Summary
Abstract
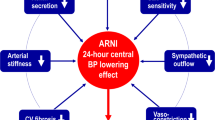
Irbesartan interrupts the renin-angiotensin system via selective blockade of the angiotensin II subtype 1 receptor; the latter being responsible for the pressor related effects of angiotensin II.
As treatment for mild to moderate hypertension, irbesartan 150 mg/day controlled diastolic BP in 56% of patients according to pooled data from several phase III studies and 77% of patients in a large phase IV study. In comparative trials, irbesartan was significantly more effective than losartan and valsartan as treatment for mild to moderate essential hypertension and as effective as enalapril or atenolol. Results from many studies show an additive antihypertensive effect when hydrochlorothiazide is added to irbesartan monotherapy. The drug also induces statistically significant regression of left ventricular mass in patients with hypertension and left ventricular hypertrophy, and preliminary evidence suggests it has beneficial haemodynamic effects in patients with heart failure.
Irbesartan is very well tolerated, exhibiting an adverse event profile similar to that seen with placebo in comparative trials.
In conclusion, although the role of irbesartan as a treatment for heart failure is little clearer than it was 2 years ago, the place of the drug in the management of hypertension is now better established. There is evidence to suggest the drug may have a role as initial therapy for hypertension, although formal recommendation in management guidelines will almost certainly not occur until long term morbidity and mortality benefits are established.
Pharmacodynamic Properties
Irbesartan is a selective angiotensin II subtype 1 (AT1) receptor antagonist, having no agonist activity and no affinity for the AT2 receptor. The drug has no affinity for α1- or α2-adrenoceptors or serotonergic receptors.
In the rabbit aorta model, increasing concentrations of irbesartan caused a parallel rightward shift of the angiotensin II concentration contractile response curve and a progressive reduction in maximal response. On this basis the receptor effects of irbesartan have been described as insurmountable.
In healthy volunteers, oral irbesartan (150mg), valsartan (80mg) or losartan (50mg) induced peak inhibition of the angiotensin II-induced pressor response after ∼4 hours; however, the effects of irbesartan were significantly greater, and lasted longer, than those of valsartan which were significantly greater than those of losartan.
Irbesartan has been shown to inhibit angiotensin II-induced proliferation of cultured human aorta smooth muscle cells in vitro and had anti-atherosclerotic effects in genetically hypercholesterolaemic rabbits in vivo. In animals subjected to experimental heart failure, myocardial infarction or aortic stenosis, administration of irbesartan decreased the development of ventricular hypertrophy. In patients with heart failure, single doses of irbesartan produced dose-dependent acute improvement in pulmonary capillary wedge pressure. Similar effects were seen in a further study that assessed both the acute and medium term (12-week) effects of the drug.
Several studies have shown that irbesartan improves glomerulosclerosis and reduces proteinuria in rats with experimentally induced renal failure.
In healthy volunteers, a 50mg dose of irbesartan increased renal vasodilation zbut did not affect arterial BP or glomerular filtration rate (GFR). The drug increased sodium excretion but did not exhibit a uricosuric effect. Irbesartan prevented arterial hypertension and renal vasoconstriction in response to exogenous angiotensin II infusion in this study. Similar effects were observed in a 6-week comparison with enalapril in patients with hypertension. Both drugs caused renal vasodilation without significantly affecting GFR; however, the effects of irbesartan occurred later in the dosage interval and were more prolonged than those of enalapril.
Pharmacokinetic Properties
Irbesartan has a bioavailability of ∼60 to 80% and this is not affected by concomitant food intake. In healthy volunteers, peak plasma irbesartan concentrations (Cmax) and area under the plasma concentration-time curve (AUC) increase linearly with increasing dosage although the time to peak plasma concentration (tmax) is dose-independent. The drug is 96% bound to plasma proteins and has a steady-state volume of distribution of 53 to 93L.
In patients with hypertension treated with irbesartan 300 mg once daily, steady-state irbesartan Cmax (3.9 mg/L) tmax (1.5 hours) and AUCτ (22.0 mg/L · h) values were very similar to those observed in healthy volunteers.
