Summary
Abstract
Prolonged-release mesalazine (Pentasa®2) consists of ethylcellulose-coated microgranules from which mesalazine (known in the US as mesalamine) is released in the small and large intestine in a diffusion-dependent manner.
Dose-dependent improvements in clinical and endoscopic parameters have been reported with prolonged-release mesalazine 2 and 4 g/day in clinical trials in patients with mild to moderately active ulcerative colitis. Induction of clinical and endoscopic remission was achieved in more patients receiving a daily dosage of 4 g/day than in those receiving placebo.
In patients with ulcerative colitis in remission, prolonged-release mesalazine is effective in reducing the rate of relapse. Higher dosages tend to be more effective, and a 12-month remission rate of 64% has been reported for patients treated with a 4g daily dosage of this formulation. Comparative data indicate that prolonged-release mesalazine has similar efficacy in maintaining remission to molar equivalent doses of sulfasalazine.
Data from a study in patients with mild to moderately active Crohn’s disease indicates that higher dosages (4 g/day) of prolonged-release mesalazine are more effective than placebo in reducing disease activity. After 16 weeks’ treatment, 64% of patients receiving a 4 g/day dosage experienced clinical improvement and 43% attained remission. In studies of patients in remission of Crohn’s disease, the formulation appears to be more effective in preventing relapse in patients with isolated small bowel disease than in those with colonie involvement.
The tolerability profile of oral prolonged-release mesalazine is similar to that of placebo and the incidence of adverse events does not appear to be dose-related. Nausea/vomiting, diarrhoea, abdominal pain and dyspepsia occur most frequently, although their incidence is low. Reports of nephrotoxicity during prolonged-release mesalazine treatment are rare.
Conclusions: Oral prolonged-release mesalazine is effective for maintenance and induction of remission of mild to moderately active colitis, both in patients with distal disease and in those with pancolitis. The formulation has similar efficacy to that of equimolar concentrations of sulfasalazine. Prolonged-release mesalazine also appears to be effective in the treatment of Crohn’s disease, and maintenance therapy is of particular value in patients with isolated small bowel involvement. Evidence suggests that higher dosages (3 to 4 g/day) of prolonged-release mesalazine have additional therapeutic benefits over lower dosages in patients with inflammatory bowel disease without increasing the incidence of adverse events.
Mode of Action
The mechanism by which mesalazine exerts its therapeutic actions remains elusive. However, numerous in vitro studies have indicated modulatory actions of mesalazine on the lipid mediators, cytokines and reactive oxygen species involved in the nonspecific inflammation and tissue damage characteristic of ulcerative colitis and Crohn’s disease.
In vitro studies have consistently demonstrated inhibitory effects of mesalazine on leukotriene (LT)B4 synthesis and release from biopsy specimens from individuals with normal colons and from patients with inflammatory bowel disease. Although mesalazine had conflicting effects on prostaglandin (PG)E2 levels, higher concentrations appeared to considerably reduce PGE2 production in colonic mucosa from patients with ulcerative colitis. Mesalazine also appears to reduce in vitro levels of LTC4, 5-hydroxyeicosatetraenoic acid (HETE), 11-, 12-, 15-HETE, PGD2 and platelet-activating factor.
In addition to inhibiting interferon (IFN)-γbinding, mesalazine reduced IFNγ-induced cell permeability and expression of the HLA-DR product of the major histocompatibility complex in colonic epithelial cell lines. Recent evidence suggests that mesalazine reverses the antiproliferative effects of tumour necrosis factor-(TNF)α and inhibits TNFα signalling events in intestinal cells. Mesalazine may also reduce interleukin (IL)-1/1β and IL-2 production.
Mesalazine reduced production of reactive oxygen species and protected against oxidant-induced tissue injury in several in vitro models.
Pharmacokinetic Properties
Entry of water into prolonged-release mesalazine microgranules creates a concentration gradient down which mesalazine diffuses, liberating active drug throughout the small bowel and colon.
Prolonged-release mesalazine acts topically in the affected bowel lumen. In volunteers, 18 to 20% of the administered dose was delivered to the jejunoileal segment as solubilised drug, while cumulative colonic delivery was 82% (approximately 75% as intact microgranules) during the first 7 hours after drug administration. Food intake, local pH and diarrhoeal states do not appear to substantially affect the disposition of mesalazine from the prolonged-release formulation.
Mesalazine is primarily metabolised by acetylation in the gut wall and liver, forming acetyl mesalazine. After oral administration, up to 53% of the administered dose is excreted in the urine as mesalazine plus acetyl mesalazine. Faecal excretion accounts for 40% of the administered dose (14 to 19% as unchanged mesalazine, although exact levels of acetylated and nonacetylated mesalazine in different colonie segments are not known).
