Summary
Abstract
Dalteparin is a low molecular weight heparin (LMWH) with a mean molecular weight of 5000. Compared with unfractionated heparin (UFH), the drug has markedly improved bioavailability and increased plasma elimination half-life, and exerts a greater inhibitory effect on plasma activity of coagulation factor Xa relative to its effects on other coagulation parameters. Dalteparin also has less lipolytic activity than UFH.
Dalteparin 2500U once daily subcutaneously is of similar antithrombotic efficacy to UFH 5000IU twice daily, and 2 studies have shown superiority over UFH 2 or 3 times daily of dalteparin 5000U once daily in patients requiring surgical thromboprophylaxis. After total hip arthroplasty, dalteparin was superior to adjusted-dosage warfarin and was of greater thromboprophylactic efficacy when given for 35 than for 7 days.
Intravenous or subcutaneous dalteparin is as effective as intravenous UFH when given once or twice daily in the initial management of established deep vein thrombosis (DVT). The drug is also effective in long term home treatment. Dalteparin has been shown to be effective in combination with aspirin in the management of unstable coronary artery disease (CAD), with composite end-point data from 1 study suggesting benefit for up to 3 months. Current data indicate potential of the drug in the management of acute myocardial infarction (MI). Dalteparin is also of similar efficacy to UFH, with a single bolus dose being sufficient in some patients, in the prevention of clotting in haemodialysis and haemofiltration circuits.
Pharmacoeconomic data indicate that overall costs relative to UFH from a hospital perspective can be reduced through the use of dalteparin in patients receiving treatment for venous thromboembolism. Dalteparin has also been shown to be cost effective when used for surgical thromboprophylaxis.
Overall, rates of haemorrhagic complications in patients receiving dalteparin are low and are similar to those seen with UFH.
Conclusions: Dalteparin is effective and well tolerated when given subcutaneously once daily in the prophylaxis and treatment of thromboembolic disease. The simplicity of the administration regimens used and the lack of necessity for laboratory monitoring facilitate home or outpatient treatment and appear to translate into cost advantages from a hospital perspective over UFH or warfarin. Dalteparin also maintains the patency of haemodialysis and haemofiltration circuits, with beneficial effects on blood lipid profiles and the potential for prophylaxis with a single bolus injection in some patients. Data are also accumulating to show dalteparin to be an effective and easily administered alternative to UFH in patients with CAD.
Pharmacological Properties
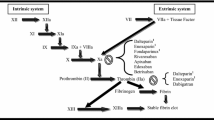
Dalteparin inhibits coagulation factor Xa in human plasma in a dose-dependent manner, with anti-factor Xa activities 2 and 5 times those seen after an intravenous dose of UFH 5000IU being reported after intravenous doses of dalteparin 5000 and 10 000U, respectively. In contrast to UFH, anti-factor Xa activity exceeds anti-factor IIa activity in plasma of individuals who have received dalteparin. The drug also exerts significantly greater effects than UFH on plasma anti-factor Xa activity relative to its effects on other coagulation parameters [including activated partial thromboplastin time (aPTT) and thrombin time]. Dalteparin does not have any clinically relevant effects on plasma antithrombin levels, platelet counts or on the fibrinolytic system, although recent studies show inhibition of thrombin formation in patients with activated haemostatic systems.
Data from healthy volunteers and patients undergoing haemodialysis show less lipolytic activity with dalteparin than with UFH, with reductions in blood levels of total and low density lipoprotein cholesterol and triglycerides being shown with the LMWH.
Dalteparin has monoexponential, first order and dose-independent pharmacokinetic characteristics. Absorption is rate-limiting after subcutaneous administration: peak plasma concentrations (as measured by plasma anti-factor Xa activity) are attained after 2.8 to 4 hours, and the drug undergoes substantially less hepatic and renal deposition than UFH. Bioavailability is 87% and plasma elimination half-life (t½β) 2.4 to 4 hours. t½β after intravenous administration is approximately 2 hours. Elimination takes place predominantly via the kidneys.
The anticoagulant effects of a number of agents (e.g. aspirin, dipyridamole, vitamin K antagonists and non-steroidal anti-inflammatory drugs) may be enhanced by coadministration with dalteparin. The anticoagulant effect of dalteparin may be reduced by the presence of antihistamines, cardiac glycosides, tetracyclines or ascorbic acid.
Therapeutic Use
Surgical Thromboprophylaxis. Randomised and double-blind studies have shown consistently that dalteparin 2500U given subcutaneously once daily for 5 to 13 days is of similar thromboprophylactic efficacy to UFH 5000IU subcutaneously twice daily in patients undergoing general or orthopaedic surgery. Two studies, one in over 800 patients undergoing general surgery and the other with a 6-to 8-week follow-up in 122 patients undergoing orthopaedic surgery, showed dalteparin 5000U once daily subcutaneously to be superior to UFH 5000IU 2 or 3 times daily.
Recent studies have shown that dalteparin 5000U once daily subcutaneously reduces the frequency of venographically evident thromboembolism to a greater extent when given for 35 days than for 7 days in patients undergoing total hip arthroplasty. In 2 double-blind studies (each involving around 200 patients), reductions in incidence of DVT relative to 7-day prophylaxis of 54 and 63% were reported after 35 days’ administration. Dalteparin was also of superior thromboprophylactic efficacy to adjusted-dosage warfarin in patients undergoing total hip arthroplasty.
Two small single-blind studies have been carried out to compare dalteparin with the other LMWHs enoxaparin and nadroparin, but the results of these trials were inconclusive.
Thromboprophylaxis in Pregnancy. Dalteparin has been used successfully with no evidence of any adverse fetal effects in pregnant women at high risk of thromboembolic complications. Dosages were adjusted according to plasma anti-factor Xa activity in these patients. There was an apparently lower risk of bleeding with dalteparin than with UFH in a nonblind comparative study in 105 patients.
Treatment of Established Thromboembolic Disease. Comparative studies have shown intravenous or subcutaneous dalteparin (given once or twice daily) to be of equivalent efficacy in terms of Marder scores and venographic findings to aPTT-adjusted intravenous UFH in patients receiving initial heparin treatment for established DVT. Six-month follow-up data from 1 study showed no significant difference in Marder scores, symptoms or thrombus evolution between patients who received dalteparin 200 U/kg once daily subcutaneously or recipients of continuously infused aPTT-adjusted UFH for 5 to 10 days. Similar conclusions were reported after up to 14 years’ follow-up in patients from 3 Swedish clinical studies in which subcutaneous dalteparin adjusted according to anti-factor Xa activity had been compared with aPTT-adjusted intravenous UFH (either given for at least 5 days pending dosage titration of warfarin).