Single or multiple oral doses of irbesartan 300 mg/day produced apparent total and renal clearance values of ∼18 and 0.07 L/h. Elimination half-lives of 11 to 15 hours, independent of dosage, have been reported.
In healthy volunteers, 20 and ∼30% of radioactivity from a single 150mg dose of [14C] irbesartan was recovered from urine and faeces, respectively. After oral or intravenous administration of 14C-labelled irbesartan >80% of plasma radioactivity was attributable to unmetabolised irbesartan. The primary metabolic fate of the drug appears to be oxidation via cytochrome P450 (CYP) isoform 2C9.
Multiple oral doses of irbesartan ≤300 mg/day had no clinically relevant influence on the pharmacokinetic profiles of warfarin or nifedipine but a 150mg dose increased the AUCτ of fluconazole.
Therapeutic Use
Pooled data from 8 studies show that monotherapy with irbesartan ≥150 mg/day for 6 to 12 weeks induces a clinically significant reduction in BP. 56% of patientsresponded to an irbesartan dosage of 150 mg/day (response was defined as an endpoint DBP <90mm Hg or a reduction of ≥10mm Hg from baseline); antihy-pertensive effects increased with increasing dosage, reaching a plateau at ≥300 mg/day. Ambulatory monitoring has shown that irbesartan 150mg once daily controls 24-hour BP as effectively as 75mg twice daily. A phase IV study involving 7314 evaluable patients reported a 77% response rate to irbesartan 150 mg/day as monotherapy.
In randomised double-blind studies, irbesartan was significantly more effective than losartan or valsartan in patients with mild to moderate essential hypertension. Irbesartan was as effective as enalapril or atenolol in other well-designed studies.
Pooled results from 1- to 2-year extensions of studies evaluating the efficacy of irbesartan ≤300 mg/day ± hydrochlorothiazide initially in a total of 1006 patients with hypertension revealed a clinically relevant reduction from baseline in BP after 2 to 4 months treatment that plateaued after 6 to 8 months. BP normalised in 83% of patients and the overall response rate was 90% in this analysis.
A matrix study evaluating several combinations of irbesartan and hydrochlorothiazide showed that regimens containing higher dosages of irbesartan appeared to have greater antihypertensive efficacy than those containing higher dosages of hydrochlorothiazide.
In a further study, addition of hydrochlorothiazide to irbesartan monotherapy in patients not responsive to the latter resulted in additive antihypertensive effects within 2 weeks.
In the reverse situation, addition of irbesartan to hydrochlorothiazide was found to be significantly more effective than hydrochlorothiazide plus placebo.
Results from several preliminary studies show that irbesartan induces statistically significant regression of left ventricular mass (LVM) in patients with hypertension. Two randomised double-blind studies have compared the effects of irbesartan and atenolol on left ventricular hypertrophy in patients with hypertension. In both studies LVM-index decreased to a greater extent with irbesartan than with atenolol.
The antihypertensive efficacy of irbesartan ≤300 mg/day was not influenced by mild to severe renal impairment in a noncomparative study in patients with hypertension and renal impairment; however, the effects of the drug were enhanced in patients undergoing haemodialysis compared with those with mild to severe renal impairment.
A 12-week randomised double-blind study evaluating the effects of irbesartan 12.5 to 150 mg/day in patients with heart failure reported that significantly fewer patients receiving higher dosages (≥75 mg/day) of irbesartan discontinued treatment or were hospitalised because of worsening heart failure.
Tolerability
Analysis of pooled tolerability data from 9 studies (mean treatment duration 9 weeks) involving 2606 patients with mild to moderate hypertension revealed no clinically relevant difference between irbesartan and placebo in the incidence of any adverse event. The most common adverse event in these trials, headache, occurred significantly more frequently in placebo (17%) than in irbesartan-treated patients (12%). All other adverse events occurring at a rate ≥2% had a similar incidence in each group. 21% of irbesartan versus 20% of placebo recipients experienced ≥1 adverse event.
