levels were unremarkable and typical of proton pump inhibitors. No dosage adjustment is necessary in renal and mild to moderate hepatic impairment.
Conclusion: Rabeprazole is a well tolerated proton pump inhibitor. It has proven efficacy in healing, symptom relief and prevention of relapse of peptic ulcers and GORD and can form part of effective H. pylori eradication regimens. It is an important alternative to H2 antagonists and an additional treatment option to other proton pump inhibitors in the management of acid-related disorders.
Overview of Pharmacological Properties
Rabeprazole inhibits the gastric parietal cell proton pump (H+/K+-ATPase), dose-dependently reducing basal and peptone-stimulated acid secretion with 20 mg/day providing the optimum antisecretory effect.
In healthy volunteers, rabeprazole had a similar or faster onset of action than omeprazole and pantoprazole. In addition, rabeprazole had a greater antisecretory effect over a 24-hour period than esomeprazole, omeprazole, lansoprazole and pantoprazole. Rabeprazole had a duration of action of ≥24 hours. Among patients with gastro-oesophageal reflux disease (GORD) rabeprazole is as effective as omeprazole and more effective than placebo in normalising 24-hour oesophageal acid exposure.
Rabeprazole produces dose-dependent increases in gastrin levels which are directly related to increases in pH and has no effect on endocrine function.
Unlike omeprazole and lansoprazole, multiple-dose studies in volunteers have shown the effect of rabeprazole on intragastric pH to be unaffected by cytochrome P450 (CYP) 2C19 genotype status.
Rabeprazole is dose-dependently absorbed after oral administration and is extensively metabolised primarily via nonenzymatic metabolism with minor contributions from CYP 3A and 2C19 pathways. Rabeprazole is extensively distributed in a variety of tissues including gastric mucosa and 96% bound to plasma proteins. No significant accumulation occurs during repeated administration, and 90% of a dose is excreted in the urine as its thioether carboxylic acid metabolite and its glucuronide and mercapturic acid metabolites. The elimination half-life of rabeprazole is ≈1 to 2 hours. Other than pH-dependent interactions with digoxin and ketoconazole, rabeprazole has no clinically significant drug interactions. Administration of food slows the rate but does not affect the extent of absorption.
Therapeutic Efficacy
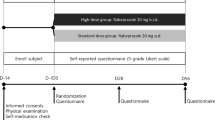
The efficacy of oral rabeprazole has been studied in patients with gastric or duodenal ulcers, erosive and nonerosive GORD, Zollinger-Ellison syndrome and Helicobacter pylori infection.
GORD. Rabeprazole 20 mg/day was as effective as omeprazole 20 mg/day and superior to ranitidine 150mg four times daily in the healing of erosive GORD. In addition, the proportion of patients who reported improvement in the frequency of heartburn, complete resolution of daytime heartburn severity, complete resolution of night-time heartburn severity and overall well-being were significantly higher in rabeprazole-treated patients than in those receiving ranitidine. Preliminary data from two 1-week, well designed trials comparing rabeprazole 20 mg/day with omeprazole 20 or 40 mg/day in patients with erosive GORD suggest rabeprazole may provide faster resolution of symptoms than omeprazole.
Well designed trials have compared the efficacy of rabeprazole 10 and 20 mg/day with placebo or omeprazole 20 mg/day in maintaining healing and symptom relief in patients following healing of grades 2 to 4 GORD. One study demonstrated no difference in relapse rates between rabeprazole 10 mg/day and omeprazole 20 mg/day regimens after 1 year of treatment. In addition, the probability of remaining healed at 2 years was 100% for patients treated with omeprazole 20 mg/day or rabeprazole 10 mg/day versus 97.5% for those treated with rabeprazole 20 mg/day. There were no significant differences in symptom frequency or severity between regimens after 2 years of treatment. In addition, 1-year placebo-controlled studies report rabeprazole (10 and 20 mg/day) to be superior to placebo in both maintenance of healing and the reduction of the rate and severity of symptoms in patients with healed GORD.
In patients with nonerosive GORD, two 4-week, well controlled studies have shown rabeprazole 10 and 20 mg/day to be more effective than placebo in relieving heartburn and various other gastrointestinal symptoms. Onset of treatment benefit was seen from the first day of treatment. Rabeprazole was significantly better than placebo in reducing daytime and night-time heartburn symptoms and in a further trial in reducing the mean gastro-oesophageal symptom assessment distress scale score within a 4-week period.