Noncomparative studies have demonstrated feasibility of initial outpatient treatment of established thromboembolic disease with dalteparin 200 U/kg once daily subcutaneously for at least 4 to 5 days. The drug was also effective and well tolerated when self-administered for 3 months at a dosage of 5000U once daily by patients not eligible for warfarin therapy. In a 3-month nonblind comparison, there was no statistically significant difference in efficacy between long term dalteparin 5000U once daily subcutaneously and warfarin in 86 patients with thromboembolic disease.
Coronary Artery Disease. Dalteparin 7500U once daily subcutaneously plus aspirin (n = 562) was of similar efficacy to aspirin alone (n = 561) in terms of a composite end-point of death, MI or recurrence of angina over 39 days of double-blind placebo-controlled treatment in a study in patients with unstable CAD. Equivalence of dalteparin 120 U/kg twice daily subcutaneously and aPTT-ad-justed UFH infusion (in terms of rates of death or MI, need for coronary revas-cularisation or recurrence of angina) was suggested by the results of an initial 6-day nonblind phase in 1482 patients.
In the first of 2 randomised double-blind studies carried out by the Swedish Fragmin and Fast Revascularisation in Coronary Artery Disease (FRISC) study group, significantly lower rates of death and new MI and reduced need for revascularisation or intravenous heparin were reported after 6 days’ treatment with dalteparin 120 U/kg subcutaneously twice daily (n = 746) than with placebo (n = 760). Subgroup analyses suggested maintenance of benefit at 40 days with dalteparin 7500 U/day in non-smokers, patients with non-Q-wave MI and those with body mass index below 26 kg/m2. There was no significant difference from placebo after 4 to 5 months.
A second study carried out by the FRISC group in 2267 patients with unstable CAD showed a 47% decrease (p = 0.002) relative to placebo in a combined end-point of death and MI after the first month of a 3-month period of double-blind treatment with dalteparin 5000 or 7500U twice daily. When a triple end-point of death, MI and need for revascularisation was considered for both the 3-month double-blind treatment period and an initial 5-to 7-day nonblind phase (in which all patients received dalteparin), there were significant differences in favour of dalteparin after 1 month and 3 months. Subgroup analyses have suggested a link between efficacy of dalteparin in the longer term and raised levels of the cardiac marker troponin-T.
Outcomes were not affected by dalteparin therapy in a further comparative study in which percutaneous coronary intervention was shown to be superior to non-invasive therapy in 2457 patients with unstable CAD.
In a randomised double-blind study in 517 patients with acute anterior MI, there was a statistically significant 35% reduction versus placebo in a combined end-point of left ventricular thrombus formation or arterial thromboembolism with dalteparin 150 U/kg twice daily subcutaneously for 7 to 11 days after thrombol-ysis with streptokinase. In another double-blind study in 101 patients with acute MI, dalteparin 100 U/kg before and 12 hours after streptokinase thro mbolysis had no effect on rates of death or reinfarction or other cardiac events, although significantly fewer dalteparin than placebo recipients had ECG evidence of ischaemia from 6 to 24 hours after starting treatment. Preliminary results from a study in 1128 patients with acute MI who were not eligible for thrombolysis indicate short term (3-day) but not long term (30-or 90-day) benefit of subcutaneous dalteparin 120 U/kg twice daily.
Haemodialysis and Haemofiltration. Dalteparin was of similar efficacy to UFH in the maintenance of patency of haemodialysis and haemofiltration circuits in studies in which heparin was administered as an intravenous bolus followed by continuous infusion. Initial doses of dalteparin ranged from 2500 to 5000U; those of UFH ranged from 2000 to 5000IU. Infusions were given at fixed hourly rates or were adjusted according to bodyweight or whole blood activated clotting times. Dalteparin prevented blood clot formation in dialysers to a similar extent to tinzaparin, and was associated with similar haemofilter survival times to nadroparin, in comparative studies. Data are also available to show equivalent efficacy of a single bolus of dalteparin (given at the start of haemodialysis) and continuously infused UFH.
Ischaemic Stroke. Dalteparin has not been shown to have any significant advantage over aspirin on cerebral end-points in patients with acute ischaemic stroke. Outcomes were similar in patients treated with dalteparin 100 U/kg twice daily subcutaneously and in those receiving aspirin 160mg daily (orally or rectally) in a recent placebo-controlled double-blind trial in 449 patients with atrial fibrillation and ischaemic stroke.
Pharmacoeconomic Considerations
A retrospective comparison using results from 434 patients, 80.2% of whom received home treatment with subcutaneous dalteparin 200 U/kg once daily for initial management of established DVT, showed a 34.5% reduction relative to inpatient treatment in Swedish mean hospital and treatment costs (1996 values). Australian researchers estimated overall per-patient treatment costs (year not stated) to be reduced by $A1239 when initial DVT treatment with dalteparin 200 U/kg once daily was given at home rather than in hospital.
Canadian and Spanish data indicate overall institutional cost savings when dalteparin is used in place of UFH in the initial management of DVT in hospital. In addition, a brief pharmacoeconomic report from a UK study in 105 patients showed a £900 per-patient overall cost saving when subcutaneous dalteparin 5000U once daily rather than laboratory-adjusted warfarin therapy was given for 3 months for the prevention of recurrence of DVT.
Significantly lower rates of DVT with subcutaneous dalteparin 5000U once daily than with laboratory-adjusted warfarin for a mean 7 days translated into similar average cost effectiveness of dalteparin and warfarin in terms of cost per event-free patient in a pharmacoeconomic analysis of 382 individuals receiving thromboprophylaxis after total hip arthroplasty. Overall costs per patient from a hospital perspective were similar under different treatment scenarios (short term (6-day) and long term (35-day) treatment started before or after surgery) for dalteparin and warfarin in a North American study in which 1130 patients were randomised to prophylaxis with either drug after total hip arthroplasty. Incremental cost effectiveness of dalteparin ranged from $US 1799 to $US4661 per patient (year of costing not stated) in this analysis.