In a post-marketing surveillance study 1232 of 9009 patients (13.7%) reported a total of 1766 events of which 1257 were considered related to irbesartan. Most adverse events were mild to moderate in severity; the incidence of headache and dizziness, the most common adverse events, were 1.8 and 1.9%, respectively. 119 adverse events considered serious occurred in 85 patients; of these 20 were thought to be treatment related.
Dosage and Administration
Irbesartan is indicated for the treatment of hypertension in adults, either alone or in combination with other antihypertensive agents. The recommended starting dosage of irbesartan is 150mg administered once daily. In patients who are volume or salt depleted as a result of vigorous treatment with diuretics or haemodialysis, a lower starting dosage (75 mg/day) is recommended. The maximum recommended dosage of irbesartan is 300mg once daily. In patients who do not achieve an adequate BP response to monotherapy, the combination of irbesartan plus hydrochlorothiazide 12.5 mg/day may be used. Dosage adjustments are not required in elderly patients or in patients with renal or hepatic impairment.





Similar content being viewed by others
References
Birkenhäger WH, de-Leeuw PW. Non-peptide angiotensin type 1 receptor antagonists in the treatment of hypertension. J Hypertens 1999 Jul; 17: 873–81
Chung O, Csikós T, Unger T. Angiotensin II receptor pharmacology and AT1-receptor blockers. J Hum Hypertens 1999 Jan; 13 1: S11–20
Gillis JC, Markham A. Irbesartan.A review of its pharmacodynamic and pharmacokinetic properties and therapeutic use in the management of hypertension. Drugs 1997 Dec; 54: 885–902
Cazaubon C, Gougat J, Bousquet F, et al. Pharmacological characterization of SR 47436, a new nonpeptide AT1 subtype anti-otensin II receptor antagonist. J Pharmacol Exp Ther 1993 May; 265: 826–34
Moreau N, Richer C, Vincent MP, et al. Sympatho-inhibitory effects of SR 47436, a new angiotensin II antagonist in the pithed spontaneously hypertensive rat [abstract]. J Hypertens 1993 Nov; 11(11): 1309
Martineau D, Yamaguchi N, Briand R. Inhibition by BMS 186295, a selective nonpeptide AT1 antagonist, of adrenal catecholamine release induced by angiotensin II in the dog in vivo. Can J Physiol Pharmacol 1995; 73: 459–64
Fierens FLP, Vanderheyden PML, De Backer J–P, et al. Insurmountable angiotensin AT1 receptor antagonists: the role of tight antagonist binding. Eur J Pharmacol 1999 May 14; 372: 199–206
Vanderheyden PML, Fierens FLP, De Backer JP, et al. Distinction between surmountable and insurmountable selective AT1 receptor antagonists by use of CHO-K1 cells expressing human angiotensin II AT1 receptors. Br J Pharmacol 1999 Feb; 126: 1057–65
Vanderheyden PML, Fierens FLP, De Backer J–P, et al. Reversible and syntopic interaction between angiotensin receptor antagonists on Chinese hamster ovary cells expressing human angiotensin II type 1 receptors. Biochem Pharmacol 2000 Apr 15; 59(8): 927–35
Belz GG, Butzer R, Kober S, et al. Time course and extent of angiotensin II antagonism after irbesartan, losartan, and valsartan in humans assessed by angiotensin II dose response and radioligand receptor assay. Clin Pharmacol Ther 1999 Oct; 66: 367–73
Mazzolai L, Maillard M, Rossat J, et al. Angiotensin II receptor blockade in normotensive subjects: a direct comparison of three AT1 receptor antagonists. Hypertension 1999 Mar; 33: 850–5
Xi X-P, Graf K, Goetze S, et al. Central role of the MAPK pathway in ang II-mediated DNA synthesis and migration in rat vascular smooth muscle cells. Arterioscler Thromb Vasc Biol 1999 Jan; 19: 73–82
