Summary
Synopsis
Trimetrexate is a folinic acid analogue structurally related to methotrexate, whose primary mechanism of action is believed to be inhibition of dihydrofolate reductase. This reduces the production of DNA and RNA precursors and leads to cell death. Trimetrexate is lipophilic and can passively diffuse across cell membranes including those of Pneumocystis carinii and its mammalian host. To minimise toxicity, trimetrexate must be coadministered with calcium folinate (leucovorin calcium), a reduced folate coenzyme, which is transported into, and protects, mammalian host cells but not P. carinii cells.
In noncomparative trials trimetrexate was effective in the treatment of P. carinii pneumonia (PCP) in patients with AIDS who were intolerant of or refractory to cotrimoxazole (trimethoprim/sulfamethoxazole) and pentamidine treatment. In these patients, 2- to 4-week survival rates of 48 to 69% were reported. In a comparative trial in the initial therapy of PCP, trimetrexate was less effective than cotrimoxazole in moderate to severe disease as evidenced by a significantly higher failure rate.
Trimetrexate was better tolerated than cotrimoxazole when used in this setting, however. Significantly fewer patients receiving trimetrexate plus calcium folinate discontinued treatment because of adverse events than did patients receiving cotrimoxazole. The most common adverse effect associated with trimetrexate is myelosuppression (neutropenia and thrombocytopenia); this is mitigated by coadministration of calcium folinate and is generally reversible upon dosage reduction or discontinuation. Other adverse effects include increases in serum aminotransferase levels, anaemia, fever, rash/pruritus, and increased alkaline phosphatase or serum creatinine levels.
Further research into the use of trimetrexate, including its efficacy as prophylaxis, in combination with other agents and as an oral formulation, is needed to clearly define its role in the treatment of PCP and to identify patients most likely to benefit. Currently, trimetrexate should be considered as an alternative treatment option in immunocompromised patients with moderate to severe PCP who have not responded to or are intolerant of first-line therapy.
Pharmacodynamic Properties
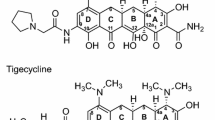
Trimetrexate is a folate antagonist structurally related to methotrexate but distinguished by its lipophilic properties which allow it to enter cells independently of the folate membrane transport system. Mammalian cells have this transport system but Pneumocystis carinii does not. Thus, trimetrexate can enter P. carinii cells while hydrophillic compounds such as calcium folinate (leucovorin calcium) cannot.
The mechanism of action of trimetrexate has not been fully elucidated; however, it is believed to be primarily due to inhibition of dihydrofolate reductase (DHFR). This inhibition reduces production of thymidylate and purines (DNA and RNA precursors) and leads to cell death. Host cells are protected from the cytotoxicity of trimetrexate by administration of calcium folinate, which is a fully reduced folate that enters the cell via the folate membrane transport system and can be directly utilised in cellular metabolism.
In vitro, trimetrexate showed greater binding affinity for P. carinii DHFR and was more effective than trimethoprim or pyrimethamine in inhibiting P. carinii DHFR activity. Trimetrexate was less effective than sulfamethoxazole or pentamidine but more so than trimethoprim in its ability to inhibit incorporation of para-aminobenzoic acid by P. carinii in the de novo synthesis of reduced folates. Trimetrexate has also been shown to inhibit P. carinii cultured with human embryonic lung fibroblast cells and in immunosuppressed rodent models of P. carinii pneumonia (PCP).
Pharmacokinetic Properties
The majority of pharmacokinetic data with trimetrexate were obtained from patients being treated for cancer although limited studies have been performed in patients with AIDS receiving treatment for PCP. Most pharmacokinetic parameters are relatively consistent between patient populations and treatment regimens although there tends to be wide interpatient variability.
After oral administration the mean bioavailability of trimetrexate is 44% with peak plasma concentrations achieved within 0.5 to 4 hours. Following intravenous administration there is a linear relationship between trimetrexate dose, and area under the plasma concentration-time curve and steady-state plasma concentrations. Distribution into other compartments is not well described, although data from a small number of patients have shown that trimetrexate distributes well into the respiratory tract but very poorly into the CNS.
The primary route of elimination appears to be via hepatic metabolism (via cytochrome P450), as less than one-third of the drug is excreted unchanged in the urine. Trimetrexate is transformed to at least 2 metabolites, both of which inhibit DHFR. The elimination curve of trimetrexate is best described by either a biexponential or triexponential model with the elimination half-life reported to range from 4 to 12 hours in patients with AIDS and PCP and from 8 to 26 hours in patients with cancer.