Economic data from a 9-week time and motion study in 116 patients receiving aPTT-adjusted UFH infusion for acute CAD showed costs from a hospital perspective of $Can25.68 for UFH and $Can28.82 for dalteparin 120 U/kg twice daily subcutaneously. In this analysis, costs for dalteparin therapy were estimated using a projection based on assumptions regarding resource utilisation, staff activity and acquisition cost.
Tolerability
Overall, rates of haemorrhagic complications appear similar for dalteparin and UFH in patients receiving thromboprophylaxis and those undergoing treatment for established thromboembolic disease. Collated data from studies in surgical patients receiving subcutaneous thromboprophylaxis with dalteparin 2500 or 5000U or UFH 10 000IU daily show similar rates of bleeding with either heparin. Increased frequency of bleeding complications relative to placebo has been reported in patients undergoing treatment with dalteparin for up to 3 months for unstable CAD; in patients receiving acute treatment for MI in 1 study, major haemorrhage was reported in 2.9% of dalteparin recipients and 0.3% of those receiving placebo (p = 0.006). There have been no reports of excess bleeding relative to placebo in patients receiving extended (35-day) thromboprophylaxis with dalteparin after orthopaedic surgery, and the drug has not been associated with clinically significant haemorrhagic complications or adverse fetal or maternal outcomes in pregnant women.
The exact incidence of thrombocytopenia with dalteparin is not known, but has been reported to be less than 1% in patients receiving the drug for thromboprophylaxis.
Dosage and Administration
Patients at moderate risk of venous thromboembolism after surgery should receive dalteparin subcutaneously at a dosage of 2500U once daily; patients at high risk should receive 5000U once daily. A dosage of 200 U/kg once daily or 100 U/kg twice daily is recommended for the initial treatment of established thromboembolic disease, and 120 U/kg every 12 hours in addition to aspirin is indicated for patients with unstable CAD. An intravenous weight-adjusted bolus followed by continuous infusion is recommended for haemodialysis or haemo-filtration procedures lasting 4 hours or more; a single intravenous bolus may be suitable where sessions are of less than 4 hours’ duration. Subcutaneous administration of dalteparin should be via the abdomen or the lateral portion of the thigh.
Laboratory monitoring of the coagulation response is not necessary in most patients receiving dalteparin therapy. Plasma anti-factor Xa activity should be monitored in certain groups of individuals, however; these include those with acute or chronic renal failure, and those at high risk of bleeding who require treatment for established thromboembolic disease.












Similar content being viewed by others
References
Pineo GF, Hull RD. Unfractionated and low-molecular-weight heparin: comparisons and current recommendations. Med Clin North Am 1998; 82(3): 587–99
Hirsh J, Warkentin TE, Raschke R, et al. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacoki-netics, dosing considerations, monitoring, efficacy, and safety. Chest 1998; 114(5) Suppl.: 489S–510S
Dunn CJ, Sorkin EM. Dalteparin sodium. A review of its pharmacology and clinical use in the prevention and treatment of thromboembolic disorders. Drugs 1996 Aug; 52: 276–305
Wolf H. Low-molecular-weight heparin. Med Clin North Am 1994; 78(3): 733–43
Dalteparin sodium. In: McEvoy GK, editor. AHFS drug information. Bethesda, MD: American Society of Health-System Pharmacists, 1999: 1253–5
Fragmin ampoules. In: Walker G, editor. ABPI compendium of data sheets and summaries of product characteristics 1998–99. London: Datapharm Publications Ltd, 1998: 1000–1
Holmer E, Söderberg K, Bergqvist D, et al. Heparin and its low molecular weight derivatives: anticoagulant and antithrom-botic properties. Haemostasis 1986; 16 Suppl. 2: 1–7
Barrowcliffe TW, Curtis AD, Johnson EA, et al. An international standard for low molecular weight heparin. Thromb Haemost 1988; 60: 1–7
Agnelli G, Bonn J, Cosmi B, et al. Effects of standard heparin and a low molecular weight heparin (Kabi 2165) on fibrinolysis. Thromb Haemost 1988 Oct 31; 60: 311–3
Andrassy K, Mörike K, Koderisch J, et al. Human pharmacological studies of a defined low molecular weight heparin fraction (Fragmin®) evidence for a simultaneous inhibition of factor Xa and IIa (thrombin). Thromb Res 1988 Mar 15; 49: 601–11
Mätzsch T, Bergqvist D, Burmark US, et al. The influence of surgical trauma on factor XaI and IIaI activity and heparin concentration after a single dose of low-molecular-weight heparin. Blood Coagul Fibrinolysis 1991 Oct; 2: 651–7
Bara L, Combe-Tamzali S, Conard J, et al. Comparative biological modifications induced by 3 low molecular weight heparins, PK 10169, Kabi 2165 and CY 216 and a non-fractionated heparin, injected subcutaneously in healthy volunteers, general surgery patients and elderly patients with medical disorders [in French]. J Mal Vasc 1987; 12 Suppl. B: 78–84
Eriksson BI, Söderberg K, Widlund L, et al. A comparative study of three low-molecular weight heparins (LMWH) and unfractionated heparin (UH) in healthy volunteers. Thromb Haemost 1995 Mar; 73: 398–401
Eriksson E, Wollter IM, Christenson B, et al. Heparin and fibrinolysis —comparison of subcutaneous administration of unfractionated and low molecular weight heparin. Thromb Haemost 1988 Apr 8; 59: 284–8
Eriksson BI, Zachrisson BE, Teger-Nilsson A-C, et al. Thrombosis prophylaxis with low molecular weight heparin in total hip replacement. Br J Surg 1988 Nov; 75: 1053–7