Herbert J–M, Delisée C, Dol F, et al. Effect of SR 47436, a novel angiotensin II AT1 receptor antagonist, on human vascular smooth muscle cells in vitro. Eur J Pharmacol 1994 Jan 14; 251: 143–50
Ambrose J, Pribnow DG, Giraud GD, et al. Angiotensin type 1 receptor antagonism with irbesartan inhibits ventricular hypertrophy and improves diastolic function in the remodeling post-myocardial infarction ventricle. J Cardiovasc Pharmacol 1999 Mar; 33: 433–9
Chobanian AV Comparison of the effects of ACE inhibition and AT1 receptor blockade on atherosclerosis [abstract]. Am J Hypertens 1998 Apr; 11(Pt 2): 238
Thrasher TN, Shifflett CP, Ramsay DJ. Blockade of angiotensin type 1 (AT1) receptors reduces ventricular hypertrophy in response to aortic stenosis in rats [abstract no. F002]. Am J Hypertens 1999 Apr; 12(4 Pt 2): 194A
Spinale FG, Holzgrefe HH, Walker JD, et al. Angiotensin II subtype-1 receptor blockade during the development of left ventricular hypertrophy in dogs: effects on ventricular and myocyte function. J Cardiovasc Pharmacol 1997 Nov; 30: 623–31
Richer C, Fornes P, Cazaubon C, et al. Effects of long-term angiotensin II AT1 receptor blockade on survival, hemodynamics and cardiac remodeling in chronic heart failure in rats. Cardiovasc Res 1999 Jan; 41: 100–8
LeJemtel T, Awan N, Liang C-s, et al. Irbesartan - a new angiotensin II antagonist: acute hemodynamic effects in patients with heart failure [abstract no. 3646]. Circulation 1996 Oct 15; 94 Suppl. 1: 622–3
Havranek EP, Thomas I, Smith WB, et al. Dose-related beneficial long-term hemodynamic and clinical efficacy of irbesartan in heart failure. J Am Coll Cardiol 1999 Apr; 33: 1174–81
Tan LG, Chang DS, Lukman LF, et al. Irbesartan decreases atrial natriuretic peptide levels and improves ejection fraction in diabetic patients with congestive heart failure [abstract]. Cardiovasc Drugs Ther 1999 Mar; 13: 13
McLaughlin K, Jardine AG. Angiotensin converting enzyme inhibitors and angiotensin receptor (AT1) antagonists: either or both for primary renal disease. Nephrol Dial Transplant 1999 Jan; 14: 25–8
Mackenzie HS, Provoost AP, Troy JL, et al. Irbesartan reduces blood pressure and prevents renal injury in fawn-hooded hypertensive rats [abstract no. B5]. Am J Hypertens 1996 Apr; 9(4 Pt 2): 127A
Anderson AE, Tolbert EM, Esparza AR, et al. Discordant effects of an angiotensin converting enzyme inhibitor (ACEI) vs an AII receptor antagonist (AA) on blood pressure and renal damage in spontaneously hypertensive rats [abstract]. Am J Hypertens 1996; 9(4 Pt 2): 14A
Ziai F, Ots M, Provoost AP, et al. The angiotensin receptor antagonist, irbesartan, reduces renal injury in experimental chronic renal failure. Kidney Int 1996; 50 Suppl. 57: S132–6
Burnier M, Hagman M, Nussberger J, et al. Short-term and sustained renal effects of angiotensin II receptor blockade in healthy subjects. Hypertension 1995 Apr; 25(Pt 1): 602–9
Schmitt F, Martinez F, Brillet G, et al. Acute renal effects of AT1-receptor blockade after exogenous angiotensin II infusion in healthy subjects. J Cardiovasc Pharmacol 1998 Feb; 31: 314–21
Pechère-Bertschi A, Nussberger J, Decosterd L, et al. Renal response to the angiotensin II receptor subtype 1 antagonist irbesartan versus enalapril in hypertensive patients. J Hypertens 1998 Mar; 16: 385–93
Fogari R, Poletti L, Zoppi A, et al. Effects of celipropol, irbesartan and lisinopril on insulin sensitivity in non diabetic hypertensive patients [abstract no. 36]. Cardiovasc Drugs Ther 1999 Mar; 13: 11
