Summary
Primary Raynaud’s phenomenon is common, particularly in younger women, and may be familial. Vasospasm is not confined to the digits and may involve, for example, the tongue and nose, and also visceral organs like the heart, oesophagus or lung and cerebral circulation. Symptoms tend to be milder in primary compared with secondary Raynaud’s phenomenon, which is associated with other disorders such as the connective tissue diseases. Indeed, the severity of symptoms often acts as the predictor for the much later onset of the associated systemic disease. Occupational Raynaud’s phenomenon is related to the use of vibrating instruments, and a significant proportion of patients may be cured by an early change in job. In those over 60 years of age, Raynaud’s phenomenon is commonly a result of atherosclerotic obstructive arterial disease, and screening for and treatment of the risk factors is appropriate.
The best-studied mechanisms in Raynaud’s phenomenon involve the blood and vascular endothelium. Microcirculatory flow may be impeded by activated platelet clumps, rigid red and white blood cells and damaged endothelium. These platelet clumps, white blood cells and damaged endothelium also release vasoactive/vasoconstrictive compounds which may additionally trigger the clotting cascade and thrombosis.
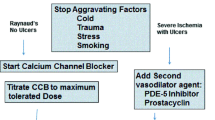
Initial management for mild disease should focus on support and advice regarding avoidance of known precipitating factors, including vasospastic drugs. Cold protection with warming agents, ‘Abel’ shoes and also electrically heated gloves and socks is effective, but may be too cumbersome and inconvenient for some patients. Simple vasodilators like naftidrofuryl, inositol nicotinate and possibly pentoxifylline (oxpentifylline) are useful in mild disease, with adverse effects like headache and flushing being less problematic. The ‘gold standard’ of Raynaud’s phenomenon treatment is nifedipine, a calcium channel antagonist/blocker. Full dosage, however, can be limited by ankle swelling, headache and flushing, but adverse effects may be reduced by using the ‘retard’ or long-acting preparations. Adverse effects are also reduced with the newer calcium channel antagonists like diltiazem but at the expense of efficacy. Useful, enhanced benefit is also achieved by combination therapy with vasodilators.
Newer treatments include the prostaglandin analogues which are effective but disadvantaged by their parenteral route of administration, and lack of licence in some countries. Oral preparations are, however, being studied and are in the pipeline. Essential fatty acid supplementation is mildly effective, while ketanserin and calcitonin gene—related peptide both look promising. Lumbar sympathectomy retains its important role in the treatment of Raynaud’s phenomenon involving the lower limbs.
Satisfactory symptomatic relief is now possible for many patients with Raynaud’s phenomenon and this should certainly be the aim for all patients seeking medical help.
Similar content being viewed by others
References
Porter JM, Bardona EJ, Baur GM, et al. The clinical significance of Raynaud’s syndrome. Surgery 1976; 80: 756–64
Maricq HR, Weinrich MC, Keil JE, et al. Prevalence of Raynaud’s phenomenon in the general population. J Chronic Dis 1986; 39: 423–7
Olsen N, Neilsen SL. Prevalence of primary Raynaud’s phenomena in young females. Scand J Clin Lab Invest 1978; 37: 761–4
Edwards JM, Porter JM. Associated disease in patients with Raynaud’s syndrome. Vasc Med Rev 1990; 1: 51–8
Goodfield MJD, Hume A, Rowell. NR. The acute effects of cigarette smoking on cutaneous blood flow in smoking and non-smoking subjects with and without Raynaud’s phenomenon. Br J Rheumatol 1990; 29: 89–91
