Summary
Synopsis
Halofantrine is an orally administered blood schizontocide which is active against both chloro-quine-sensitive and chloroquine-resistant plasmodia. Dose-finding and noncomparative clinical trials have confirmed the efficacy of halofantrine in the treatment of falciparum malaria in areas of chloroquine- and sulfonamide/pyrimethamine-resistant malaria and vivax malaria. However, poor results obtained in patients who failed mefloquine prophylaxis suggest that the efficacy of halofantrine may not extend to mefloquine-resistant P. falciparum, although more studies are needed to confirm this. Data concerning halofantrine in the treatment of P. ovale and P. malariae infections are still limited. One comparative study indicates that halofantrine has an efficacy equivalent to that of mefloquine and may be better tolerated.
Halofantrine is generally well tolerated in both adults and children, the most common drugassociated effects being abdominal pain, pruritus, vomiting, diarrhoea, headache and rash, although it is difficult to distinguish between disease- and treatment-related events.
The development of parasite resistance to halofantrine, like other blood schizontocides, is inevitable. Poor absorption resulting in variable peak plasma halofantrine concentrations, and possible cross-resistance with mefloquine, may accelerate the emergence of resistance to halofantrine. Thus, it is of primary importance that halofantrine is used only in areas where chloroquine- and sulfonamide/pyrimethamine-resistance are established in order to preserve and sustain its efficacy. If used with care, halofantrine will provide an important treatment option for falciparum malaria, a widespread parasitic disease associated with considerable morbidity against which the number of effective drugs available is being increasingly compromised by the spread of resistance.
Pharmacological Properties
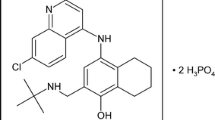
In vitro, halofantrine has demonstrated activity against both chloroquine-sensitive (IC50 1.5 to 2.5 µg/L) and chloroquine-resistant (1.3 to 3.9 µg/L) strains of Plasmodium falciparum. These observations are supported by in vivo data from animal models of both P. berghei and P. falciparum infections. Halofantrine demonstrated activity about 3 times greater than that of chloroquine in mice infected with P. berghei. In humans, halofantrine 250mg administered every 6 hours for 3 days cleared parasitaemia in volunteers experimentally infected with P. vivax and multidrug-resistant and chloroquine-sensitive strains of P. falciparum. Recrudescence occurred after single-dose treatment.
Halofantrine is a blood schizontocide and thus is active against the erythrocytic stages of Plasmodium spp. Data concerning the possible mechanism of action of halofantrine are contradictory although there is some support for the formation of a halofantrine-ferriprotoporphyrin IX complex, a mode of action similar to that proposed for other blood schizontocides. Inhibition of a proton pump at the host-parasite interface has also been hypothesised as an alternative mode of action.
Most endemic malarious areas are now affected by chloroquine resistance. While the susceptibility of P. falciparum to halofantrine has been confirmed in a number of countries, in vitro cross-resistance with mefloquine has been documented although the full clinical relevance of this observation has yet to be clarified.
Halofantrine is poorly and variably absorbed. The rate and extent of absorption is dramatically improved with food. In patients with falciparum malaria, peak plasma concentrations of 0.9 to 1.2 mg/L were achieved after about 16 hours following treatment with a 3-dose oral regimen of halofantrine (500mg 6-hourly). Elimination half-lives of halofantrine and its pharmacologically active metabolite, N-desbutylhalofantrine, ranged from 91 to 113 and 79 to 118 hours, respectively; the long half-life of the metabolite may encourage the selection of resistant strains. Plasma clearance was 0.58 L/h/kg. According to animal data, halofantrine is distributed widely in tissues and is excreted mainly in the faeces.
Therapeutic Efficacy
Dose-finding and noncomparative studies have confirmed the efficacy of halofantrine in the treatment of falciparum malaria in areas of chloroquine and sulfonamide/pyrimethamine resistance. Cure rates of 83 to 100% have been reported in noncomparative trials in adults and children after treatment with the recommended 3-dose regimen of halofantrine (500mg 6-hourly). Treatment is accompanied by clearance of parasitaemia within 34 to 78 hours and fever within 18 to 101 hours. Other symptoms of malaria also show evidence of improvement, usually on the first day of treatment. Splenomegaly and hepatomegaly cleared in around three-quarters of affected patients in the follow-up period after treatment. In an overview of 1474 patients with malaria, parasitaemia was not cleared in 0.5% of patients and the recrudescence rate was 5.8%. The majority of treatment failures observed with halofantrine have been attributed to incomplete drug absorption, although frequently there have been insufficient data to eliminate the possibility of decreased parasite susceptibility or resistance. In some studies, patients remained in endemic areas and recrudescence may have been attributable to reinfection. The efficacy of halofantrine in the treatment of P. vivax infections has also been established, but experience in the treatment of P. ovale and P. malariae infections is very limited.
Halofantrine appears to be as effective as single-dose mefloquine in falciparum malaria according to one large comparative trial conducted in Thailand. However, the results of a more recent comparative trial were suggestive of parasite resistance to halofantrine in eastern Thailand. A failure rate of 30% with halofantrine in patients who failed mefloquine prophylaxis provides some support for in vitro data indicating that there is cross-resistance between halofantrine and mefloquine. Although further studies are needed to support these findings, these observations suggest that the activity of halofantrine may not be optimal against mefloquine-resistant P. falciparum.