Polidori C, Ciccocioppo R, Nisato D, et al. Evaluation of the ability of irbesartan to cross the blood-brain barrier following acute intragastric treatment. Eur J Pharmacol 1998 Jul 3; 352: 15–21
Culman J, von-Heyer C, Piepenburg B, et al. Effects of systemic treatment with irbesartan and losartan on central responses to angiotensin II in conscious, normotensive rats. Eur J Pharmacol 1999 Feb 19; 367: 255–65
Lacour C, Canals F, Cazaubon C, et al. Central effects of irbesartan, an AT1 antagonist in rats [abstract]. Pharmacol Res 1995; 31 Suppl.: 326
Vachharajani NN, Shyu WC, Chando TJ, et al. Oral bioavailability and disposition characteristics of irbesartan, an angiotensin antagonist, in healthy volunteers. J Clin Pharmacol 1998 Aug; 38: 702–7
Vachharajani NN, Shyu WC, Mantha S, et al. Lack of effect of food on the oral bioavailability of irbesartan in healthy male volunteers. J Clin Pharmacol 1998 May; 38: 433–6
Marino MR, Langenbacher K, Ford NF, et al. Pharmacokinetics and pharmacodynamics of irbesartan in healthy subjects. J Clin Pharmacol 1998 Mar; 38: 246–55
Ruilope L. Human pharmacokinetic/pharmacodynamic profile of irbesartan: a new potent angiotensin II receptor antagonist. J Hypertens Suppl 1997 Dec; 15 Suppl. 7: S15–20
Vacharajani N, Shyu WC, Greene D, et al. The effect of age on the pharmacokinetics of irbesartan [abstract]. J Clin Pharmacol 1997; 37: 872
Marino MR, Langenbacher KM, Ford NF, et al. Pharmacodynamics and pharmacokinetics of irbesartan in patients with mild to moderate hypertension. J Cardiovasc Pharmacol and Therapeut 1999; 4(2): 67–75
Marino MR, Langenbacher KM, Raymond RH, et al. Pharmacokinetics and pharmacodynamics of irbesartan in patients with hepatic cirrhosis. J Clin Pharmacol 1998 Apr; 38: 347–56
Bristol Myers Squibb and Company. Avapro (irbesartan) prescribing information [on line]. [Accessed 28 April 2000]. Bristol Myers Squibb and Company. Princeton, New Jersey, USA. Revised Nov. 1999. Available at URL: http://www.bms.com/cgi-bin/bmscom/anypix.pl?pix=select%20PPI%20from%20TBPRODUCTPPI%20where%20PPIS EQ.54
Bourrié M, Meunier V, Berger Y, et al. Role of cytochrome P-4502C9 in irbesartan oxidation by human liver microsomes. Drug Metab Dispos 1999 Feb; 27: 288–96
Marino M, Vachharajani NN. The pharmacokinetics of irbesartan are not altered in special populations [abstract no. E023]. Am J Hypertens 1998 Apr; 11(4 Pt 2): 101A
Mangold B, Gielsdorf W, Marino MR. Irbesartan does not affect the steady-state pharmacodynamics and pharmacokinetics of warfarin. Eur J Clin Pharmacol 1999 Oct; 55: 593–8
Marino MR, Hammett JL, Ferreira I, et al. Effect of nifedipine on the steady-state pharmacokinetics and pharmacodynamics of irbesartan in healthy subjects. J Cardiovasc Pharmacol Therapeut 1998; 3(2): 111–8
Kovacs SJ, Wilton JH, Blum RA. Steady state (SS) pharmacokinetics (PK) of irbesartan alone and in combination with fluconazole (F) [abstract PI-59]. Clin Pharmacol Ther 1999 Feb; 65(2): 132
Marino MR, Langenbacher KM, Ford NF, et al. Effect of hydrochlorothiazide on the pharmacokinetics and pharmacodynamics of the angiotensin II blocker irbesartan. Clin Drug Invest 1997; 14(5): 383–91
Escolar M, López de Ocariz A, Simón M, et al. Effects of antacids on irbesartan pharmacokinetics [abstract no. FC-8]. Methods Find Exp Clin Pharmacol 1998; 20 Suppl. A: 53
Pool JL, Guthrie RM, Littlejohn TW III, et al. Dose-related antihypertensive effects of irbesartan in patients with mild-tomoderate hypertension. Am J Hypertens 1998 Apr; 11(4 Pt 1): 462–70