In a nonblind, 1-year study among patients with Barrett’s oesophagus, rabeprazole 20 mg/day was significantly more effective than placebo in maintaining healing of associated erosive GORD at all time points. At week 52, 90% of patients treated with rabeprazole 20 mg/day remained healed versus 47% in the placebo group.
Duodenal Ulcer and Gastric Ulcer. In randomised trials, as part of triple therapy, rabeprazole 20 to 40 mg/day has been shown to be an effective part of a H. pylori eradication triple-therapy regimen. When combined with twice daily clarithromycin 500mg and either metronidazole 400mg or amoxicillin 1g eradication rates of ≥90% can be achieved. In three large, randomised studies, rabeprazole as part of a 7-day triple-therapy eradication regimen was as effective as omeprazole or lansoprazole. In a well designed study rabeprazole 20mg twice daily was compared with omeprazole 20mg twice daily in addition to clarithromycin 500mg twice daily and amoxicillin 1g twice daily. Intention-to-treat analysis revealed eradication rates of 84% for rabeprazole-treated patients versus 69% for omeprazole-treated patients (no p-value reported). In a nonblind study, eradication rates with lansoprazole 30mg twice daily, rabeprazole 20mg and 10mg twice daily in addition to amoxicillin 500mg three times a day and clarithromycin 200mg twice daily were 82.7, 85.6 and 87%, respectively.
Eradication rates of >90% were achieved in two randomised trials in Japanese patients given rabeprazole 20 or 40 mg/day as part of a 5-day quadruple H. pylori eradication regimen containing amoxicillin 750mg, clarithromycin 200mg and metronidazole 250mg, all given twice daily. In one study, per-protocol analysis revealed eradication rates of 95% for a 5-day quadruple regimen compared with 82% for a 7-day triple regimen (p < 0.05).
The effect of CYP 2C19 genotype status on the cure rates of rabeprazole-based H. pylori eradication regimens appears unclear and further data are required.
When used as monotherapy, for peptic ulcer healing and symptom relief, well designed trials of 4 to 6 weeks’ duration have shown rabeprazole 10 to 40 mg/day to be superior to placebo and ranitidine and similar to omeprazole. Among patients with active duodenal ulcer disease rabeprazole showed higher healing rates (83 vs 73%; p = 0.017) at week 4 and provided faster symptom relief than ranitidine 150mg twice daily in one study. Data from a large study among patients with gastric ulcer disease found 3- and 6-week healing rates to be similar in both rabeprazole and omeprazole 20 mg/day recipients but day and night-time pain improved to a greater extent with rabeprazole.
Preliminary data from a small, noncomparative 1-year study indicate that rabeprazole in dosages of up to 120 mg/day can resolve, and prevent the recurrence of symptoms and endoscopic lesions associated with Zollinger-Ellison syndrome.
Tolerability
Rabeprazole has been well tolerated in short- and long-term studies of up to 2 years in duration when administered in doses of up to 120 mg/day for the treatment of acid-related disorders. In over 1700 patients only headache (2.4%) was reported more often than with placebo. The most common adverse events reported in clinical trials were headache, diarrhoea, rhinitis, nausea, pharyngitis and abdominal pain. Flatulence occurred significantly more frequently in omeprazole-treated patients and less frequently in ranitidine-treated patients than in rabeprazole-treated patients in three well designed comparative studies. No other significant differences occurred between treatment groups.
Serum gastrin changes that are consistent with proton pump inhibitor pharmacology have been reported in well designed trials, in patients receiving rabeprazole. No trial reported mean values at endpoint that were outside the normal range. In controlled clinical trials 3/1456 patients treated with rabeprazole and 2/237 patients treated with placebo developed treatment-emergent abnormalities in AST, ALT or both.
Scoring of enterochromaffin-like cells in biopsies taken prospectively from patients in studies of up to 2 years in duration demonstrate some hyperplastic changes, but no evidence of adenomatoid, dysplastic or neoplastic changes.