Ockelford PA, Patterson J, Johns AS. A double-blind randomized placebo controlled trial of thromboprophylaxis in major elective general surgery using once daily injections of a low molecular weight heparin fragment (Fragmin). Thromb Haemost 1989 Dec 29; 62: 1046–9
Prins MH, Gelsema R, Sing AK, et al. Prophylaxis of deep venous thrombosis with a low-molecular-weight heparin (Kabi 2165/Fragmin®) in stroke patients. Haemostasis 1989; 19(5): 245–50
Onarheim H, Lund T, Heimdal A, et al. A low molecular weight heparin (KABI 2165) for prophylaxis of postoperative deep venous thrombosis. Acta Chir Scand 1986 Oct; 152: 593–6
Caen JP. A randomized double-blind study between a low molecular weight heparin Kabi 2165 and standard heparin in the prevention of deep vein thrombosis in general surgery. A French multicenter trial. Thromb Haemost 1988 Apr 8; 59: 216–20
Koller M, Schoch U, Buchmann P, et al. Low molecular weight heparin (KABI 2165) as thromboprophylaxis in elective visceral surgery. A randomized, double-blind study versus unfractionated heparin. Thromb Haemost 1986 Dec 15; 56(3): 243–6
Bergqvist D, Burmark US, Frisell J, et al. Prospective double-blind comparison between Fragmin and conventional low-dose heparin: thromboprophylactic effect and bleeding complications. Haemostasis 1986; 16 Suppl. 2: 11–8
Schrader J, Stibbe W, Armstrong VW, et al. Comparison of low molecular weight heparin to standard heparin in hemodialysis/hemofiltration. Kidney Int 1988; 33: 890–6
Padilla A, Gray E, Pepper DS, et al. Inhibition of thrombin generation by heparin and low molecular weight (LMW) heparins in the absence and presence of platelet factor 4 (PF4). Br J Haematol 1992 Oct; 82: 406–13
O’Brien JR, Etherington MD, Pashley MA. The heparin-mobilisable pool of platelet factor 4: a comparison of intravenous and subcutaneous heparin and Kabi heparin fragment 2165. Thromb Haemost 1985 Dec 17; 54: 735–8
Andersen BS. Postoperative activation of the haemostatic system —influence of prolonged thromboprophylaxis in patients undergoing total hip arthroplasty. Haemostasis 1997 Sep–Oct; 27: 219–27
Wolzt M, Eder M, Weltermann A, et al. Comparison of the effects of different low molecular weight heparins on the hemostatic system activation in vivo in man. Thromb Haemost 1997 Aug; 78: 876–9
Ernofsson M, Strekerud F, Toss H, et al. Low-molecular weight heparin reduces the generation and activity of thrombin in unstable coronary artery disease. Thromb Haemost 1998 Mar; 79: 491–4
Myrmel T, Larsen TS, Reikerås O. Lipolytic effect of low-molecular-weight-heparin (Fragmin®) and heparin/dihydroer-gotamine in thromboprophylactic doses during total hip replacement. Scand J Clin Lab Invest 1992 Nov; 52: 741–5
Schmitt Y, Schneider H. Low-molecular-weight heparin (LMWH): influence on blood lipids in patients on chronic haemodialysis. Nephrol Dial Transplant 1993; 8(5): 438–42
Persson E. Lipoprotein lipase, hepatic lipase and plasma lipolytic activity. Effects of heparin and a low molecular weight heparin fragment (Fragmin). Acta Med Scand Suppl 1988; 724: 1–56
Persson E, Nordenström J, Hagenfeldt L, et al. Plasma lipolytic activity after subcutaneous administration of heparin and a low molecular weight heparin fragment. Thromb Res 1987; 46: 697–704
Deuber HJ, Schulz W. Reduced lipid concentrations during four years of dialysis with low molecular weight heparin. Kidney Int 1991; 40: 496–500
Schmitt Y, Schneider H. The influence of low molecular weight heparin on blood lipoproteins in patients on chronic hemodialysis [abstract]. Atherosclerosis 1997 1–2, Oct No; 134: 49
Lüders S, Kandt M, Schrader J. Low molecular weight heparin versus standard heparin in patients with hypertriglyceridemia on hemodialysis-5 years follow-up [abstract]. Nephrol Dial Transplant 1996 Jun; 11: A221
Bratt G, Törnebohm E, Lockner D, et al. A human pharmacological study comparing conventional heparin and a low molecular weight heparin fragment. Thromb Haemost 1985; 53: 208–11
Bratt G, Törnebohm E, Widlund L, et al. Low molecular weight heparin (KABI 2165, Fragmin): pharmacokinetics after intravenous and subcutaneous administration in human volunteers. Thromb Res 1986 Jun 1; 42: 613–20
Dryjski M, Schneider DE, Mojaverian P, et al. Investigations on plasma activity of low molecular weight heparin after intravenous and oral administrations. Br J Clin Pharmacol 1989 Aug; 28: 188–92
Collignon F, Frydman A, Caplain H, et al. Comparison of the pharmacokinetic profiles of three low molecular mass heparins —dalteparin, enoxaparin and nadroparin —administered subcutaneously in healthy volunteers (doses for prevention of thromboembolism). Thromb Haemost 1995 Apr; 73: 630–40
Simoneau G, Bergmann JF, Kher A, et al. Pharmacokinetics of a low molecular weight heparin [Fragmin] in young and elderly subjects. Thromb Res 1992 Jun 1; 66: 603–7
Palm M, Mattsson C. Pharmacokinetics of heparin and low molecular weight heparin fragment (Fragmin) in rabbits with impaired renal or metabolic clearance. Thromb Haemost 1987 Oct 28; 58: 932–5
Jørgensen B, Nielsen C, Rasmussen LH. Erythrocyte adhesion affects the bioavailability of low-molecular-weight heparin [abstract]. Haemostasis 1998 Nov; 28 Suppl. 3: 134
Stiekema JCJ, van Griensven JM, van Dinther TG, et al. Across-over comparison of the anti-clotting effects of three low molecular weight heparins and glycosaminoglycuronan. Br J Clin Pharmacol 1993 Jul; 36: 51–6
Greer IA, Gibson JL, Young A, et al. Effect of ketorolac and low molecular weight heparin individually and in combination on haemostasis. Blood Coagul Fibrinolysis 1998 Nov; 10: 367–73
Bergqvist D. Modern aspects of prophylaxis and therapy for venous thrombo-embolic disease. Aust N Z J Surg 1998; 68(7): 463–8