Therapeutic Efficacy
Prolonged-release mesalazine at dosages up to 4 g/day has been investigated for the maintenance of remission and treatment of mild to moderately active ulcerative colitis and Crohn’s disease. Higher doses of prolonged-release mesalazine (3 to 4 g/day) were generally more effective than low doses (1.5 to 2 g/day) for treatment of acute exacerbations and for maintenance of disease remission.
At dosages of 2 or 4 g/day, the formulation improved clinical and endoscopic findings in patients with active ulcerative colitis, and success of treatment was independent of disease location. At a dosage of 1.5 g/day, the prolonged-release formulation was as effective as sulfasalazine 3 g/day in improving clinical and endoscopic parameters.
The estimated 1-year remission rate in patients with quiescent ulcerative colitis receiving prolonged-release mesalazine 1.5 g/day was similar to that with sulfasalazine 3 g/day (54 vs 46%). A 4g daily dosage of the mesalazine formulation was more effective than placebo in preventing endoscopie and clinical relapse (1-year remission rates 64 vs 38%).
Low dosages (≤2 g/day) of prolonged-release mesalazine had no significant benefits over placebo in patients with mild to moderately active Crohn’s disease. However, the formulation showed benefits compared with placebo at a dosage of 4 g/day in 1 study. In another study, prolonged-release mesalazine 4 g/day produced improvement, but was not statistically better than placebo. In addition to increasing the percentage of patients in remission, or experiencing therapeutic benefit, prolonged-release mesalazine reduced the time to remission and the percentage of treatment failures, compared with placebo. In another study, 16-week remission rates were significantly higher in patients receiving oral budesonide 9 mg/day than in those treated with a4g daily dosage of prolonged-release mesalazine (62 vs 36%).
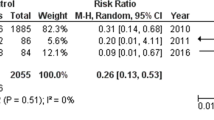
During prolonged-release mesalazine treatment for maintenance of remission of Crohn’s disease, dosages of ≤2 g/day were not consistently effective in producing benefits over placebo. However, significantly lower relapse rates were reported in patients treated with a 3g daily dosage than in those receiving placebo over a 48-week period. In a noncomparative study of up to 30 months’ duration, dosages of ≤4 g/day (median 3.7 g/day) were effective in maintaining 72% of patients continuously in remission over a 1-year period. Prolonged-release mesalazine showed particular benefit in reducing the rate of relapse in patients with isolated ileal disease. Endoscopie recurrence rates after 1 year in patients with a recent surgical resection of the affected bowel were significantly lower in those receiving prolonged-release mesalazine 3 g/day than in placebo recipients.
Improvements in disease status have been reported in children (aged 9 to 18 years) receiving prolonged-release mesalazine (22 to 53 mg/kg/day) for the treatment of active Crohn’s disease.
Tolerability
There is no evidence of a dose relationship in the adverse events profile of prolonged-release mesalazine and the tolerability profile is similar to that of placebo. The most common adverse events considered related to treatment with the mesalazine formulation at dosages up to 4 g/day were nausea and/or vomiting, headache, abdominal pain, diarrhoea and dyspepsia. Treatment-related adverse events necessitating study withdrawal occurred less commonly in patients receiving a 4g daily dosage of prolonged-release mesalazine than in those receiving placebo.
Although nephrotoxicity has been associated with the use of other mesalazine-containing preparations, impaired renal function does not appear to be associated with use of the prolonged-release formulation. However, as with other mesalazine preparations, precautionary monitoring of serum creatinine levels has been advocated.
Prolonged-release mesalazine appears to be well tolerated in patients intolerant of sulfasalazine. In patients who had experienced infertility as a result of sulfasalazine treatment, sperm quality was improved or normalised after switching to prolonged-release mesalazine treatment.
Dosage and Administration
Oral prolonged-release mesalazine at dosages up to 4 g/day is indicated for the induction of remission and treatment of mild to moderate ulcerative colitis in adults. For patients with quiescent disease, the recommended starting dosage is 1.5 g/day in 2 or 3 divided doses. However, evidence from clinical trials of dosages up to 4 g/day indicates a dose-dependent increase in efficacy.
No US or UK dosage recommendations are available for the use of prolonged-release mesalazine in the management of Crohn’s disease. However, individualised dosage of up to 4 g/day in divided doses is generally recommended for the treatment of active disease and maintenance of remission in other countries.
Prolonged-release mesalazine should not be used in patients with known sensitivity to salicylates or in those with severe renal and/or liver impairment, and is not recommended for use in children. The formulation should be used with caution during pregnancy.