Therapeutic Potential
Noncomparative trials [including the large (n = 577) Treatment IND program] using trimetrexate as salvage therapy in patients with AIDS and PCP who were refractory to or intolerant of cotrimoxazole (trimethoprim/sulfamethoxazole) and pentamidine, reported 2- to 4-week survival rates ranging from 48 to 69%. Response rates ranged from 42 to 90% when assessed in patients with a variety of disease and treatment histories.
In a randomised comparison with cotrimoxazole, trimetrexate (as initial therapy) was less effective but better tolerated. Treatment with trimetrexate resulted in a significantly higher failure rate (38 vs 20% at day 21) compared with cotrimoxazole. However, because discontinuation due to serious adverse effects was significantly more common in the cotrimoxazole group (see tolerability summary for details), the number of patients receiving their assigned treatment at the end of the 3-week study was similar in both groups.
Tolerability
In patients with cancer, the main dose-limiting adverse effect of trimetrexate is myelosuppression, particularly neutropenia and thrombocytopenia. In these patients in whom concomitant calcium folinate is not used, there is a linear relationship between plasma trimetrexate concentration and haematological toxicity. This haematological toxicity is usually readily reversible upon dosage reduction or discontinuation. In patients with PCP, myelosuppression can be prevented or minimised by concurrent administration of calcium folinate. Other adverse effects include elevated serum aminotransferase levels, anaemia, fever, rash/pruritus and increased alkaline phosphatase or serum creatinine levels.
Trimetrexate plus calcium folinate is better tolerated than cotrimoxazole when used in patients with AIDS for the initial treatment of PCP. In a comparative trial, discontinuation rates at day 21 due to adverse effects were 28% in patients treated with cotrimoxazole compared with 8% in patients treated with trimetrexate.
Dosage and Administration
In the treatment of immunocompromised patients with moderate to severe PCP, the recommended dosage of trimetrexate is 45 mg/m2/day infused intravenously over 60 to 90 minutes for 21 days. Calcium folinate 80 mg/m2/day, either orally or intravenously in 4 divided doses, must be used concomitantly and continued for 3 days beyond the completion of trimetrexate treatment. Dosage adjustments of both drugs may be required to limit neutropenia and thrombocytopenia.
Similar content being viewed by others
References
Huan SD, Legha SS, Raber MN, et al. Phase I studies of trimetrexate using single and weekly dose schedules. Invest New Drugs 1991 May; 9: 199–206.
Lin JT, Bertino JR. Update on trimetrexate, a folate antagonist with antineoplastic and antiprotozoal properties. Cancer Invest 1991; 9 (2): 159–72.
Jackson RC, Fry DW, Boritzki TJ, et al. Biochemical pharmacology of the lipophilic antifolate, trimetrexate. Adv Enzyme Regul 1984; 22: 187–206.
Allegra CJ, Hoang K, Yeh GC, et al. Evidence for direct inhibition of de novo purine synthesis in human MCF-7 breast cells as a principal mode of metabolic inhibition by methotrexate. J Biol Chem 1987 Oct 5; 262: 13520–6.
Kim SN, MacDonald JR. Protection from trimetrexate toxicity in dogs with leucovorin coadministration [abstract]. FASEB J 1990 Feb 28; 4:A884.
MacDonald JR, Courtney CL, Pegg DG. Leucovorin protection against repeated daily dose toxicity of trimetrexate in rats. Fundam Appl Toxicol 1993 Aug; 21: 244–52.
Lerza R, Mencoboni M, Bogliolo G, et al. Leucovorin antagonizes the effects of trimetrexate on mouse hemopoietic progenitors. Anticancer Res 1991 Mar-Apr; 11: 613–6.
Browman GP, Spiegl P, Booker L, et al. Comparison of leucovorin protection from variety of antifolates in human lymphoid cell lines. Cancer Chemother Pharmacol 1985; 15: 111–4.
Sloand E, Laughon B, Armstrong M, et al. The challenge of Pneumocystis carinii culture. J Euk Microbiol 1993; 40 (2): 188–95.
Queener SF, Bartlett MS, Jay MA, et al. Activity of lipid-soluble inhibitors of dihydrofolate reductase against Pneumocystis carinii in culture and in a rat model of infection. Antimicrob Agents Chemother 1987 Sep; 31: 1323–7.
Davey Jr RT, Masur H. Recent advances in the diagnosis, treatment, and prevention of Pneumocystis carinii pneumonia. Antimicrob Agents Chemother 1990 Apr; 34: 499–504.
Kovacs JA, Allegra CJ, Beaver J, et al. Characterization of de novo folate synthesis in Pneumocystis carinii and Toxoplasma gondii: potential for screening therapeutic agents. J Infect Dis 1989 Aug; 160: 312–20.
Allegra CJ, Kovacs JA, Drake JC, et al. Activity of antifolates against Pneumocystis carinii dihydrofolate reductase and identification of a potent new agent. J Exp Med 1987 Mar 1; 165: 926–31.