Thromboembolic Risk Factors (THRIFT) Consensus Group. Risk of and prophylaxis for venous thromboembolism in hospital patients. BMJ 1992 Sep 5; 305: 567–74
Flordal PA, Bergqvist D, Burmark US, et al. Risk factors for major thromboembolism and bleeding tendency after elective general surgical operations. Eur J Surg 1996 Oct; 162: 783–9
Nurmohamed MT, Rosendaal FR, Büller HR, et al. Low-molecular-weight heparin versus standard heparin in general and orthopaedic surgery: a meta-analysis. Lancet 1992 Jul 18; 340: 152–6
Nurmohamed MT, Büller HR, ten Cate JW. Physiological changes due to age: implications for the prevention and treatment of thrombosis in older patients. Drugs Aging 1994 Jul; 5(1): 20–33
Bergqvist D, Mätzsch T, Burmark US, et al. Low molecular weight heparin given the evening before surgery compared with conventional low-dose heparin in prevention of thrombosis. Br J Surg 1988 Sep; 75(9): 888–91
Eriksson BI, Kälebo P, Anthmyr B A, et al. Prevention of deep-vein thrombosis and pulmonary embolism after total hip replacement. J Bone Joint Surg Am 1991 Apr; 73A(4): 484–93
Francis CW, Pellegrini Jr VD, Totterman S, et al. Prevention of deep-vein thrombosis after total hip arthroplasty. Comparison of warfarin and dalteparin. J Bone Joint Surg Am 1997 Sep; 79: 1365–72
Pineo GF, Hull RD. A double-blind randomized comparison of low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery [abstract]. Blood 1999; 94 Suppl. 1 (Pt 1): 30a
Hull RD, Pineo GF. A double-blind, randomized comparison of low-molecular-weight heparin prophylaxis using dalteparin extended out-of-hospital versus warfarin-placebo in hiparthroplasty patients [abstract]. Blood 1999; 94 Suppl. 1 (Pt 1): 29a
Dahl OE, Andreassen G, Aspelin T, et al. Prolonged thromboprophylaxis following hip replacement surgery —results of a double-blind, prospective, randomised, placebo-controlled study with dalteparin (Fragmin). Thromb Haemost 1997 Jan; 77: 26–31
Lassen MR, Borris LC, Anderson BS, et al. Efficacy and safety of prolonged thromboprophylaxis with a low molecular weight heparin (dalteparin) after total hip arthroplasty —the Danish Prolonged Prophylaxis (DaPP) Study. Thromb Res 1998 Mar 15; 89: 281–7
Hartl P, Brücke P, Dienstl E, et al. Prophylaxis of thromboembolism in general surgery: comparison between standard heparin and Fragmin. Thromb Res 1990 Feb 15; 57: 577–84
Kakkar VV, Cohen AT, Edmondson RA. Low molecular weight versus standard heparin for prevention of venous thromboembolism after major abdominal surgery. Lancet 1993 Jan 30; 341: 259–65
Ward B, Pradhan S. Comparison of low molecular weight heparin (Fragmin) with sodium heparin for prophylaxis against postoperative thrombosis in women undergoing major gynaecological surgery. Aust NZ J Obstet Gynaecol 1998 Feb; 38: 91–2
Kollár L, Scholz ME, Roszos I. Comparison of pentosan polysulfate sodium (Na-PPS) with a low-molecular-weight heparin in the prevention of venous thrombosis after abdominal surgery. Perfusion 1994 Apr; 7(4): 123–30
Bounameaux H, Huber O, Khabiri E, et al. Unexpectedly high rate of phlebographic deep venous thrombosis following elective general abdominal surgery among patients given prophylaxis with low-molecular-weight heparin. Arch Surg 1993 Mar; 128: 326–8
Røise O, Nurmohamed M, Reijnders P, et al. A multicentre, randomised, assessor-blind, pilot study comparing the efficacy in the prophylaxis of DVT and the safety of Orgaran (Org 10172), Fragmin, Clexane/Lovenox in patients undergoing surgery for a fractured hip [abstract]. Thromb Haemost 1993 Jun; 69(6): 620
Hunt BJ, Doughty HA, Majumdar G, et al. Thrombopro-phylaxis with low molecular weight heparin (Fragmin) in high risk pregnancies. Thromb Haemost 1997 Jan; 77: 39–43
Pettilä V, Kaaja R, Leinonen P, et al. Thromboprophylaxis with low molecular weight heparin (Dalteparin) in pregnancy. Thromb Res 1999; 96(4): 275–82
Blombäck M, Bremme K, Hellgren M, et al. Thromboprophylaxis with low molecular mass heparin, ‘Fragmin’ (dalteparin), during pregnancy —a longitudinal safety study. Blood Coagul Fibrinolysis 1998 Jan; 9: 1–9
Geisen U, Abou-Mandour N, Grossman R, et al. Long-term thromboprophylaxis with low-molecular-weight-heparin (dalteparin) in high-risk pregnancies [abstract]. Haemostasis 1998 Nov;28 Suppl. 3: 137
Charland SL, Klinter DEJ. Low-molecular-weight heparins in the treatment of pulmonary embolism. Ann Pharmacother 1998; 32(2): 258–64
Marder VJ, Soulen RL, Atichartakarn V, et al. Quantitative venographic assessment of deep vein thrombosis in the evaluation of streptokinase and heparin therapy. J Lab Clin Med 1977; 89(5): 1018–29
Albada J, Nieuwenhuis HK, Sixma JJ. Treatment of acute venous thromboembolism with low molecular weight heparin (Fragmin). Results of a double-blind randomized study. Circulation 1989 Oct; 80: 935–40
Lockner D, Bratt G, Törnebohm E, et al. Intravenous and subcutaneous administration of Fragmin in deep venous thrombosis. Haemostasis 1986; 16 Suppl. 2: 25–9
Aiach M, Fiessinger JN, Vitoux JF, et al. Deep vein thrombosis treatment. A comparative study: subcutaneous Fragmin versus unfractionated heparin administered by continuous infusion. Multicenter trial [in French]. Rev Med Interne 1989 Jul–Aug; 10: 375–81
Bratt G, Aberg W, Johansson M, et al. Two daily subcutaneous injections of Fragmin as compared with intravenous standard heparin in the treatment of deep vein thrombosis (DVT). Thromb Haemost 1990 Dec 28; 64: 506–10
Fiessinger J-N, Lopez-Fernandez M, Gatterer E, et al. Once-daily subcutaneous dalteparin, a low molecular weight heparin, for the initial treatment of acute deep vein thrombosis. Pharmacia & Upjohn (Stockholm). Data on file
Holm HA, Ly B, Handeland GF, et al. Subcutaneous heparin treatment of deep vein thrombosis: a comparison of unfractionated and low molecular weight heparin. Haemostasis 1986; 16 Suppl. 2: 30–7