Similar content being viewed by others
References
Martin F. Oral 5-aminosalicylic acid preparations in treatment of inflammatory bowel disease: an update. Dig Dis Sci 1987; 32 (12 Suppl.):57S–63S
Azad Khan AK, Piris J, Truelove SC. An experiment ot determine the active therapeutic moiety of sulphasalazine. Lancet 1979; II(8044): 892–5
Schröder H, Price E, Evans DA. Acetylator phenotype and adverse events of sulphasalazine in healthy subjects. Gut 1972; 13(4): 278–84
Haagen Nielsen O, Bondesen S. Kinetics of 5-aminosalicylic acid after jejunal instillation in man. Br J Clin Pharmacol 1983; 16(6): 738–40
Geier DL, Miner Jr PB. New therapeutic agents in the treatment of inflammatory bowel disease. Am J Med 1992; 93: 199–208
Hardy JG, Harvey WJ, Sparrow RA, et al. Localization of drug release sites from an oral sustained-release formulation of 5-ASA (Pentasa®) in the gastrointestinal tract using gamma scintigraphy. J Clin Pharmacol 1993; 33: 712–8
Järnerot G. New salicylates as maintenance treatment in ulcerative colitis. Gut 1994; 35: 1155–8
Hanauer SB. Inflammatory bowel disease. N Engl J Med 1996; 334: 841–8
Ireland A, Jewell DP. Mechanism of action of 5-aminosalicylic acid and its derivatives. Clin Sci 1990; 78: 119–25
Greenfield SM, Punchard NA, Teare JP, et al. Review article: the mode of action of the aminosalicylates in inflammatory bowel disease. Aliment Pharmacol Ther 1993; 7: 369–83
Travis SPL, Jewell DP. Salicylates for ulcerative colitis — their mode of action. Pharmacol Ther 1994; 63: 135–61
Schmidt C, Fels T, Baumeister B, et al. The effect of 5-aminosalicylate and para-aminosalicylate on the synthesis of prostaglandin E2 and leukotriene B4 in isolated colonic mucosal cells. Curr Med Res Opin 1996; 13(7): 417–25
Capasso F, Tavares IA, Bennett A. Release of platelet-activating factor (PAF) from human colon mucosa and its inhibition by 5-aminosalicylic acid. Drugs Exp Clin Res 1991; 17: 351–3
Rachmilewitz D, Karmeli F, Schwartz LW, et al. Effect of aminophenols (5-ASA and 4-ASA) on colonic interleukin-1 generation. Gut 1992; 33: 929–32
Di Paolo MC, Merrett MN, Crotty B, et al. 5-Aminosalicylic acid inhibits the impaired epithelial barrier function induced by gamma interferon. Gut 1996; 38: 115–9
Gionchetti P, Guarnieri C, Campieri M, et al. Scavenger effect of sulfasalazine, 5-aminosalicylic acid, and olsalazine on superoxide radical generation. Dig Dis Sci 1991; 36: 174–8
Sandoval M, Liu X, Mannick EE, et al. Peroxynitrite-induced apoptosis in human intestinal epithelial cells is attenuated by mesalamine. Gastroenterology 1997; 113: 1480–8
Horn H, Preclik G, Stange EF, et al. Modulation of arachidonic acid metabolism by olsalazine and other aminosalicylates in leukocytes. Scand J Gastroenterol 1991; 26: 867–79
Gertner DJ, Rampton DS, de Nucci G, et al. Eicosanoid release by rectal mucosa in vitro in ulcerative colitis: effects of conventional and potential new therapies. Eur J Gastroenterol Hepatol 1992; 4: 837–41
Eliakim R, Karmeli F, Chorev M, et al. Effect of drugs on colonic eicosanoid accumulation in active ulcerative colitis. Scand J Gastroenterol 1992; 27: 968–72
Fox C, Moore WC, Lichtenstein LM. Modulation of mediator release from human intestinal mast cells by sulfasalazine and 5-aminosalicylic acid. Dig Dis Sci 1991; 36: 179–84
Rachmilewitz D, Karmeli F, Eliakim R. Platelet-activating factor — a possible mediator in the pathogenesis of ulcerative colitis. Scand J Gastroenterol 1990; 25 Suppl. 172: 19–21
Bruin KF, Hommes DW, Jansen J, et al. Modulation of cytokine release from human monocytes by drugs used in the therapy of inflammatory bowel diseases. Eur J Gastroenterol Hepatol 1995; 7: 791–5
Mahida YR, Lamming CED, Gallagher A, et al. 5-Aminosalicylic acid is a potent inhibitor of interleukin 1 β production in organ culture of colonic biopsy specimens from patients with inflammatory bowel disease. Gut 1991; 32: 50–4
Stevens C, Lipman M, Fabry S, et al. 5-Aminosalicylic acid abrogates T-cell proliferation by blocking interleukin-2 production in peripheral blood mononuclear cells. J Pharmacol Exp Ther 1995; 272: 399–406