Pharmacoeconomic Issues
In the treatment and relapse prevention of GORD, US studies using decision analysis models have shown rabeprazole to be more cost effective than omeprazole, lansoprazole and ranitidine; however, no study was performed alongside a prospective clinical trial. In analyses from a third-party perspective, a 1-year relapse prevention study reported treatment with rabeprazole resulted in an average cost-effectiveness ratio of $US1637 per occurrence prevented, compared with $US2439 for lansoprazole and $US1968 for omeprazole. The incremental cost per patient, relative to rabeprazole, was $US257 for lansoprazole and $US185 for omeprazole. In the treatment of GORD, the incremental cost-effectiveness ratio was $US313 when rabeprazole was compared with ranitidine. For ranitidine and rabeprazole to be equally cost effective, the 8-week system response rate with ranitidine therapy would have had to increase from 28 to 72%.
Dosage and Administration
Rabeprazole is licensed world wide for use in acid-related disorders; however, it is not licensed in the US for the treatment of gastric ulcer or as part of a H. pylori eradication regimen. The usual oral dosage for the treatment of duodenal ulcers, gastric ulcers and GORD is 20 mg/day for 4 to 8 weeks with a further course given if needed. The dosage can be reduced to 10 to 20 mg/day for maintenance therapy. In Europe rabeprazole 10 mg/day is licensed for the treatment of non-erosive GORD. In H. pylori eradication regimens the licensed oral dosage is 20mg twice daily as part of a 7-day triple-therapy regimen. Dosages for Zollinger-Ellison syndrome, in the US, are up to 60mg twice daily.
The dosage of rabeprazole need not be adjusted in the elderly or in those with renal and mild-to-moderate hepatic impairment. As with other proton pump inhibitors coadministration of rabeprazole with digoxin and ketoconazole should be treated with caution.









Similar content being viewed by others
References
Xia HH-X, Talley NJ. Helicobacter pylori eradication in patients with non-ulcer dyspepsia. Drugs 1999 Nov; 58: 785–92
Langtry H, Wilde MI. Omeprazole. A review of its use in Helicobacter pylori infection, gastro-oesophageal reflux disease and peptic ulcers induced by nonsteroidal anti-inflammatory drugs. Drugs 1998; 56(3): 447–86
Johnson D, Perdomo C, Barth J, et al. The benefit/risk profile of rabeprazole, a new proton-pump inhibitor. Eur J Gastroenterol Hepatol 2000 Jul; 12(7): 799–806
Moskovitz M, Fass R. Preventing relapse of recurrent erosive or ulcerative GERD: focus on rabeprazole. PT 2000; 25(9): 492–500
Byrne MF, Murray FE. Formulary management of proton pump inhibitors. Pharmacoeconomics 1999 Sep; 16: 225–46
Langtry HD, Markham A. Rabeprazole: a review of its use in acid-related gastrointestinal disorders. Drugs 1999 Oct; 58: 725–42
Tsutsui N, Taneike I, Ohara T, et al. A novel action of the proton pump inhibitor rabeprazole and its thioether derivative against the motility of Helicobacter pylori. Antimicrob Agents Chemother 2000 Nov; 44(11): 3069–73
Kawakami Y, Akahane T, Yamaguchi M, et al. In vitro activities of rabeprazole, a novel proton pump inhibitor, and its thioether derivative alone and in combination with other antimicrobials against recent clinical isolates of Helicobacter pylori. Antimicrob Agents Chemother 2000 Feb; 44(2): 458–61
Watanabe T, Higuchi K, Tominaga K, et al. Cytoprotective effect of rabeprazole against ethanol-induced gastric mucosal damage: possible involvement of nitric oxide. Drugs Exp Clin Res 2000; 26(2): 41–5
Sukegawa M, Hokari K, Takeda H, et al. Effect of lansoprazole and rabeprazole on intragastric acidity in relation to CYP2C19 genotype status [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2. (Pt 2): 1310
Adachi K, Katsube T, Kawamura A, et al. CYP2C19 genotype status and intragastric pH during dosing with lansoprazole or rabeprazole. Aliment Pharmacol Ther 2000 Oct; 14(10): 1259–66