Lindmarker P, Holmström M, Granqvist S. Comparison of once-daily subcutaneous Fragmin® with continuous intravenous unfractionated heparin in the treatment of deep vein thrombosis. Thromb Haemost 1994 Aug; 72: 186–90
Luomanmäki K, Grankvist S, Hallert C, et al. A multicentre comparison of once-daily subcutaneous dalteparin (low molecular weight heparin) and continuous intravenous heparin in the treatment of deep vein thrombosis. Pharmacia & Upjohn (Stockholm). Data on file
Luomanmäki K, Grankvist S, Hallert C, et al. A multicentre comparison of once-daily subcutaneous dalteparin (low molecular weight heparin) and continuous intravenous heparin in the treatment of deep vein thrombosis. J Intern Med 1996 Aug; 240: 85–92
Fiessinger JN, Lopez-Fernandez M, Gatterer E, et al. Once-daily subcutaneous dalteparin, a low molecular weight heparin, for the initial treatment of acute deep vein thrombosis. Thromb Haemost 1996; 76(2): 195–9
Meyer G, Brenot F, Pacouret G, et al. Subcutaneous low-molecular-weight heparin fragmin versus intravenous unfractionated heparin in the treatment of acute non massive pulmonary embolism: an open randomized pilot study. Thromb Haemost 1995 Dec; 74: 1432–5
Holmström M, Lindmarker P, Granqvist S, et al. A 6-month venographic follow-up in 164 patients with acute deep vein thrombosis. Thromb Haemost 1997 Aug; 78: 803–7
Holmström M, Åberg W, Lockner D, et al. Long-term clinical follow-up in 265 patients with deep venous thrombosis initially treated with either unfractionated heparin or dalteparin: a retrospective analysis. Thromb Haemost 1999; 82(4): 1222–6
Bick RL. Low molecular weight heparins in the outpatient management of venous thromboembolism. Semin Thromb Hemost 1999; 25 Suppl. 3: 97–9
Büller HR. Outpatient therapy with low-molecular-weight heparins: new perspectives for treatment of deep vein thrombosis. Haemostasis 1998; 28 Suppl. 3: 91–4
Lindmarker P, Holmström M. Use of low molecular weight heparin (dalteparin), once daily, for the treatment of deep vein thrombosis. A feasibility and health economic study in an outpatient setting. Swedish Venous Thrombosis Dalteparin Trial Group. J Intern Med 1996 Dec; 240: 395–401
Savage KJ, Wells PS, Schulz V, et al. Outpatient use of low molecular weight heparin (dalteparin) for the treatment of deep vein thrombosis of the upper extremity. Thromb Haemost 1999; 82(3): 1008–10
Kovacs MJ, Anderson D, Morrow B, et al. Outpatient treatment of pulmonary embolism with dalteparin. Thromb Haemost 2000 Feb; 83: 209–11
Ting SB, Ziegenbein RW, Gan TE, et al. Dalteparin for deep venous thrombosis: a hospital-in-the-home program. Med J Aust 1998 Mar 16; 168: 272–6
Wilson SJ, Gray L, Anderson DR. Outpatient treatment of deep vein thrombosis and pulmonary embolism: a hospital-based program. Can J Hosp Pharm 1999; 52(5): 282–8
Stockelberg D, Jonsson T, Hansson E. Long term follow up of patients with deep vein thrombosis treated in an outpatient setting [abstract]. Thromb Haemost 1997 Jun Suppl.: 288–9
Wells PS, Kovacs MJ, Bormanis J, et al. Expanding eligibility for outpatient treatment of deep venous thrombosis and pulmonary embolism with low-molecular-weight heparin: a comparison of patient self-injection with homecare injection. Arch Intern Med 1998 Sep 14; 158: 1809–12
Bick RL, Rice J. Long-term outpatient dalteparin (Fragmin) therapy for arterial and venous thrombosis: efficacy and safety -a preliminary report. Clin Appl Thrombosis/Hemostasis 1999; 5 Suppl. 1: S67–71
Das SK, Cohen AT, Edmondson RA, et al. Low-molecular-weight heparin versus warfarin for prevention of recurrent venous thromboembolism: a randomized trial. World J Surg 1996; 20(5): 521–7
Campbell RWF, Wallentin L, Verheugt FWA, et al. Management strategies for a better outcome in unstable coronary artery disease. Clin Cardiol 1998; 21(5): 314–22
Brieger DB, Freedman SB. Low molecular weight heparins: promising therapy for unstable angina and non-Q wave myocardial infarction. Asia Pacific Heart J 1997; 6(3): 173–7
Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) Study investigators. A comparison of aspirin plus tirofiban with aspirin plus heparin for unstable angina. N Engl JMed 1998; 338: 1498–505
Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) Study investigators. Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q-wave myocardial infarction. N Engl J Med 1998; 338: 1488–97
The PURSUIT Trial Investigators. Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. N Engl J Med 1998; 339: 436–43
Goa KL, Noble S. Eptifibatide: a review of its use in patients with acute coronary syndromes and/or undergoing percutaneous coronary intervention. Drugs 1999 Mar; 57(3): 439–62
RISC group. Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. Lancet 1990; 336: 827–30
Oler A, Whooley MA, Oler J, et al. Adding heparin to aspirin reduces the incidence of myocardial infarction and death in patients with unstable angina. A meta-analysis. JAMA 1996; 276(10): 811–5
Théroux P, Waters D, Lam J, et al. Reactivation of unstable angina after the discontinuation of heparin. N Engl J Med 1992; 327(3): 141–5
Klein W, Buchwald A, Hillis SE, et al. Comparison of low-molecular-weight heparin with unfractionated heparin acutely and with placebo for 6 weeks in the management of unstable coronary artery disease. Fragmin in unstable coronary artery disease study (FRIC). Circulation 1997 Jul 1; 96: 61–8
Fragmin During Instability in Coronary Artery Disease (FRISC) study group. Low-molecular-weight heparin during instability in coronary artery disease. Lancet 1996 Mar 2; 347: 561–8