Mazlam MZ, Montazeri G, Hodgson HJF. The effects of some anti-inflammatory agents on cytokine release from human monocytes in vitro. Eur J Gastroenterol Hepatol 1993; 5: 515–20
Dallegri F, Ottonello L, Ballestrero A, et al. Cytoprotection against neutrophil derived hypochlorous acid: a potential mechanism for the therapeutic action of 5-aminosalicylic acid in ulcerative colitis. Gut 1990; 31: 184–6
Lobos EA, Sharon P, Stenson WF. Chemotactic activity in inflammatory bowel disease: role of leukotriene B4. Dig Dis Sci 1987; 32(12): 1380–8
Sharon P, Stenson WF. Enhanced synthesis of leukotriene B4 by colonic mucosa in inflammatory bowel disease. Gastroenterology 1984; 86(3): 453–60
Lauritsen K, Laursen LS, Bukhave K, et al. Effects of topical 5-aminosalicylic acid and prednisolone on prostaglandin E2 and leukotriene B4 levels determined by equilibrium in vivo dialysis of rectum in relapsing ulcerative colitis. Gastroenterology 1986; 91(4): 837–44
Guimbaud R, Izzo A, Martinolle JP, et al. Intraluminal excretion of PAF, lysoPAF, and acetylhydrolase in patients with ulcerative colitis. Dig Dis Sci 1995; 40(12): 2635–40
Eliakim R, Kanneli F, Razin E, et al. Role of platelet-activating factor in ulcerative colitis. Enhanced production during active disease and inhibition by sulphasalazine and prednisolone. Gastroenterology 1988; 95(5): 1167–72
Thyssen E, Turk J, Bohrer A, et al. Quantification of distinct molecular species of platelet-activating factor in ulcerative colitis. Lipids 1996; 31 Suppl.: S255–9
Sobhani I, Hochlaf S, Denziot Y, et al. Raised concentrations of platelet activating factor in colonic mucosa of Crohn’s disease patients. Gut 1992; 33(9): 1220–5
Crotty B, Hoang P, Dalton HR, et al. Salicylates used in inflammatory bowel disease and colchicine impair interferon-γ induced HLA-DR expression. Gut 1992; 33: 59–64
Crotty B, Rosenberg WMC, Aronson JK, et al. Inhibition of binding of interferon-γ to its receptor by salicylates used in inflammatory bowel disease. Gut 1992; 33: 1353–7
Horie Y, Chiba M, Suzuki T, et al. Induction of major histocompatibility complex class II antigens on human colonic epithelium by interferon-gamma, tumor necrosis factor-alpha, and interleukin-2. J Gastroenterol 1998; 33(1): 39–47
Selby WS, Janossy G, Mason DY, et al. Expression of HLA-DR antigens by colonic epithelium in inflammatory bowel disease. Clin Exp Immunol 1983; 53(3): 614–8
McDonald GB, Jewell DP. Class II antigen (HLA-DR) expression by intestinal epithelial cells in inflammatory diseases of colon. J Clin Pathol 1987; 40: 312–7
Ishii N, Chiba M, Iiziuka M, et al. Induction of HLA-DR antigen expression on human colonic epithelium by tumor necrosis factor-α and interferon-γ. Scand J Gastroenterol 1994; 29(10): 903–7
Oberhuber G, Püspök A, Peck-Radosavlevic M, et al. Aberrant esophageal HLA-DR expression in a high percentage of patients with Crohn’s disease. Am J Surg Pathol 1999; 23(8): 970–6
Kaiser GC, Yan F, Polk DB. Mesalamine blocks tumor necrosis factor growth inhibition and nuclear factor κ-B activation in mouse colonocytes. Gastroenterology 1999; 116: 602–9
Greenfield SM, Hamblin AS, Shakoor ZS, et al. Inhibition of leucocyte adhesion molecule upregulation by tumour necrosis factor a: a novel mechanism of action of sulphasalazine. Gut 1993; 34: 252–6
Simmonds AJ, Allen RE, Stevens TRJ, et al. Chemiluminescence assay of mucosal reactive oxygen metabolites in inflammatory bowel disease. Gastroenterology 1992; 103(1): 186–96
Keshavarzian A, Sedghi S, Kanofsky J, et al. Excessive production of reactive oxygen metabolites by inflamed colon: analysis by chemiluminescence probe. Gastroenterology 1002; 103(1): 177–85
Prónai L, Yukinobu I, Lang I, et al. The oxygen-centered radicals scavenging activity of sulphasalazine and its metabolites. A direct protection of the bowel. Acta Physiol Hung 1992; 80: 317–23
Greenfield SM, Punchard NA, Thompson RPH. Inhibition of red cell membrane lipid peroxidation by sulphasalazine and 5-aminosalicylic acid. Gut 1991; 32: 1156–9