Lew EA, Barbuti RC, Kovacs TOG, et al. An ascending single-dose safety and tolerance study of an oral formulation of rabeprazole (E3810). Aliment Pharmacol Ther 1998 Jul 12: 667–72
Robinson M, Maton PN, Rodriguez S, et al. Effects of oral rabeprazole on oesophageal and gastric pH in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 1997 Oct 11: 973–80
Ohning GV, Barbuti RC, Kovacs TOG, et al. Rabeprazole produces rapid, potent, and long-acting inhibition of gastric acid secretion in subjects with Helicobacter pylori infection. Aliment Pharmacol Ther 2000 Jun; 14: 701–8
Williams MP, Blanshard C, Millson C, et al. A placebo-controlled study to assess the effects of 7-day dosing with 10, 20 and 40 mg rabeprazole on 24-h intragastric acidity and plasma gastrin in healthy male subjects. Aliment Pharmacol Ther 2000 Jun; 14: 691–9
Gardner JD, Sloan S, Barth JA, et al. Determination of onset, duration of action and maximal effect of rabeprazole on gastric and esophageal acidity in GERD [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 2): 1236
Gardner JD, Sloan S, Barth JA, et al. Maximal or near-maximal inhibition of esophageal acidity by the 1 st dose of rabeprazole in GERD [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt2): 1237
Pantoflickova D, Dorta G, Jornod P, et al. Identification of the characteristics influencing the degree of antisecretory activity of PPIs [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (4): 1290
Pantoflickova D, Dorta G, Jornod P, et al. Antisecretory activity of PPIs [abstract]. Gut 2000 Dec; 47 Suppl. III: 64
Ohning GV, Kovacs TO, Murthy A, et al. Rabeprazole is superior to omeprazole for inhibition of meal-stimulated gastric acid secretion in H. pylori-negative subjects [abstract]. Am J Gastroenterol 2001; 96(9): 27
Williams MP, Sercombe J, Pounder RE, et al. A placebo-controlled trial to assess the effects of 8 days of dosing with rabeprazole versus omeprazole on 24-h intragastric acidity and plasma gastrin concentrations in young healthy male subjects. Aliment Pharmacol Ther 1998; 12: 1079–89
Gardner JD, Sloan S, Barth JA. Rabeprazole vs omeprazole: onset, duration, and magnitude of gastric antisecretory effects [abstract]. Gut 2000 Dec; 47 Suppl. III: 61
Gardner JD, Sloan S, Barth JA. Onset, duration, and magnitude of gastric antisecretory effects of rabeprazole and omeprazole [abstract plus poster]. Am J Gastroenterol 1999 Sep; 94: 2608
Baisley KJ, Tejura B, Morocutti A, et al. Rabeprazole 20 mg is more potent than esomeprazole 20 mg in control of gastric pH in healthy volunteers [abstract]. Am J Gastroenterol 2001 Sep; 96(9): 48
Birbara C, Breiter J, Perdomo C, et al. Rabeprazole for the prevention of recurrent erosive or ulcerative gastro-oesophageal reflux disease. Rabeprazole Study Group. Eur J Gastroenterol Hepatol 2000 Aug; 12(8): 889–97
Dammann H-G, Burkhardt F, Wolf N. The effects of oral rabeprazole on endocrine and gastric secretory function in healthy volunteers. Aliment Pharmacol Ther 1999 Sep; 13: 1195–203
Galmiche JP, Zerbib F, Ducrotte P, et al. Decreasing oesphageal acid exposure in patients with GERD: a comparison of rabeprazole and omeprazole. Aliment Pharmacol Ther 2001; 15: 1343–50
Horai Y, Kimura M, Furuie H, et al. Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther 2001 Jun; 15: 793–803
Shirai N, Furuta T, Takashima M, et al. Effects of genotypic differences in CYP2C19 on intragastric pH values after single and repeated doses of omeprazole and rabeprazole [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 1): 501
Tsutsui N, Taneike I, Ohara T, et al. A novel action of the proton pump inhibitor rabeprazole and its thioether derivative against the motility of Helicobacter pylori. Antimicrob Agents Chemother 2000 Nov; 44: 3069–73