Fragmin and Fast Revascularisation During Instability in Coronary Artery Disease (FRISC II) investigators. Long-term low-molecular-mass heparin in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. Lancet 1999 Aug 28; 354: 701–7
Lindahl B, Venge P, Wallentin L. Troponin T identifies patients with unstable coronary artery disease who benefit from long-term antithrombotic protection. J Am Coll Cardiol 1997 Jan; 29: 43–8
Lindahl B, Diderholm E, Kontny F, et al. Long term treatment with low molecular weight heparin (dalteparin) reduces cardiac events in unstable coronary artery disease with troponin-T elevation: a FRISCH substudy [abstract]. Circulation 1999 Nov 2; l00 Suppl. 1: 498
Beller GA. Diagnosis and management of patients with unstable angina. Curr Probl Cardiol 1999; 24(11): 687–744
Fragmin and Fast Revascularisation During Instability in Coronary Artery Disease (FRISC II) investigators. Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. Lancet 1999 Aug 28; 354: 708–15
Frostfeldt G, Ahlberg G, Gustafsson G, et al. Low molecular weight heparin (dalteparin) as adjuvant treatment of thrombolysis in acute myocardial infarction —a pilot study: biochemical markers in acute coronary syndromes (BIOMACS II). J Am Coll Cardiol 1999 Mar; 33: 627–33
Bleich SD, Nichols TC, Schumacher RR, et al. Effect of heparin on coronary arterial patency after thrombolysis with tissue plasminogen activator in acute myocardial infarction. J Am Coll Cardiol 1990; 66: 1412–7
Kontny F, Dale J, Abildgaard U, et al. Randomized trial of low molecular weight heparin (dalteparin) in prevention of left ventricular thrombus formation and arterial embolism after acute anterior myocardial infarction: the Fragmin in Acute Myocardial Infarction (FRAMI) Study. J Am Coll Cardiol 1997 Oct; 30: 962–9
Kakkar VV, Iyengar SS, de Lorenzo F. Multicentre randomised prospective trial of LMWH (Dalteparin sodium —Fragmin®) in acute myocardial infarction. Blood 1999; 94 Suppl. 1 (Pt 2): 106b
Beijering RJR, Ten Cate H, Nurmohamed MT, et al. Anticoagulants and extracorporeal circuits. Semin Thromb Hemost 1997; 23(2): 225–33
Anastassiades E, Ireland H, Flynn A, et al. A low-molecular-weight heparin (KABI 2165, ‘Fragmin’) in repeated use for haemodialysis: prevention of clotting and prolongation of the venous compression time in comparison with commercial unfractionated heparin. Nephrol Dial Transplant 1990 Feb; 5: 135–40
Bonn JJJ, Krediet R, Sturk A, et al. Heparin versus low molecular weight heparin K 2165 in chronic hemodialysis patients: a randomized cross-over study. Haemostasis 1986; 16 Suppl. 2: 59–68
Kerr PG, Mattingly S, Lo A, et al. The adequacy of Fragmin as a single bolus dose with reused dialyzers. Artif Organs 1994 Jun; 18: 416–9
Ljungberg B, Blombäck M, Johnsson H, et al. A single dose of a low molecular weight heparin fragment for anticoagulation during hemodialysis. Clin Nephrol 1987 Jan; 27: 31–5
Suzuki T, Ota K, Naganuma S, et al. Clinical application of Fragmin (FR-860) in hemodialysis: multicenter cooperative study in Japan. Semin Thromb Hemost 1990 Oct; 16 Suppl.: 46–54
Reeves JH, Cumming AR, Gallagher L, et al. A controlled trial of low-molecular-weight heparin (dalteparin) versus unfractionated heparin as anticoagulant during continuous venovenous hemodialysis with filtration. Crit Care Med 1999; 27(10): 2224–8
Kwon TH, Kim YL, Cho DK. A comparison of low molecular weight heparin with unfractionated heparin for anticoagulation during hemodialysis [abstract]. Kidney Int 1997 Mar; 51(3): 953
Beijering RJR, Stevens P, Vanholder R, et al. First randomized longterm comparative clinical trial for efficacy and safety of two LMWH in hemodialysis: tinzaparin versus dalteparin [abstract]. Nephrol Dial Transplant 1998 Jun; 13: A179
de Pont AC, Oudemans van Straaten HM, Roozendaal KJ, et al. Nadroparin versus dalteparin anticoagulation in high-volume, continuous venovenous hemofiltration: a double-blind, randomized, crossover study. Crit Care Med 2000; 28(2): 421–5
Bonita R. Epidemiology of stroke. Lancet 1992; 339: 342–4
Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy —I: prevention of death, myocardial infarction, and stroke by prolonged anti-platelet therapy in various categories of patients. BMJ 1994; 308: 81–106
Berge E, Abdelnoor M, Nakstad PH, et al. Low molecular-weight heparin versus aspirin in patients with acute ischaemic stroke and atrial fibrillation: a double-blind randomised study. Lancet 2000; 355: 1205–10
Heaton D, Pearce M. Low molecular weight versus un-fractionated heparin: a clinical and economic appraisal. PharmacoEconomics 1995 Aug; 8: 91–9
Pleil A, Calais M, Vreeland M, et al. An economic assessment of dalteparin versus warfarin in total hip replacement [abstract]. Value Health 1999 Sep–Oct; 2(5): 350–1
Williamson TE. Outpatient DVT treatment with Fragmin® can result in cost and bed savings [abstract]. Am J Managed Care 1997; 3(3) Suppl.: S60–3
Soto Alvarez J, Fernández Cano P. Evaluación económica del uso de dalteparina sódica versus heparina no fraccionada en el tratamiento de la trombosis venosa profunda. Farm Hosp 1997; 21(2): 111–6
Francis CW, Pleil AM, Reinhart SP, et al. A pharmacoeconomic evaluation of low-molecular-weight heparin in patients after total hip-replacement surgery. Pharmacol Ther 1999; 24(3): 136–45
Paradiso-Hardy FL, Oh P. The cost of unfractionated and low-molecular weight heparin in the management of acute coronary syndromes. Can J Hosp Pharm 1999; 52(2): 72–6
Dalteparin sodium. In: Mosby’s GenRx: the complete reference for generic and brand drugs. 9th ed. St Louis, MO: Mosby, 1999: II-603-II-604
Richter C, Huch A, Huch R. Transfer of low molecular heparin during breast feeding [abstract]. Thromb Haemost 1997 Jun Suppl.: 734
Monreal M, Olive A, Lafoz E. Heparins, coumarin, and bone density [letter]. Lancet 1991 Sep 14; 338: 706