Guthrie R, Saini R, Herman T, et al. Efficacy and tolerability of irbesartan, an angiotensin II receptor antagonist, in primary hypertension. A double-blind, placebo-controlled, dose-titration study. Clin Drug Invest 1998; 15(3): 217–27
Fogari R, Ambrosoli S, Corradi L, et al. 24-Hour blood pressure control by once-daily administration of irbesartan assessed by ambulatory blood pressure monitoring. J Hypertens 1997; 15(12Pt 1): 1511–8
Kassler-Taub K, Littlejohn T, Elliott W, et al. Comparative efficacy of two angiotensin II receptor antagonists, irbesartan and losartan in mild-to-moderate hypertension [published erratum appears in Am J Hypertens 1998 Jun;11 (6 Pt 1):736]. Am J Hypertens 1998 Apr; 11(4): 445–53
Kochar M, Guthrie R, Triscari J, et al. Matrix study of irbesartan with hydrochlorothiazide in mild-to-moderate hypertension. Am J Hypertens 1999; 12(8 Pt 1): 797–805
Weber M, Saini R, Kassler-Taub K, et al. Irbesartan combined with low-dose hydrochlorothiazide for mild-to-moderate hypertension [abstract no. P16.27]. J Hypertens 1998 Jun; 16 Suppl. 2: S129
Reeves RA, Lin CS, Kassler-Taub K, et al. Dose-related efficacy of irbesartan for hypertension: an integrated analysis. Hypertension 1998 Jun; 31: 1311–6
Oparil S, Guthrie R, Lewin AJ, et al. An elective-titration study of the comparative effectiveness of two angiotensin II-receptor blockers, irbesartan and losartan. Irbesartan/Losartan Study Investigators. Clin Ther 1998 May–Jun; 20: 398–409
Mancia G, Korlipara K, van Rossum P, et al. Irbesartan results in superior blood pressure reduction vs valsartan [abstract]. Hypertension. In press
Larochelle P, Flack JM, Marbury TC, et al. Effects and tolerability of irbesarten versus enalapril in patients with severe hypertension. Am J Cardiol 1997 Dec 15; 80: 1613–4
Mimran A, Ruilope L, Kerwin L, et al. A randomised, double-blind comparison of the angiotensin II receptor antagonist, irbesartan, with the full dose range of enalapril for the treatment of mild-to-moderate hypertension. J Hum Hypertens 1998 Mar; 12: 203–8
Stumpe KO, Haworth D, Hoglund C, et al. Comparison of the angiotensin II receptor antagonist irbesartan with atenolol for treatment of hypertension. Blood Press 1998; 7: 31–7
Bunt T. Problems with interpreting the data in Kassler-Taub et al’s article comparing irbesartan and losartan [letter]. Am J Hypertens 1999 Jan; 12(1 Pt 1): 79–80
Bunt T. An elective-titration study of the comparative effectiveness of two angiotensin II-receptor blockers, irbesartan and losartan [letter]. Clin Ther 1999 Mar; 21: 611–2
Bays HE, Park JS, Reilly K, et al. Irbesartan safety and effectiveness: a postmarketing surveillance study [abstract]. Am J Hypertens 1999 Apr; 12(Pt 2): 120
Littlejohn T III, Saini R, Kassler-Taub K, et al. Long-term safety and antihypertensive efficacy of irbesartan: pooled results of five open-label studies. Clin Exp Hypertens 1999 Nov; 21: 1273–95
Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure. The sixth report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure. Arch Intern Med 1997 Nov 24; 157(21): 2413–46
Weir MR, Tolchin N, Toth P, et al. Addition of hydrochlorothiazide to irbesartan produces further dose-related reductions in blood pressure within two weeks [abstract no. P16.34]. J Hypertens 1998 Jun; 16 Suppl. 2: S130
Raskin P, Guthrie R, Flack JM, et al. The long-term antihypertensive activity and tolerability of irbesartan with hydrochlorothiazide. J Hum Hypertens 1999 Oct; 13: 683–7
Rosenstock J, Rossi L, Lin CS, et al. The effects of irbesartan added to hydrochlorothiazide for the treatment of hypertension in patients non-responsive to hydrochlorothiazide alone. J Clin Pharm Ther 1998 Dec; 23: 433–40