Yasuda S, Ohnishi A, Ogawa T, et al. Pharmacokinetic properties of E3810, a new proton pump inhibitor, in healthy male volunteers. Int J Clin Pharmacol Ther 1994 Sep; 32: 466–73
Swan SK, Hoyumpa AM, Merritt GJ. The pharmacokinetics of rabeprazole in health and disease. Aliment Pharmacol Ther 1999; 13 Suppl. 3: 11–7
Rabeprazole product monograph. Misato, Japan: Eisai Co., Ltd, 2000
Humphries TJ, Nardi RV, Lazar JD, et al. Drag-drug interaction evaluation of rabeprazole sodium: a clean/expected slate? [abstract]. Gut 1996; 39 Suppl. 3: 47
Andersson T, Cederberg C, Heggelund A, et al. The pharmacokinetics of single and repeated once-daily doses of 10, 20 and 40mg omperazole as enteric-coated granules. Drag Invest 1991; 3: 45–52
Yasuda S, Horai Y, Tomono Y, et al. Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4′-hydroxylation status. Clin Pharmacol Ther 1995 Aug; 58(2): 143–54
Pichard-Garcia L, Whomsley R, Daujat M, et al. Comparative effects of rabeprazole and omeprazole on the inducibility of cytochrome P450-1A and cytochrome P450-3A isoenzymes in human hepatocytes, and effects on cyclosporin metabolism in human liver microsomes. Clin Drag Invest 2000 Oct; 20: 245–54
Ishizaki T, Chiba K, Manabe K, et al. Comparison of the interaction potential of a new proton pump inhibitor, E3810, versus omeprazole with diazepam in extensive and poor metabolizers of S-mephenytoin 4’-hydroxylation. Clin Pharmacol Ther 1995 Aug; 58: 155–64
Farley A, Wruble LD, Humphries TJ. Rabeprazole versus ranitidine for the treatment of erosive gastroesophageal reflux disease: a double-blind, randomized clinical trial. Rabeprazole Study Group. Am J Gastroenterol 2000 Aug; 95(8): 1894–9
Dekkers CPM, Beker JA, Thjodleifsson B, et al. Double-blind placebo-controlled comparison of rabeprazole 20 mg vs omeprazole 20 mg in the treatment of erosive or ulcerative gastro-oesophageal reflux disease. Aliment Pharmacol Ther 1999 Jan; 13: 49–57
Delchier JC, Cohen G, Humphries TJ. Rabeprazole, 20 mg once daily or 10 mg twice daily, is equivalent to omeprazole, 20 mg once daily, in the healing of erosive gastro-oesophageal reflux disease. Scand J Gastroenterol 2000 Dec; 35: 1245–50
Holtmann G, Bytzer P, Blum AL. Clinical efficacy of a standard dose rabeprazole and a high dose omeprazole for the relief of GERD symptoms [abstract]. Gastroenterology 2001 Apr; 120 Suppl. 1: 435
Sloan S, Camacho F, Perdomo C, et al. Rabeprazole provides better heartburn relief compared to omeprazole in the first 3 and 7 days of treatment [abstract]. Gut 2000 Dec; 47 Suppl. III: 62
Jokubaitis L, Murthy A, Hegedus R, et al. The future of acid suppression therapy trial with rabeprazole: preliminary analysis of acute symptom relief [abstract plus poster]. Am J Gastroenterol 2000 Sep; 95: 2423
Robinson M, Murthy A, Barth J, et al. Rabeprazole 20 mg in future of acid suppresssion therapy (F.A.S.T.) trial: acute heartburn relief in patients refractory to omeprazole and lansoprazole [abstract]. Gut 2001 Mar; 48 Suppl. 1: 25
Thjodleifsson B, Beker JA, Dekkers C, et al. Rabeprazole versus omeprazole in preventing relapse of erosive or ulcerative gastroesophageal reflux disease: a double-blind, multicenter, European trial. The European Rabeprazole Study Group. Dig Dis Sci 2000 May; 45(5): 845–53
Humphries TJ, Thjodleifsson B, Perdomo C. Rabeprazole and omeprazole in long-term maintenance of erosive or ulcerative GERD [abstract plus poster]. Am J Gastroenterol 1999 Sep; 94: 2587
Caos A, Moskovitz M, Dayal Y, et al. Rabeprazole for the prevention of pathologic and symptomatic relapse of erosive or ulcerative gastroesophageal reflux disease. Rebeprazole Study Group. Am J Gastroenterol 2000 Nov; 95(11): 3081–8
Dean BB, Siddique RM, Yamashita BD, et al. Cost-effectiveness of proton-pump inhibitors for maintenance therapy of erosive reflux esophagitis. Am J Health-Syst Pharm 2001 Jul 15; 58: 1338–46
Miner P, Fillipone J, Jokubaitis L, et al. Rabeprazole relieves heartburn and associated symptoms in nonerosive gastroesophageal reflux disease [abstract]. Am J Gastroenterol 2000 Sep; 95: 2435