Broughton MC, Queener SF. Pneumocystis carinii dihydrofolate reductase used to screen potential antipneumocystis drugs. Antimicrob Agents Chemother 1991 Jul; 35: 1348–55.
Allegra CJ, Chabner BA, Tuazon CU, et al. Trimetrexate for the treatment of Pneumocystis carinii pneumonia in patients with the acquired immunodeficiency syndrome. N Engl J Med 1987 Oct 15; 317: 978–85.
Rogers P, Allegra CJ, Murphy RF, et al. Bioavailability of oral trimetrexate in patients with acquired immunodeficiency syndrome. Antimicrob Agents Chemother 1988 Mar; 32: 324–6.
Smit MJ, DeGroot R, VanDongen JJ, et al. Trimetrexate efficacy and pharmacokinetics during treatment of refractory Pneumocystis carinii pneumonia in an infant with severe combined immunodeficiency disease. Pediatr Infect Dis J 1990 Mar; 9: 212–4 (discussion 215).
Kovacs JA, Allegra CJ, Kennedy S, et al. Efficacy of trimetrexate, a potent lipid-soluble antifolate, in the treatment of rodent Pneumocystis carinii pneumonia. Am J Trop Med Hyg 1988 Nov; 39: 491–6.
Walzer PD, Foy J, Steele P, et al. Activities of antifolate, antiviral, and other drugs in an immunosuppressed rat model of Pneumocystis carinii pneumonia. Antimicrob Agents Chemother 1992 Sep; 36: 1935–42.
Marshall JL, DeLap RJ. Clinical pharmacokinetics and pharmacology of trimetrexate. Clin Pharmacokinet 1994 Mar; 26: 190–200.
Freij BJ, Wientzen Jr RL, Hayek G, et al. Pharmacokinetics of trimetrexate glucuronate in infants with AIDS and Pneumocystis carinii pneumonia. Ann N Y Acad Sci 1993 Oct 29; 693: 302–5.
Allegra CJ, Jenkins J, Weiss RB, et al. A phase I and pharma-cokinetic study of trimetrexate using a 24-hour continuous-infection schedule. Invest New Drugs 1990 May; 8: 159–66.
Balis FM, Patel R, Luks E, et al. Pediatric phase I trial and pharmacokinetic study of trimetrexate. Cancer Res 1987 Sep 15; 47: 4973–6.
Fanucchi MP, Walsh TD, Fleisher M, et al. Phase I and clinical pharmacology study of trimetrexate administered weekly for three weeks. Cancer Res 1987 Jun 15; 47: 3303–8.
Grochow LB, Noe DA, Dole GB, et al. Phase I trial of trimetrexate glucuronate on a five-day bolus schedule: clinical pharmacology and pharmacodynamics. J Natl Cancer Inst 1989 Jan 18; 81: 124–30.
Ho DWH, Covington WP, Legha SS, et al. Clinical pharmacology of trimetrexate. Clin Pharmacol Ther 1987 Sep; 42: 351–6.
Hudes GR, LaCreta F, Walczak J, et al. Pharmacokinetic study of trimetrexate in combination with cisplatin. Cancer Res 1991 Jun 15; 51: 3080–7.
Lin JT, Cashmore AR, Baker M, et al. Phase I studies with trimetrexate: clinical pharmacology, analytical methodology, and pharmacokinetics. Cancer Res 1987 Jan 15; 47: 609–16.
Reece PA, Morris RG, Bishop JF, et al. Pharmacokinetics of trimetrexate administered by five-day continuous infusion to patients with advanced cancer. Cancer Res 1987 Jun 1; 47: 2996–9.
Stewart JA, McCormack JJ, Tong W, et al. Phase I clinical and pharmacokinetic study of trimetrexate using a daily x5 schedule. Cancer Res 1988 Sep 1; 48: 5029–35.
Grochow LB, Noe DA, Ettinger DS, et al. A phase I trial of trimetrexate glucuronate (NSC 352122) given every 3 weeks: clinical pharmacology and pharmacodynamics. Cancer Chemother Pharmacol 1989 Oct; 24: 314–20.
McCormack JJ, Webster LK, Tong WP, et al. Studies of a metabolite of trimetrexate. Proc Amer Assoc Cancer Res 1986; 27: 256.
Webster LK, Tong WP, McCormack JJ. Effect of trimethoprim, paracetamol and cimetidine on trimetrexate metabolism by rat perfused isolated livers. J Pharm Pharmacol 1987 Nov; 39: 942–4.
US Bioscience. Trimetrexate glucuronate prescribing information. West Conshohocken, PA.
Sattler FR, Frame P, Davis R, et al. Trimetrexate with leucovorin versus trimethoprim-sulfamethoxazole for moderate to severe episodes of Pneumocystis carinii pneumonia in patients with AIDS: a prospective, controlled multicenter investigation of the AIDS Clinical Trials Group Protocol 029/031. J Infect Dis 1994 Jul; 170: 165–72.