Simmonds NJ, Millar AD, Blake DR, et al. Antioxidant effects of aminosalicylates and potential new drugs for inflammatory bowel disease: assessment in cell-free systems and inflamed human colorectal biopsies. Aliment Pharmacol Ther 1999; 13: 363–72
Yu DK, Morrill B, Eichmeier LS, et al. Pharmacokinetics of 5-aminosalicylic acid from controlled-release capsules in man. Eur J Clin Pharmacol 1995; 48: 273–7
Wilding IR, Kenyon CJ, Hooper G. Gastrointestinal spread of oral prolonged-release mesalazine microgranules (Pentasa) dosed as either tablets or sachet. Aliment Pharmacol Ther 2000; 14: 163–9
Small RE, Schraa CC. Chemistry, pharmacology, pharmacokinetics, and clinical applications of mesalamine for the treatment of inflammatory bowel disease. Pharmacotherapy 1994; 14: 385–98
Rasmussen SN, Bondesen S, Hvidberg EF, et al. 5-Aminosalicylic acid in a slow-release prepararation: bioavailability, plasma level, and excretion in humans. Gastroenterology 1982; 83: 1062–70
Stolk LM, Rietbroek R, Wiltink EH, et al. Dissolution profiles of mesalazine formulations in vitro. Pharm Weekbl Sci 1990; 12: 200–4
Larouche J, Morais J, Picard M, et al. Release of 5-ASA from Pentasa in patients with Crohn’s disease of the small intestine. Aliment Pharmacol Ther 1995; 9: 315–20
Wilding IR. A scintigraphic study to evaluate what happens to Pentasa® and Asacol® in the human gut. Pract Gastroenterol 1999: 1–8
Layer PH, Goebell H, Keller J, et al. Delivery and fate of oral mesalamine microgranules within the human small intestine. Gastroenterology 1995; 108: 1427–33
Christensen LA, Fallingborg J, Abildgaard K, et al. Topical and systemic availability of 5-amino-salicylate: comparisons of three controlled release preparations in man. Aliment Pharmacol Ther 1990; 4: 523–33
Christensen LA, Fallingborg J, Jacobsen B A, et al. Comparative bioavailability of 5-aminosalicylic acid from a controlled release preparation and an azo-bond preparation. Aliment Pharmacol Ther 1994; 8: 289–94
Christensen LA, Slot O, Sanchez G, et al. Release of 5-aminosalicylic acid from Pentasa during normal and accelerated intestinal transit time. Br J Clin Pharmacol 1987; 23: 365–9
Rijk MCM, Van Schaik A, Van Tongeren JHM. Disposition of mesalazine from mesalazine-delivering drugs in patients with inflammatory bowel disease, with and without diarrhoea. Scand J Gastroenterol 1992; 27: 863–8
Bondesen S, Tage-Jensen U, Jacobsen O, et al. 5-Aminosalicylic acid in patients with an ileo-rectal anastomosis. A comparison of the fate of sulfasalazine and Pentasa. Eur J Clin Pharmacol 1986; 31: 23–6
Bondesen S, Hegnhoj J, Larsen F, et al. Pharmacokinetics of 5-aminosalicylic acid in man following administration of intravenous bolus and Per Os slow-release formulation. Dig Dis Sci 1991; 36: 1735–40
Daneshmend TK, Hendrickse M, Salzmann M, et al. Does systemic absorption of 5-aminosalicylic acid from olsalazine (Dipentum®) and mesalazine (Asacol® and Pentasa®) differ significantly in ulcerative colitis? [abstract]. Gut 1994; 35 Suppl. 4: 233
Staerk-Laursen L, Stokholm M, Bukhave K, et al. Disposition of 5-aminosalicylic acid by olsalazine and three mesalazine preparations in patients with ulcerative colitis: comparison of intraluminal colonic concentrations, serum values, and urinary excretion. Gut 1990; 31: 1271–6
Christensen LA, Rasmussen SN, Hansen SH. Disposition of 5-aminosalicylic acid and N-acetyl-5-aminosalicylic acid in fetal and maternal body fluids during treatment with different 5-aminosalicylic acid preparations. Acta Obstet Gynecol Scand 1994; 74: 399–402
Lauritsen K, Laursen LS, Rask-Madsen J. Clinical pharmaco-kinetics of drugs used in the treatment of gastrointestinal diseases (Part II). Clin Pharmacokinet 1990; 19: 94–125
Botoman VA, Bonner GF, Botoman DA. Management of inflammatory bowel disease. Am Fam Physician 1998; 57: 57–68
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults. Am J Gastroenterol 1997; 92: 204–11