Miner P, Sloan S, Filippone J, et al. Significant heartburn relief after the first dose of rabeprazole sodium in non-erosive reflux disease (NERD) patients [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 1): 19
Siddique R, Sloan S, Zheng M, et al. Rabeprazole relieves symptom distress in patients with non-erosive gastroesphageal reflux disease (GERD) [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 2): 1096
Siddique R, Sloan S, Bhattacharjya A, et al. Rabeprazole relieves symptom distress in patients with non-erosive gastro-oesophageal reflux disease [abstract]. Gut 2000 Dec; 47 Suppl. III: 61–2
Barth J, Perdomo C, Sloan S, et al. Rabeprazole maintains GERD healing in patients with Barrett’s esophagus [abstract plus poster]. Am J Gastroenterol 1999 Sep; 94: 2579
Dajani EZ, Klamut MJ. Novel therapeutic approaches to gastric and duodenal ulcers: an update. Expert Opin Investig Drags 2000 Jul; 9(7): 1537–44
Helicobacter pylori Consensus Conference: review 1999. Conclusions and revised recommendations of the working group [in French]. Hepatogastroenterology 1999 Nov–1999 31; 6 Suppl. 6: 9–18
Miwa H, Ohkura R, Murai T, et al. Impact of rabeprazole, a new proton pump inhibitor, in triple therapy for Helicobacter pylori infection: comparison with omeprazole and lansoprazole. Aliment Pharmacol Ther 1999; 13: 741–6
Moayyedi P. Finding the optimum treatment for Helicobacter pylori. Dig Liver Dis 2000; 32(2): 116–8
Gisbert JP, Calvet X, Gomollon F, et al. Eradication treatment of Helicobacter pylori. Recommendations of the Spanish Consensus Conference [in Spanish]. Med Clin (Barc) 2000 Feb 12; 114: 185–95
Stack WA, Knifton A, Thirlwell D, et al. Safety and efficacy of rabeprazole in combination with four antibiotic regimens for the eradication of Helicobacter pylori in patients with chronic gastritis with or without peptic ulceration. Am J Gastroenterol 1998; 93(10): 1909–12
Kihira K, Satoh K, Saifuku K, et al. Rabeprazole, amoxycillin and low- or high-dose clarithromycin for cure of Helicobacter pylori infection. Aliment Pharmacol Ther 2000 Aug; 14(8): 1083–7
Miwa H, Yamada T, Sato K, et al. Efficacy of reduced dosage of rabeprazole in PPI/AC therapy for Helicobacter pylori infection: comparison of 20 and 40mg rabeprazole with 60 mg Lansoprazole. Dig Dis Sci 2000 Jan; 45: 77–82
Hawkey CJ, Treichel HC, Krankenhjaus J, et al. Rabeprazole vs omeprazole in 7-day, triple-therapy H. pylori eradication regimens for peptic ulcer. Gastroenterology 2001 Apr; 120 Suppl. 1: 581
Kihira K, Sugano K, Kimura K, et al. Effect of triple therapy with new proton pump inhibitor rabeprazole, amoxicillin and low or high dose of clarithromycin for Helicobacter pylori infection [abstract]. Gut 1999 Sep; 45 Suppl. III: 117
Cammarota G, Cianci R, Cannizzaro O, et al. Efficacy of two one-week rabeprazole/levofloxacin-based triple therapies for Helicobacter pylori infection. Aliment Pharmacol Ther 2000 Oct; 14(10): 1339–43
Danese S, Armuzzi A, Romano A, et al. Efficacy and tolerability of antibiotics in patients undergoing H-pylori eradication. Hepatogastroenterology 2001 Mar 30; 48: 465–7
Isomoto H, Furusu H, Morikawa T, et al. 5-day vs. 7-day triple therapy with rabeprazole, clarithromycin and amoxicillin for Helicobacter pylori eradication. Aliment Pharmacol Ther 2000 Dec; 14(12): 1619–23
Nagahara A, Miwa H, Ogawa K, et al. Addition of metronidazole to rabeprazole-amoxicillin-clarithromycin regimen for Helicobacter pylori infection provides an excellent cure rate with five-day therapy. Helicobacter 2000 Jun; 5(2): 88–93
Karatapanis S, Georgopoulos S, Papakonstantinou L, et al. Rabeprazole 7-days vs rabeprazole 10-days triple therapy in the eradication of H. pylori infection: a randomized study [abstract]. Gut 2000 Oct; 47 Suppl. 1: 107