Sattler FR, Allegra CJ, Verdegem TD, et al. Trimetrexateleucovorin dosage evaluation study for treatment of Pneumocystis carinii pneumonia. J Infect Dis 1990 Jan; 161: 91–6.
Feinberg J, Hafner R, et al. An open, prospective, non-comparative trial of trimetrexate with leucovorin protection for Pneumocystis carinii pneumonia in AIDS patients refractory to or intolerant of conventional therapies for Pneumocystis carinii pneumonia. US Bioscience Study, data on file. Jan, 1993.
Bishop JF, Raghavan D, Olver IN, et al. A phase I study of trimetrexate (NSC 352122) administered by 5-day continuous intravenous infusion. Cancer Chemother Pharmacol 1989 Oct; 24: 246–50.
Grem JL, King SA, Costanza ME, et al. Hypersensitivity reactions to trimetrexate. Invest New Drugs 1990 May; 8: 211–4.
Kovacs JA, Masur H. Pneumocystis carinii pneumonia: therapy and prophylaxis. J Infect Dis 1988 Jul; 158: 254–9.
Stringer JR, Edman JC, Cushion MT, et al. The fungal nature of Pneumocystis. J Med Vet Mycol 1992; 30 Suppl. 1: 271–8.
Vöhringer H-F, Arastéh K. Pharmacokinetic optimisation in the treatment of Pneumocystis carinii pneumonia. Clin Pharmacokinet 1993 May; 24: 388–412.
Smith D, Gazzard B. Treatment and prophylaxis of Pneumocystis carinii pneumonia in AIDS patients. Drugs 1991 Oct; 42: 628–39.
Medina I, Mills J, Leoung G, et al. Oral therapy for Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. A controlled trial of trimethoprim-sulfamethoxazole versus trimethoprim-dapsone. N Engl J Med 1990 Sep 20; 323 (12): 776–82.
Hardy WD, Bozzette S, Safrin S, et al. Results from recent therapeutic trials for opportunistic infections (OIs) from the United States. AIDS 1994; 8 Suppl. 4: S15.
Toma E, Fournier S, Dumont M, et al. Clindamycin/primaquine versus trimethoprim-sulfamethoxazole as primary therapy for Pneumocystis carinii pneumonia in AIDS: a randomized, double-blind pilot trial. Clin Infect Dis 1993 Aug; 17: 178–84.
Hughes W, Leoung G, Kramer F, et al. Comparison of atovaquone (566C80) with trimethoprim-sulfamethoxazole to treat Pneumocystis carinii pneumonia in patients with AIDS. N Engl J Med 1993 May 27; 328 (21): 1521–7.
Smith DE, Davies S, Smithson J, et al. Eflornithine versus cotrimoxazole in the treatment of Pneumocystis carinii pneumonia in AIDS patients. AIDS 1992; 6: 1489–93.
Stevens RC, Laizure SC, Williams CL, et al. Pharmacokinetics and adverse effects of 20-mg/kg/day trimethoprim and 100-mg/kg/day sulfamethoxazole in healthy adult subjects. Antimicrob Agents Chemother 1991 September; 35 (9): 1884–90.
Sattler FR, Cowan R, Nielson DM, et al. Trimethoprim-sulfamethoxazole compared with pentamidine for treatment of Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome: a prospective, noncrossover study. Ann Intern Med 1988; 109: 280–7.
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: C.J. Allegra, NCI-Navy Medical Oncology Branch, National Cancer Institute, Bethesda, Maryland, USA; J.R. Bertino, Molecular Pharmacology and Therapeutics, Sloan-Kettering Institute for Cancer Research, New York, New York, USA; B.G. Gazzard, Chelsea and Westminster Hospital, London, England; P-M. Girard, Service de Maladies Infectieuses et Tropicales, Hôpital Rothschild, Paris, France; L.M. Kuitert, Department of Thoracic Medicine, National Heart and Lung Institute, London, England; J.L. Marshall, Division of Hematology/Oncology, Vincent T. Lombardi Cancer Center, Washington DC, USA; S.F. Queener, Department of Pharmacology and Toxicology, Indiana University School of Medicine, Indianapolis, Indiana, USA; Y. Varthalitis, 1st Department of Medical Oncology, Metaxa’s Memorial Cancer Hospital, Piraeus, Greece; J. Weits, Department of Internal Medicine, University Hospital Groningen, Groningen, The Netherlands.
Rights and permissions
About this article
Cite this article
Fulton, B., Wagstaff, A.J. & McTavish, D. Trimetrexate. Drugs 49, 563–576 (1995). https://doi.org/10.2165/00003495-199549040-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199549040-00007