Ardizzone S, Molteni P, Bollani S, et al. Guidelines for the treatment of ulcerative colitis in remission. Eur J Gastroenterol Hepatol 1997; 9: 836–41
Hanauer S, Schwartz J, Robinson M, et al. Mesalamine capsules for the treatment of active ulcerative colitis: results of a controlled trial. Am J Gastroenterol 1993; 88: 1188–97
Munakata A, Yoshida Y, Muto T, et al. Double-blind comparative study of sulfasalazine and controlled-release mesalazine tablets in the treatment of active ulcerative colitis. J Gastroenterol 1995; 30 Suppl. 8: 108–11
Farup PG, Oddsson E, Hinterleitner T. Mesalamine 4 g prolonged release granules b.i.d. and q.i.d. versus tablets q.i.d. for mild/moderate ulcerative colitis [abstract]. Gastroenterology 1999; 116(2): A713
Fockens P, Mulder CJJ, Tytgat GNJ, et al. Comparison of the efficacy and safety of 1.5 compared with 3.0 g oral slow-release mesalazine (Pentasa) in the maintenance treatment of ulcerative colitis. Eur J Gastroenterol Hepatol 1995; 7: 1025–30
Mulder CJ, Tytgat GNJ, Weterman IT, et al. Double-blind comparison of slow-release 5-aminosalicylate and sulfasalazine in remission maintenance in ulcerative colitis [see comments]. Gastroenterology 1988; 95: 1449–53
Miner P, Hanauer S, Robinson M, et al. Safety and efficacy of controlled-release mesalamine for maintenance of remission in ulcerative colitis. Dig Dis Sci 1995; 40: 296–304
Hanauer SB, Meyers S. Management of Crohn’s disease in adults. Am J Gastroenterol 1997; 92(4): 559–66
Singleton J. Second trial of mesalamine therapy in the treatment of active Crohn’s disease [letter]. Gastroenterology 1994; 107: 632–3
Singleton JW, Hanauer SB, Gitnick GL, et al. Mesalamine capsules for the treatment of active Crohn’s disease: results of a 16-week trial. Pentasa Crohn’s Disease Study Group [see comments]. Gastroenterology 1993; 104: 1293–301
Hanauer SB, Krawitt EL, Robinson M, et al. Long-term management of Crohn’s disease with mesalamine capsules (Pentasa®). Am J Gastroenterol 1993; 88: 1343–51
Colombel J-F, Lémann M, Cassagnou M, et al. Acontrolled trial comparing ciprofloxacin with mesalazine for the treatment of active Crohn’s disease. Groupe d’Etudes Thérapeutiques des Affections Inflammatoires Digestives (GETAID). Am J Gastroenterol 1999; 94: 674–8
Thomsen OØ, Cortot A, Jewell D, et al. A comparison of budesonide and mesalamine for active Crohn’s disease. N Engl J Med 1998; 339: 370–4
Rasmussen SN, Lauritsen K, Tage-Jensen U, et al. 5-Aminosalicylic acid in the treatment of Crohn’s disease. A 16-week double-blind, placebo-controlled, multicentre study with Pentasa. Scand J Gastroenterol 1987; 22: 877–83
Mahida YR, Jewell DP. Slow-release 5-amino-salicylic acid (Pentasa) for the treatment of active Crohn’s disease. Digestion 1990; 45: 88–92
Gendre J-P, Mary J-Y, Florent C, et al. Oral mesalamine (Pentasa) as maintenance treatment in Crohns disease: a multicenter placebo-controlled study [in French]. Ann Gastroenterol Hepatol 1993; 29: 251–6
Brignola C, Iannone P, Pasquali S, et al. Placebo-controlled trial of oral 5-ASA in relapse prevention of Crohn’s disease. Dig Dis Sci 1992; 37: 29–32
Sutherland LR, Martin F, Bailey RJ, et al. 5-Aminosalicylic acid (Pentasa) in the maintenance of remission of Crohn’s disease [abstract]. Gastroenterology 1995; 108 Suppl.: 924
Brignola C, Cottone M, Pera A, et al. Mesalamine in the prevention of endoscopie recurrence after intestinal resection for Crohn’s disease. Italian Cooperative Study Group. Gastroenterology 1995; 108: 345–9
Lochs H, Mayer M, Fleig WE, et al. Prophylaxis of postoperative relapse in Crohn’s disease with mesalamine: European Cooperative Crohn’s Disease Study VI. Gastroenterology 2000; 118: 264–73
Bondesen S, Danish 5-ASA-group. Mesalazine (Pentasa) as prophylaxis in Crohn’s disease. A multicenter, controlled trial [abstract]. Scand J Gastroenterol 1991; 26 Suppl. 183: 68
Modigliani R, Colombel J-F, Dupas J-L, et al. Mesalamine in Crohn’s disease with steroid-induced remission: effect on steroid withdrawal and remission maintenance, Groupe d’Etudes Therapeutiques des Affections Inflammatoires Digestives. Gastroenterology 1996; 110: 688–93