de Trafford JC, Lafferty K, Potter CE, et al. An epidemiological survey of Raynaud’s phenomenon. Eur J Vasc Surg 1988; 2(3): 167–70
Belch JJF, Land D, Park RHR, et al. Decreased oesophageal blood flow in patients with Raynaud’s phenomenon. Br J Rheumatol 1988; 27: 426–30
Porter JM, Rivers SP, Anderson CJ, et al. Evaluation and management of patients with Raynaud’s syndrome. Am J Surg 1987; 142: 183–9
Allen EV, Brown GE. Raynaud’s disease: a critical review of minimal requisites for diagnosis. Am J Med Sci 1932; 183: 187–200
Kallenberg CGM, Wouda AA, Hoet MA, et al. Development of connective tissue disease in patients presenting with Raynaud’s phenomenon: a six year follow up with emphasis on the predictive value of antinuclear antibodies as detected by immunoblotting. Ann Rheum Dis 1988; 47: 634–41
Kallenberg CG, Wouda AA, Hoet MH. Systemic involvement and immunological findings in patients presenting with Raynaud’s phenomenon. Am J Med 1980; 69: 675–80
Maricq HR, Johnson MN, Whetstone CC. Capillary abnormalities in polyvinyl chloride production workers in examinations by in vivo microscopy. JAMA 1976; 236: 1368–71
Taylor W. The hand-arm vibration syndrome: secondary Raynaud’s phenomenon of occupational origin. Proc R Coll Phys Edinb 1989; 19: 7–14
Lewis T. Raynaud’s disease and preganglionic sympathectomy. Clin Sci 1938; 3: 320–36
Freedman RR, Sabharal SC, Desai N. Increased alpha-adrenergic responsiveness in idiopathic Raynaud’s disease. Arth Rheum 1989; 32(1): 61–5
Brotzu G, Falchi S, Mannu B, et al. The importance of presynaptic beta receptors in Raynaud’s disease. J Vasc Surg 1989; 9(6): 767–71
Carter SA, Dean E, Kroeger EA. Apparent finger systolic pressures during cooling in patients with Raynaud’s syndrome. Circulation 1988; 77(5): 988–96
Lau C, O’Dowd A, Belch JJF. White cell activation in the Raynaud’s phenomenon of systemic sclerosis and vibration induced white finger syndrome. Ann Rheum Dis 1992; 1(2): 249–52
Belch JJF, Drury J, McLaughlin K, et al. Abnormal biochemical and cellular parameters in the blood of patients with Raynaud’s phenomenon. Scott Med J 1987; 32(1): 12–4
Belch JJF, Zoma AA, Richards IM, et al. Vascular damage and factor VIII related antigen in the rheumatic diseases. Rheumatol Int 1987; 7: 107–11
Belch JF, McLaren M, Anderson J, et al. Increased prostacyclin metabolites and decreased red cell deformability in patients with systemic sclerosis and Raynaud’s syndrome. Prostaglandins Leukot Med 1985 Jan; 17: 1–9
Belch JJF, O’Dowd A, Forbes CF, et al. Platelet sensitivity to a prostacyclin analogue in systemic sclerosis. Br J Rheumatol 1986; 24: 346–50
Zamora MR, O’Brien RF, Rutherford RB, et al. Serum endothelin-1 concentrations and cold provocation in primary Raynaud’s phenomenon. Lancet 1990; 336: 1144–7
Kahaleh MB, Smith EA, Soma Y, et al. Effect of lymphotoxin and tissue necrosis factor on endothelial and connective cell growth and function. Clin Immunol Immunopathol 1988; 49: 261–72
LeRoy EC, Smith EA, Kahaleh MB, et al. A strategy for determining the pathogenesis of systemic sclerosis: is transforming growth factor-beta the answer? Arthritis Rheum 1989; 32: 817–25
Malamet R, Wise RA, Ettinger WH. Nifedipine in the treatment of Raynaud’s phenomenon — evidence for inhibition of platelet activation. Am J Med 1985; 78(4): 602–8
Smith CD, McKendry JR. Controlled trial of nifedipine in the treatment of Raynaud’s phenomenon. Lancet 1982 Dec 11; II: 1299–301
Roddeheffer RJ, Rommer JA, Wigley F, et al. Controlled double-blind trial of nifedipine in the treatment of Raynaud’s phenomenon. N Engl J Med 1983; 308: 880–3