Howe P, Phillips P, Saini R, et al. The antihypertensive efficacy of the combination of irbesartan and hydrochlorothiazide assessed by 24-hour ambulatory blood pressure monitoring. Clin Exp Hypertens 1999 Nov; 21: 1373–96
Rizzo V, Villatico Campbell S, Di Maio F, et al. Cardiac damage and blood pressure variability reduction after antihypertensive drug therapy with irbesartan [abstract no. P.71]. J Hum Hypertens 1999 May; 13 Suppl. 3: S19
Villatico Campbell S, Rizzo V, Di Maio F, et al. Comparison of irbesartan versus enalapril on left ventricular mass and function in stage I–II hypertensives [abstract no. P.70]. J Hum Hypertens 1999 May; 13 Suppl. 3: S18
Kahan T, Malmqvist K, Edner M, et al. Rate and extent of left ventricular hypertrophy regression: a comparison of angiotensin II blockade with irbesartan and beta-blockade [abstract no. 857-4]. J Am Coll Cardiol 1998 Feb; 31 Suppl. 2A: 212A
Feraco E. Therapeutic effects of irbesartan in left ventricular hypertrophy [abstract no. D019]. Am J Hypertens 1999 Apr; 12(Pt 2): 115A
Cohen A, Bregman B, Agabiti-Rosei E, et al. Comparison of irbesartan vs felodipine in the regression after 1 year of left ventricular hypertrophy in hypertensive patients (the SILVER trial). J Hum Hypertens 1998 Jul; 12: 479–83
Cooper M, Anzalone D, Townes L, et al. Safety and efficacy of irbesartan in patients with hypertension and renal insufficiency [abstract no. E025]. Am J Hypertens 1998 Apr; 11(4 Pt 2): 102A
Pohl M, Cooper M, Ulrey J, et al. Safety and efficacy of irbesarten in hypertensive patients with type II diabetes and proteinuria [abstract no. D4]. Am J Hypertens 1997; 10(4 Pt 2): 105 A
Porush JG, Hunsicker LG, Clark WR, et al. Multi-center collaborative trial of angiotensin II receptor antagonism on renal function, morbidity and mortality in hypertensive type II diabetic patients with nephropathy [abstract no. P.22]. J Hum Hypertens 1999 May; 13 Suppl. 3: S6
Arner P, Parving H-H, Brocher-Mortenson J, et al. Irbesartan in patients with type 2 diabetes mellitus and microalbuminuria (IRMA II): methods and baseline characteristics. Princeton (NJ): Bristol Myers Squibb and Company. (Data on file)
Tonkon M, Awan N, Niazi I, et al. A study of the efficacy and safety of irbesartan in combination with conventional therapy, including ACE inhibitors, in heart failure. Int J Clin Pract 2000 Jan/Feb; 54(1): 11–8
Vijay N, Alhaddad IA, Denny DM, et al. Irbesartan compared with lisinopril in patients with mild to moderate heart failure [abstractno. 812-2]. J Am Coll Cardiol 1998 Feb; 31 (2Suppl. A): 68A
Simon TA, Gelarden RT, Freitag SA, et al. Safety of irbesartan in the treatment of mild to moderate systemic hypertension. Am J Cardiol 1998 Jul 15; 82: 179–82
British Medical Association, Royal Pharmaceutical Society of Great Britain. British National Formulary. No.39. London: The Pharmaceutical Press, 2000 Mar: 93–94
Bristol-Myers Squibb Company. Avalide (irbesartan-hydrochlorothiazide) prescribing information [on line]. [Accessed 28 Apr. 2000]. Bristol Myers Squibb and Company, Princeton New Jersey, USA. Revised Nov. 1999. Available at: URL: http://www.bms.com/cgi-bin/bmscom/anypix.pl?pix=select%20PPI%20from%20TBPRODUCTPPI%20where%20PPIS EQ.57
Zanchetti A, Chalmers J, Arakawa K, et al. 1993 Guidelines for the management of mild hypertension, memorandum from a World Health Organization/International Society of Hypertension meeting. J Hypertens 1993; 11: 905–18
Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke and coronary heart disease. Part 2, short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet 1990; 335: 827–38