Nishiyama M, Itoh F, Ujiie A. Low-molecular-weight heparin (dalteparin) demonstrated a weaker effect on rat bone metabolism compared with heparin. Jpn J Pharmacol 1997 May; 74: 59–68
Kikta MJ, Keller MP, Humphrey PW, et al. Can low molecular weight heparins and heparinoids be safely given to patients with heparin-induced thrombocytopenia syndrome? Surgery 1993 Oct; 114: 705–10
Greinacher A, Michels I, Mueller-Eckhardt C. Heparin-associated thrombocytopenia: the antibody is not heparin specific. Thromb Haemost 1992 May 4; 67: 545–9
Makhoul RG, Greenberg CS, McCann RL. Heparin-associated thrombocytopenia and thrombosis: a serious clinical problem and potential solution. J Vasc Surg 1986; 4: 522–8
Greinacher A, Michels I, Kiefel V, et al. A rapid and sensitive test for diagnosing heparin-associated thrombocytopenia. Thromb Haemost 1991; 66(6): 734–6
Messmore Jr HL, Griffin B, Fareed J, et al. In-vitrostudies of the interaction of heparin, low molecular weight heparin and heparinoids with platelets. Ann N Y Acad Sci 1989; 556: 217–31
Cohen M. Heparin-induced thrombocytopenia and the clinical use of low molecular weight heparins in acute coronary syndromes. Semin Hematol 1999; 36 Suppl. 1: 33–6
Farag SS, Savoia H, O’Malley CJ, et al. Lack of invitrocross-reactivity predicts safety of low-molecular weight heparins in heparin-induced thrombocytopenia. Clin Appl Thrombosis/Hemostasis 1997; 3(1): 58–62
Fragmin multidose vial. In: Walker G, editor. AB PI data sheet compendium and summaries of product characteristics 1998–99. London: Datapharm Publications Ltd, 1998: 1001
Fragmin 2500 IU and 5000 IU syringes. In: Walker G, editor. ABPI data sheet compendium and summaries of product characteristics 1998–99. London: Datapharm Publications Ltd, 1998: 1001–2
Prentice CR. Are symptomatic endpoints acceptable in thromboprophylactic studies? Haemostasis 1998; 28 Suppl. 3: 109–12
Kalodiki E, Nicolaides AN, Al Kutoubi A, et al. How “gold” is the standard? Interobservers’ variation on venograms. Int Angiol 1998 Jun; 17(2): 83–8
Collins MF. The optimum duration of low molecular weight heparin for thromboembolism prevention in high risk orthopedic surgery. Can J Hosp Pharm 1998 Dec; 51: 274–9
Gallus AS. Applying risk assessment models in orthopaedic surgery: overview of our clinical experience. Blood Coagul Fibrinolysis 1999; 10(6) Suppl. 2: S53–61
Levine M, Gent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med 1996; 334: 677–81
Koopman MMW, Prandoni P, Piovella F, et al. Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. N Engl J Med 1996; 334: 682–7
The Columbus Investigators. Low-molecular-weight heparin in the treatment of patients with venous thromboembolism. N Engl J Med 1997; 337: 657–62
Bergqvist D, Benoni G, Björgell O, et al. Low-molecular-weight heparin (enoxaparin) as prophylaxis against venous thromboembolism after total hip replacement. N Engl J Med 1996; 335: 696–700
Schulman S. Long-term prophylaxis in venous thromboembolism: LMWH or oral anticoagulation? Haemostasis 1998; 28 Suppl. 3: 17–21
Sanson B-J, Lensing AWA, Prins MH, et al. Safety of low-molecular-weight heparin in pregnancy: a systematic review. Thromb Haemost 1999; 81(5): 668–72
Ensom MHH, Stephenson MD. Low-molecular-weight heparins in pregnancy. Pharmacotherapy 1999; 19(9): 1013–25
Mishra B, Jackson G. Unstable angina: a review and practical guide to management. Int J Clin Pract 1999; 53(7): 530–4
Cairns JA, Théroux P, Lewis Jr HD, et al. Antithrombotic agents in coronary artery disease. Chest 1998; 114(5) Suppl.: 611S–33S
Sandercock P, Bamford J, Dennis M, et al. Atrial fibrillation and stroke: prevalence in different types of stroke and influence on early and long term prognosis (Oxfordshire community stroke project). BMJ 1992; 305: 1460–5
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: R.L. Bick, Department of Medicine and Pathology, University of Texas Southwestern Medical School, Dallas, Texas, USA; J. Fareed, Loyola University Medical Center, Maywood, Illinois, USA; E. Gurfinkel, Coronary Care Unit, Favaloro Foundation, Buenos Aires, Argentina; B.J. Hunt, The Rayne Institute, St Thomas’ Hospital, London, England; M.R. Lassen, Department of Orthopaedics, Hillerød Hospital, Hillerød, Denmark; P.J. Zed, Faculty of Pharmaceutical Sciences, University of British Columbia, Vancouver, British Columbia, Canada.
Data Selection
Sources: Medical literature published in any language since 1996 on dalteparin, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International, Auckland, New Zealand). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘dalteparin’ or ‘tedelparin’ or ‘dalteparin sodium’. EMBASE search terms were ‘dalteparin’ or ‘dalteparin sodium’ or ‘FR 860’ or ‘KABI 2165’ or ‘tedelparin’. AdisBase search terms were ‘dalteparin’ or ‘dalteparin sodium’ or ‘FR-860’ or ‘KABI 2165’ or ‘tedelparin’. Searches were last updated on 19th June 2000.
Selection: Studies in patients with or at risk of thromboembolic disease or on haemodialysis/haemofiltration who received dalteparin. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Dalteparin, thromboprophylaxis, orthopaedic surgery, general surgery, pregnancy, deep vein thrombosis, pulmonary embolism, outpatient treatment, unstable coronary artery disease, myocardial infarction, haemodialysis, haemofiltration, pharmacodynamics, pharmacokinetics, pharmacoeconomics, tolerability, dosage and administration, therapeutic use.
Rights and permissions
About this article
Cite this article
Dunn, C.J., Jarvis, B. Dalteparin. Drugs 60, 203–237 (2000). https://doi.org/10.2165/00003495-200060010-00010
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200060010-00010