Griffiths A, Koletzko S, Sylvester F, et al. Slow-release 5-aminosalicylic acid therapy in children with small intestinal Crohn’s disease. J Pediatr Gastroenterol Nutr 1993; 17: 186–92
Robinson M, Hanauer S, Hoop R, et al. Mesalamine capsules enhance the quality of life for patients with ulcerative colitis. Aliment Pharmacol Ther 1994; 8: 27–34
Singleton JW, Hanauer S, Robinson M. Quality-of-life results of double-blind, placebo-controlled trial of mesalamine in patients with Crohn’s disease. Dig Dis Sci 1995; 40: 931–5
Zbrozek A, Hoop R, Robinson M, et al. Test of an instrument to measure function-related quality of life in patients with ulcerative colitis. Pharmacoeconomics 1993; 4(1): 31–9
Kotanagi H, Ito M, Koyama K, et al. Pancytopenia associated with 5-aminosalicylic acid use in a patient with Crohn’s disease. J Gastroenterol 1998; 33: 571–4
Netzer P. Diffuse alopecia as side effect of mesalazine therapy in Crohn’s disease [in German]. Schweiz Med Wochenschr 1995; 125: 2438–42
Declerck D, Wallaert B, Demarcq-Delerue G, et al. Diffuse interstitial pneumonia linked to 5-aminosalicylate [in French]. Rev Mal Respir 1994; 11: 292–3
Janowski M, Laglenne S, Beaufils F. Hypersensitivity pneumopathy during treatment with mesalazine (Pentasa®). The value of bronchoalveolar lavage [in French]. Rev Med Interne 1992; 13: 545
Besseau M, Delchier JC, Blazquez M, et al. Acute pancreatitis induced by mesalazine (Pentasa) [in French]. Gastroenterol Clin Biol 1991; 15(2): 174–5
Gron I, Winther A. Exanthema in two patients with ulcerative colitis treated with Pentasa [in Danish]. Ugeskr Laeger 1988; 150: 32
Kapur KC, Williams GT, Allison MC. Mesalazine induced exacerbation of ulcerative colitis. Gut 1995; 37: 838–9
Marteau P, Nelet F, Lu LM, et al. Adverse events in patients treated with 5-aminosalicylic acid: 1993–1994 pharmaco-vigilance report for Pentasa in France. Aliment Pharmacol Ther 1996; 10: 949–56
Marteau P, Tennenbaum R, Elefant E, et al. Foetal outcome in women with inflammatory bowel disease treated during pregnancy with oral mesalazine microgranules. Aliment Pharmacol Ther 1998; 12: 1101–8
Tennenbaum R, Marteau P, Elefant E, et al. Pregnancy outcome in inflammatory bowel disease [in French]. Gastroenterol Clin Biol 1998; 23(5): 464–9
Pardi DS, Tremaine WJ, Sandborn WJ, et al. Renal and urologic complications of inflammatory bowel disease. Am J Gastroenterol 1998; 93: 504–14
Corrigan G, Stevens PE. Interstitial nephritis associated with the use of mesalazine in inflammatory bowel disease. Aliment Pharmacol Ther 2000; 14(1): 1–6
World MJ, Stevens PE, Ashton MA, et al. Mesalazine-associated interstitial nephritis. Nephrol Dial Transplant 1996; 11: 614–21
Howard G, Lynn KL. Renal dysfunction and the treatment of inflammatory bowel disease (IBD): a case for monitoring. Aust N Z J Med 1998; 28: 346
Brouillard M, Gheerbrant JD, Gheysens Y, et al. Interstitial nephritis and mesalazine: three new cases [in French]. Gastroenterol Clin Biol 1998; 22: 724–6
Be Broe ME, Stolear JC, Nouwen EJ, et al. 5-aminosalicylic acid (5-ASA) and chronic tubulointerstitial nephritis in patients with chronic inflammatory bowel disease: is there a link? Nephrol Dial Transplant 1997; 12: 1839–41
Colombel J-F, Brabant G, Gubler M-C, et al. Renal insufficiency in infant: side-effect of prenatal exposure to mesalazine? [letter]. Lancet 1994; 344: 620–1
Mulder CJ, Tytgat GN, Dekker W, et al. Pentasa in lieu of sulfasalazine [letter]. Ann Intern Med 1988; 108: 911–2
Birnie GG, McLeod TI, Watkinson G. Incidence of sulphasalazine-induced male infertility. Gut 1981; 22(6): 452–5
Steeno OP. Side-effects of salazopyrin on male fertility. Eur J Obstet Gynecol Reprod Biol 1984; 18(5–6): 361–4
Kjaergaard N, Christensen LA, Lauritsen JG, et al. Effects of mesalazine substitution on salicylazosulfapyridine-induced seminal abnormalities in men with ulcerative colitis. Scand J Gastroenterol 1989; 24(7): 891–6