Sauza J, Kraus A, Gonzalez-Amaro R, et al. Effect of the calcium channel blocker nifedipine on Raynaud’s phenomenon: a controlled double blind trial. J Rheumat 1984; 11(3): 362–3
Kahan A, Weber S, Amor B, et al. Calcium entry blocking agents in digital vasospasm (Raynaud’s phenomenon). Eur Heart J 1983; 4 Suppl. C: 123–9
Finch MB, Copeland S, Passmore AP, et al. A double-blind cross-over study of nifedipine retard in patients with Raynaud’s phenomenon. Clin Rheumatol 1988; 7(3): 359–65
Waller DG, Challenor VF, Francis DA, et al. Clinical and rheological effects of nifedipine in Raynaud’s phenomenon. Br J Clin Pharmacol 1986; 22: 449–54
Kahan A, Amor B, Menkes CJ. A randomised double-blind trial of diltiazem in the treatment of Raynaud’s phenomenon. Ann Rheum Dis 1985; 44(1): 30–3
Leppert J, Jonasson T, Nilsson H. The effect of isradipine, a new calcium-channel antagonist, in patients with primary Raynaud’s phenomenon: a single-blind dose-response study. Cardiovasc Drugs Ther 1989; 3(3): 397–401
Cook NJ, Armstrong RD, Roper SMB, et al. Amlodipine in the treatment of Raynaud’s phenomenon. Br J Rheumatol 1993; 32(6): 524–5
Kinney EL, Nicholas GG, Gallo J, et al. The treatment of severe Raynaud’s phenomenon with verapamil. J Clin Pharmacol 1982; 22: 74–6
Miller FW, Love LA. Prevention of predictable Raynaud’s phenomenon by sublingual nifedipine. N Engl J Med 1987; 317: 1476
Smith CR, Rodeheffer RJ. Treatment of Raynaud’s phenomenon with calcium channel blockers. Am J Med 1985; 78 Suppl. 2B: 39–42
Davinroy M, Mosnier M. Double-blind clinical evaluation of naftidrofuryl in Raynaud’s phenomenon. Sem Hop 1993; 69(36): 12–8
Nilsen KH. Effects of naftidrofuryl on microcirculatory cold sensitivity in Raynaud’s phenomenon. BMJ 1979; 1: 20–1
Murphy R. The effect of inositol nicotinate (Hexopal) in patients with Raynaud’s phenomenon. Clin Trials J 1985; 22(6): 521–9
Sunderland GT, Belch JJF, Sturrock RD, et al. A double blind randomised placebo controlled trial of Hexopal in primary Raynaud’s disease. Clin Rheumatol 1988; 7(1): 46–9
Aylward M. Hexopal in Raynaud’s Disease. J Int Med Res 1979; 7: 484
Holti G. An experimentally controlled evaluation of the effect of inositol nicotinate upon the digital blood flow in patients with Raynaud’s phenomenon. J Int Med Res 1979; 7: 473
Ring EFJ, Porto LO, Bacon PA. Quantitative thermal imaging to assess inositol nicotinate treatment for Raynaud’s syndrome. J Int Med Res 1981; 9: 393–400
Stellin GP, Waxman K. Current and potential therapeutic effects of pentoxifylline. Compr Ther 1989; 15: 11–3
Mihajlovic D, Hadzi-Pesic LJ, Markovic V, et al. Experiences with pentoxifylline in the treatment of peripheral vascular disease. Curr Med Res Opin 1979; 6 Suppl. 4: 43–8
Schmidt C, Marquis P, Royer RJ, et al. Clinical and hemodynamic study of pentoxifylline in diseases of the peripheral vessels. Ann Med Nancy 1976; 15: 61–5
Neirotti M, Longo F, Molaschi M, et al. Functional vascular disease: treatment with pentoxifylline [abstract]. 28th Annual Meeting of the International College of Angiology, Nice. Angiology 1986; 37: 397–8
Stefenelli T, Silberbauer K, Glogar D. Pentoxifylline/placebo/ nifedipine in patients with Raynaud’s phenomenon: influence on frequency of attacks and rewarming time. Klin Wochenschr 1986; 64: 1155–6
Newman ED, Davis DE, Harrington TM. Double blind placebo controlled trial of pentoxifylline in the treatment of primary and secondary Raynaud’s phenomenon [abstract no. D180]. Arthritis Rheum 1989; 34(9): 193
Aylward M, Bater PA, Davies DE, et al. Long-term monitoring of the effects of thymoxamine hydrochloride tablets in the management of patients with Raynaud’s disease. Curr Med Res Opin 1982; 8(3): 158–70