Takahashi M, Katayama Y, Takada H, et al. Continuation of acid suppression therapy by rabeprazole after successful Helicobacter pylori eradication accelerates peptic ulcer healing: single-center prospective randomized control study [abstract]. Gastroenterology 2000 Apr; 118 (Suppl. 2. Pt 2): 1312
Nagahara A, Miwa H, Yamada T, et al. Five-day proton pump inhibitor-based quadruple therapy regimen is more effective than 7-day triple therapy regimen for Helicobacter pylori infection. Aliment Pharmacol Ther 2001 Mar; 15: 417–21
Furuta T, Shirai N, Takashima M, et al. Effects of genetic differences in CYP2C19 status on cure rates of Helicobacter pylori infection by dual rabeprazole/amoxicillin therapy in comparison with dual omeprazole/amoxicillin therapy [abstract]. Gastroenterology 2000 Apr; 118 Suppl. 2 (Pt 1): 495
Dojo M, Azuma T, Ohtani M, et al. Effects of CYP2C19 gene polymorphism on cure rates for Helicobacter pylori infection by triple therapy with proton pump inhibitor (omeprazole or rabeprazole), amoxicllin, and clarithromycin [abstract]. Gastroenterology 2001 Apr; 120 Suppl. 1: 582
Breiter JR, Riff D, Humphries TJ, et al. Rabeprazole is superior to ranitidine in the management of active duodenal ulcer disease: results of a double-blind, randomized North American study. Am J Gastroenterol 2000 Apr; 95: 936–42
Shim CS, Cho JY, Chung IS, et al. Rabeprazole 10mg versus omeprazole 20mg in the treatment of duodenal ulcer: the First Korean Multicenter, Comparative trial [abstract]. J Gastroenterol Hepatol 2000 Mar; 15 Suppl.: 44
Cloud ML, Enas N, Humphries TJ, et al. Rabeprazole in treatment of acid peptic diseases: results of three placebo-controlled dose-response clinical trials in duodenal ulcer, gastric ulcer, and gastro-oesophageal reflux disease (GERD). Dig Dis Sci 1998 May; 43: 993–1000
Dekkers CPM, Beker JA, Thjodleifsson B, et al. Comparison of rabeprazole 20mg vs omperazole 20mg in the treatment of active gastric ulcer: a European multicentre study. European Rabeprazole Study Group. Aliment Pharmacol Ther 1998 Aug; 12: 789–95
Mignon M, Merrouche M, Gardner JD, et al. Rabeprazole therapy is effective in Zollinger-Ellison syndrome and idiopathic gastric acid hypersecretion [abstract]. Am J Gastroenterol 1999 Sep; 94: 2613
Thjodleifsson B, Cockburn I. Review article: rabeprazole’s tolerability profile in clinical trials. Aliment Pharmacol Ther 1999 Oct; 13 Suppl. 5: 17–23
Papathoma K. The effectiveness and safety of rabeprazole in clinical practice. Hellenic Rabeprazole Study Group [abstract]. Gut 2000 Dec; 47 Suppl. III: 130–1
Johnson D, Riff R, Perdomo C, et al. Rabeprazole: safety profile of a new proton pump inhibitor [abstract no G0875]. Gastroenterology 1999 Apr; 116(4): 201
Johnstone D, Berger C, Fleckman P, et al. Acute fulminant hepatitis after treatment with rabeprazole and terbinafine. Arch Intern Med 2001 Jul 9; 161: 1677–8
Gardner JD, Rindi G, Fiocca R, et al. Changes in H. pylori infection and accompanying pathology during 4 years of rabeprazole treatment [abstract]. Gut 1999 Sep; 45 Suppl. III: 115–6
Keane WF, Swan SK, Grimes I, et al. Rabeprazole: pharmacokinetics and tolerability in patients with stable, end-stage renal failure. J Clin Pharmacol 1999; 39: 927–33
Hoyumpa A M, Trevino-Alanis H, Grimes I, et al. Rabeprazole: pharmacokinetics in patients with stable compensated cirrhosis. Clin Ther 1999; 21(4): 691–701
Ofman JJ, Yamashita BD, Siddique RM, et al. Cost effectiveness of rabeprazole versus generic ranitidine for symptom resolution in patients with erosive esophagitis. Am J Manag Care 2000 Aug; 6: 905–16
Hilleman DE, Foral PA. Pharmacoeconomic analysis of proton-pump inhibitor therapy in gastroesophageal reflux disease: a meta-analytic approach [abstract]. Pharmacotherapy 2001 Mar; 21: 378
Rabeprazole: UK product information. 2000 Hammersmith, London: Eisai Ltd, 2000
Pariet 10mg cleared for GERD in EU. Marketletter 2001 Sep 17; 8: 20