Zelissen PM, van-Hattum J, Poen H, et al. Influence of salazosulphapyridine and 5-aminosalicylic acid on seminal qualities and male sex hormones. Scand J Gastroenterol 1988; 23: 1100–4
Roberts Pharmaceuticals. Pentasa prescribing information. Eatontown, New Jersey, USA, 1998
Pentasa data sheet. Ferring Pharmaceuticals. In: ABPI Compendium of Data Sheets and Summaries of Product Characteristics. London: DataPharm Publications Ltd, 1999: 437–8
Russel MGVM, Stockbrügger RW. Epidemiology of inflammatory bowel disease: an update. Scand J Gastroenterol 1996; 31: 417–27
Harting JW. New developments in the pharmacotherapy of inflammatory bowel disease. Pharm Weekbl Sci 1992; 14: 275–86
Glickman RM. Inflammatory bowel disease: ulcerative colitis and Crohn’s disease. In: Fauci AS, Braunwald E, Isselbacher KJ, et al., editors. Harrison’s principles of internal medicine. 14th ed. v. 2. New York: McGraw-Hill, 1998: 1633–45
Ardizzone S, Bianchi PG. A practical guide to the management of distal ulcerative colitis. Drugs 1998; 55: 519–42
Brynskov J, Rasmussen SN. Clinical pharmacology in gastroenterology: development of new forms of treatment of inflammatory bowel disease. Scand J Gastroenterol Suppl 1996; 216: 175–80
Peppercorn MA. Sulfasalazine: pharmacology, clinical use, toxicity, and related new drug development. Ann Intern Med 1984; 101(3): 377–86
Singleton JW, Law DH, Kelley Jr ML, et al. National Cooperative Crohn’s Disease Study: adverse reactions to study drugs. Gastroenterology 1979; 44 (4 Pt 2): 870–82
Camilla C, Giunta M, Rosselli M, et al. Mesalamine in the maintenance treatment of Crohn’s disease: a meta-analysis adjusted for confounding variables. Gastroenterology 1997; 113: 1465–73
Rutgeerts P, Geboes K, Vantrappen G, et al. Predictability of the postoperative course of Crohn’s disease. Gastroenterology 1990; 99(4): 956–63
Olaison G, Smedh K, Sjödahl R. Natural course of Crohn’s disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut 1992; 33(3): 1150–1
Author information
Authors and Affiliations
Corresponding author
Additional information
Also known as mesalamine in the US
Various sections of the manuscript reviewed by: V.A. Botoman, Department of Gastroenterology, Cleveland Clinic, Fort Lauderdale, Florida, USA; P.D. Layer, Department of Internal Medicine, Israelitic Hospital, Hamburg, Germany; Y.R. Mahida, Division of Gastroenterology, University Hospital, Nottingham, UK; N.A. Punchard, Department of Biology and Health Science, University of Luton, Luton, UK; S.N. Rasmussen, Department of Medical Gastroenterology, Hvidovre University Hospital, Copenhagen, Denmark; M. Robinson, University of Oklahoma College of Medicine, Oklahoma City, Oklahoma, USA; B.N. Singh, Department of Industrial Pharmacy, St John’s University, New York, New York, USA; J.W. Singleton, Division of Gastroenterology & Hepatology, University of Colorado Health Sciences Center, Denver, Colorado, USA.
Data Selection
Sources: Medical literature published in any language since 1983 on Mesalazine, identified using AdisBase (a proprietary database of Adis International, Auckland, New Zealand) and Medline. Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: AdisBase search terms were ‘Mesalazine’ or ‘Mesalamine’ or ‘5-ASA’ and (‘Inflammatory-bowel-disorders’ or ‘Proctitis’) and (‘slow-release’ or ‘prolonged-release’). Medline search terms were ‘Mesalazine’ or ‘Mesalamine’ or ‘5-ASA’ and (‘Inflammatory-boweldiseases’ or ‘Crohn-disease’ or ‘Ulcerative-colitis’ or ‘Proctitis’) and ‘slow-release’. Searches were last updated 20 Mar 2000.
Selection: Studies in patients with ulcerative colitis or Crohn’s disease who received oral prolonged-releasemesalazine (Pentasa®). Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Mesalazine, mesalamine, Pentasa®, ulcerative colitis, Crohn’s disease, pharmacodynamics, pharmacokinetics, therapeutic
Rights and permissions
About this article
Cite this article
Clemett, D., Markham, A. Prolonged-Release Mesalazine. Drugs 59, 929–956 (2000). https://doi.org/10.2165/00003495-200059040-00016
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200059040-00016