Jaffe GV, Grimshaw JJ. Thymoxamine for Raynaud’s disease and chilblains. Br J Clin Pract 1980; 34: 11–2
Grigg MJ, Nicolaides AN, Papadakis K, et al. The efficacy of thymoxamine in primary Raynaud’s phenomenon. Eur J Vasc Surg 1989; 3: 309–13
Belch JJF, Greer IA, McLaren M, et al. The effects of intravenous infusion of ZK36374, a synthetic prostacyclin derivative, on normal volunteers. Prostaglandins 1984; 28(1): 67–78
Belch JJF. Prostaglandins in Raynaud’s phenomenon. In: Vane J, O’Grady J, editors. Therapeutic applications of prostaglandins. London: Edward Arnold, 1993: 219–39
Martin MFR, Dowd PM, Ring EFJ, et al. Prostaglandin E1 infusions for vascular insufficiency in progressive systemic sclerosis. Ann Rheum Dis 1981; 40: 350–4
Belch JJF, Drury JK, Capell H, et al. Intermittent epoprostenol (prostacyclin) infusion in patients with Raynaud’s syndrome — a double-blind controlled trial. Lancet 1983; I: 313–5
Rademaker M, Thomas RHM, Provost G, et al. Prolonged increase in digital blood flow following iloprost infusion in patients with systemic sclerosis. Postgrad Med J 1987; 63: 617–20
Wigley FM, Wise RA, Seibold JR, et al. Intravenous iloprost infusion in patients with Raynaud Phenomenon secondary to systemic sclerosis. Ann Intern Med 1994; 120: 199–206
Torley HI, Madhok R, Capell HA, et al. A double-blind, randomised, multicentre comparison of two doses of intravenous iloprost in the treatment of Raynaud’s phenomenon secondary to connective tissue diseases. Ann Rheum Dis 1991; 50: 800–4
Rademaker M, Cooke ED, Almond NE, et al. Comparison of intravenous infusions of iloprost and oral nifedipine in treatment of Raynaud’s phenomenon in patients with systemic sclerosis: a double-blind randomised study. BMJ 1989; 298: 561–4
Lau CS, McLaren M, Saniabadi A, et al. The pharmacological effects of cicaprost, an oral prostacyclin analogue, in patients with Raynaud’s syndrome secondary to systemic sclerosis — a preliminary study. Clin Exp Rheumatol 1991; 9: 271–3
Murai C, Sasaki T, Osaki H, et al. Oral limaprost for Raynaud’s phenomenon. Lancet 1989; I: 1218
Belch JJF, Capell HA, Cooke ED, et al. Oral iloprost as a treatment for Raynaud’s syndrome: a double-blind multi-centre placebo controlled study. Ann Rheum Dis 1995; 54(3): 197–200
Belch JJF, Shaw B, Sturrock RD, et al. Double-blind trial of CL 115,347, a transdermally absorbed prostaglandin E2 analogue, in treatment of Raynaud’s phenomenon. Lancet 1985; I: 1180–3
Belch JJF, Cormie J, Newman P, et al. Dazoxiben, a thromboxane synthetase inhibitor, in the treatment of Raynaud’s syndrome: a double-blind trial. Br J Clin Pharmacol 1983; 15: 1135–6
Belch JJF, Shaw B, O’Dowd A, et al. Evening primrose oil (Efamol) in the treatment of Raynaud’s phenomenon: a double blind study. Thromb Haemost 1985; 54(2): 490–4
DiGacomo RA, Kremer JM, Shah DM. Fish-oil dietary supplementation in patients with Raynaud’s phenomenon: a double-blind, controlled, prospective study. Am J Med 1989; 86: 158–64
Coffmann JD, Clement DL, Creager MA, et al. International study of ketanserin in Raynaud’s phenomenon. Am J Med 1989; 87: 264–8
Shawket S, Dickerson C, Hazleman B, et al. Prolonged effect of CGRP in Raynaud’s patients: a double-blind randomised with prostacyclin. Br J Clin Pharmacol 1991; 32: 209–13
Bunker CB, Terenghi G, Springall DR, et al. Deficiency of calcitonin gene-related peptide in Raynaud’s phenomenon. Lancet 1990; 336: 1530–3
Hansteen V. Medical treatment in Raynaud’s disease. Acta Chir Scand 1976; 465: 87–91
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Belch, J.F., Ho, M. Pharmacotherapy of Raynaud’s Phenomenon. Drugs 52, 682–695 (1996). https://doi.org/10.2165/00003495-199652050-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199652050-00006