Galmiche JP. How do we offer clinical relief to patients with gastro-oesophageal reflux disease? Eur J Gastroenterol Hepatol 2000 Jun; 12 Suppl. 1: 3–6
Pohle T, Domschke W. Results of short- and long-term medical treatment of gastroesophageal reflux disease (GERD). Langenbecks Arch Surg 2000; 385(5): 317–23
Kahrilas PJ. Strategies for medical management of reflux disease. Baillieres Clin Gastroenterol 2000 Oct; 15: 775–91
Thjodleifsson B, Jónsson P. Management of gastroesophageal reflux in the elderly patient. Clin Geriatr 2001; 9: 50–6
Richter JE. Gastroesophageal reflux disease in the olderpatient: presentation, treatment, and complications. Am J Gastroenterol 2000; 95(2): 368–73
Dent J, Jones R, Kahrilas P, et al. Management of gastro-oesophageal reflux disease in general practice. BMJ 2001 Feb 10; 322: 344–7
Gillen D, Wirz AA, Ardill JE, et al. Rebound hypersecretion after omeprazole and its relation to on-treatment acid suppression and Helicobacter pylori status. Gastroenterology 1999 Feb; 116: 239–47
Gillen D, Wirz AA, McColl KEL. Eradication of H. pylori unleashes post-PPI rebound acid hypersecretion: relevance to development of GERD [abstract]. Gut 2001 Nov; 49 Suppl. III: 1426
Schwizer W, Thumshirn M, Dent J, et al. Helicobacter pylori and symptomatic relapse of gastro-oesophageal reflux disease: a randomised controlled trial. Lancet 2001 Jun 2; 357: 1738–42
Malaty HM. Helicobacter pylori infection and eradication in paediatric patients. Paediatr Drugs 2000 Sep 31; 2: 357–65
European Helicobacter Pylori Study Group (EHPSG). Current European concepts in the management of Helicobacter pylori infection: the Maastricht Consensus Report. Gut 1997; 41: 8–13
Langtry HD, Wilde M. Lansoprazole: an update of its pharmacological properties and clinical efficacy in the management of acid-related disorders. Drugs 1997 Sep; 54(3): 474–97
Wolfe MM, Sachs G. Acid suppression: optimizing therapy for gastroduodenal ulcer healing, gastroesophageal reflux disease, and stress-related erosive syndrome. Gastroenterology 2000; 118 Suppl. 2: 9–31
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: K Adachi, Shimane Medical University, Department of Internal Medicine II, Izumo, Shimane, Japan; C.M. Bate, Royal Albert Edward Infirmary, Department of Gastroenterology, Wigan, United Kingdom; C. Florent, Hopital Saint-Antoine, Sevice de Gastro-Enterologie, Paris, France; R.T. Jensen, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, Maryland, USA; M. Robinson, University of Oklahoma Health Sciences Center, Oklahoma Foundation for Digestive Research, Oklahoma City, Oklahoma, USA; N Takeguchi, Toyama Medical and Pharmaceutical University, Department of Pharmaceutical Physiology, Toyama, Japan; B. Thjodleifsson, National Hospital, Department of Gastroenterology, Reykjavik, Iceland; A.B.R. Thomson, University of Alberta, Division of Gastroenterology, Edmonton, Alberta, Canada.
Data Selection
Sources: Medical literature published in any language since October 1999 on rabeprazole, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘rabeprazole’ or ‘E 3810’. EMBASE search terms were ‘rabeprazole’ or ‘E 3810’ or ‘LY 307640’. AdisBase search terms were ‘rabeprazole’ or ‘E 3810’ or ‘LY 307640’. Searches were last updated 1 Nov 2001.
Selection: Studies in patients with acid-related gastrointestinal disorders who received rabeprazole. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well designed trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Rabeprazole, acid-related disorders, gastro-oesophageal reflux disease, peptic ulcer disease, Helicobacter pylori infection, pharmacodynamics, pharmacokinetics, therapeutic use.
Rights and permissions
About this article
Cite this article
Carswell, C.I., Goa, K.L. Rabeprazole. Drugs 61, 2327–2356 (2001). https://doi.org/10.2165/00003495-200161150-00016
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200161150-00016