Collins R, Peto R, Godwin J, et al. Blood pressure and coronary heart disease [letter]. Lancet 1990; 336: 370–1
Jackson R. What are the implications for the community of the discrepancy between the theory and practice of BP control? J Hum Hypertens 1995; 9 Suppl. 2: S25–8
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial. Lancet 1998 Jun 13; 351: 1755–62
Ramsay LE, Williams B, Johnston GD, et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens 1999 Sep; 13: 569–92
Guidelines Subcommittee. 1999 World Health Organization -International Society of Hypertension Guidelines for the Management of Hypertension. J Hypertens 1999 Feb; 17: 151–83
Gress TW, Nieto FJ, Shahar E, et al. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. N Engl J Med 2000 Mar 30; 342(13): 905–12
UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS39. BMJ 1998 Sep 12; 317: 713–20
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS38. BMJ 1998 Sep 12; 317: 703–13
Pylypchuk GB. ACE inhibitor-versus angiotensin II blocker-induced cough and angioedema. Ann Pharmacother 1998 Oct; 32: 1060–6
Cha YJ, Pearson VE. Angioedema due to losartan. Ann Pharmacother 1999; 33(9): 936–8
Mancia G, Stella ML, Grassi G. New drugs for the treatment of hypertension. Curr Opin Cardiol 1999; 14(5): 375–80
Korner PI, Jennings GL. Assessment of prevalence of left ventricular hypertrophy in hypertension. J Hypertens 1998; 16: 715–23
Kahan T. The importance of left ventricular hypertrophy in human hypertension. J Hypertens 1998 Sep; 16 Suppl. 7: S23–9
Levy D, Larson MG, Vasan RS, et al. The progression from hypertension to congestive heart failure. JAMA 1996 May 22/29; 275(20): 1557–62
Havranek ER The effects of the angiotensin II receptor antagonist irbesartan in patients with congestive heart failure. Cardiovasc Rev Rep 1998 Dec; 19: 29–33
McNeil JJ, Kram H. Cardiovascular disorders. In: Speight TM, Holford NHG, editors. Avery’s drag treatment. 4th ed. Auckland: Adis International Limited, 1997: 897–933
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: V. Bonarjee, Division of Cardiology, Department of Medicine, Central Hospital in Rogaland, Stavanger, Norway; M. Burnier, Policlinique Médicale Universitaire, Lausanne, Switzerland; S.G. Carruthers, Department of Medicine, Faculty of Medicine and Dentistry, The University of Western Ontario, London, Ontario, Canada; E. Havranek, Department of Medicine/Cardiology Division; Denver Health Medicine Center, Denver, Colorado, USA; L. Ruilope, Hypertension Unit, Hospital 12 de Octubre, Madrid, Spain; P. Vanderheyden, Department of Molecular Pharmacology, Free University of Brussels, Brussels, Belgium.
Data Selection
Sources: Medical literature published in any language since 1997 on Irbesartan, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International, Auckland, New Zealand). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘Irbesartan’ or ‘BMS 186295’ or ‘SR 47436’. EMBASE search terms were ‘Irbesartan’ or ‘BMS 186295’ or ‘SR 47436’. AdisBase search terms were ‘Irbesartan’ or ‘BMS-186295’ or ‘SR-47436’. Searches were last updated 1 May, 2000.
Selection: Studies in patients with hypertension or heart failure who received irbesartan. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Irbesartan, hypertension, heart failure, cardiovascular disease, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
Markham, A., Spencer, C.M. & Jarvis, B. Irbesartan. Drugs 59, 1187–1206 (2000). https://doi.org/10.2165/00003495-200059050-00014
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200059050-00014