Tolerability
The incidence of treatment-related adverse events in almost 2000 patients treated with halofantrine was estimated to be 0.81/100 patients. The most commonly reported drug-related effects were abdominal pain, pruritus, vomiting, diarrhoea, headache and rash. However, the relationship between halofantrine treatment and adverse effects is difficult to determine in patients with malaria because many such symptoms are also disease-related.
Pruritus associated with halofantrine treatment has been found to be milder, of shorter duration and to occur less frequently than that associated with chloroquine. This observation may be important for African patients, about 8 to 20% of whom are unable to tolerate chloroquine because of treatment-related pruritus.
In animal studies, there has been no evidence of genotoxicity, teratogenicity or any effects on male fertility; however, embryotoxicity has been reported.
Dosage and Administration
The recommended dosage regimen of halofantrine is 500mg in adults or 8 mg/kg in children, administered orally for 3 doses at 6-hourly intervals. A second course of treatment given after 7 days is advised for nonimmune patients and young children. Halofantrine is contraindicated in pregnant and lactating women and is not recommended for use in causal or suppressive prophylactic regimens.
Similar content being viewed by others
References
Adagu SI, Lege-Oguntoye L, Ugbode, Okoyah JN, Asuku ZA, et al. Preliminary results of investigations on the in vivo/in vitro sensitivity of P. falciparum to halofantrine in Zaria, Northern Nigeria. European Journal of Pharmacology 183: 1025–1026, 1990
Ambroise-Thomas P, Ranque P, Dumbo O, Goulier A, Peyron F, et al. Halofantrine in the treatment of P. falciparum malaria in Mali (152 cases). Abstract 1268. IXth International Congress of Infectious and Parasitic Diseases, Munich, July 20–26, 1986.
Ambroise-Thomas P, Rossignol JF. Chemotherapy of resistant falciparum malaria. Parasitology Today 2: 79–80, 1986
Baudon D, Bernard J, Martet G, Touze JE, Lantrade P, et al. Halofantrine to prevent falciparum malaria on return from malarious areas. Lancet 2: 377, 1990
Bernard J, Sarrouy J, Dupasquier I, Lesbordes JL, Gimenez M, et al. Treatment of imported Plasmodium falciparum malaria by halofantrine: 59 cases treated. Medecine Tropicale 50: 167–171, 1990
Blauer G. Interaction of ferriprotoporphyrin IX with the antimalarials amodiaquine and halofantrine. Biochemistry International 17: 729–734, 1988
Boudreau EF, Pang LW, Dixon KE, Webster HK, Pavanand K, et al. Malaria: treatment efficacy of halofantrine (WR 171,669) in initial field trials in Thailand. Bulletin of the World Health Organization 66: 227–235, 1988
Boudreau EF, Webster HK, Pavanand K, Thosingha L. Type II mefloquifle resistance in Thailand. Lancet 2: 1335, 1982
Braendli B, Loutan L, Markwalder K, Bock HL. Treatment of acute malaria with halofantrine in Switzerland — preliminary results of a clinical study. 17th International Congress of Chemotherapy, Berlin, June, 1991
Brasseur P, Kouamouo J, Moyou RS, Druilhe P. Emergence of mefloquine-resistant malaria in Africa without drug pressure. Lancet 2: 59, 1990
Broom C. Human Pharmacokinetics of halofantrine hydrochloride. Parasitology Today (Suppl.): 15–20, 1989
Bunnag D, Viravan C, Looareesuwan S, Karbwang J, Harinasuta T, et al. Comparison of the efficacy of halofantrine and mefloquine in multidrug resistant P. falciparum malaria in Thailand. Abstract 84-C12. Bulletin Société Française de Parasitologie 8 (Suppl. 1): 420, 1990
Bygbjerg IC, Schapira A, Flachs H, Gomme G, Jepsen S. Mefloquine resistance of falciparum malaria from Tanzania enhanced by treatment. Lancet 1: 774–775, 1983
Camilleri P, Thorpe CJ. Fluorescence detection of the enantiomers of halofantrine at picomole levels using chiral high-performance liquid chromatography. Journal of Chromatography 519: 387–390, 1990
Camilleri P, Dyke C, Hossner F. Chiral separation of the optical isomers of the antimalarial drug halofantrine. Journal Of Chromatography 477: 471–471, 1989
Canfield CJ. Antimalarial aminoalcohol alternatives to mefloquine. Acta Tropica 37: 232–237, 1980
Carme B, Gay F, Chandenier J, Ndounga M, Ciceron L, et al. Unexpected trend in chemosensitivity of Plasmodium falciparum in Brazzaville, Congo. Lancet 2: 582–583, 1991
Carroll FI, Berrang B, Linn CP. Resolution of antimalarial agents via complex formation with α-(2,4,5,7-tetranitro-9-fluorenyli-deneaminooxy) propionic acid. Journal of Medicinal Chemistry 21: 326–330, 1978
Childs GE, Boudreau EF, Wimonwattrawatee T, Pang L, Milhous WK. In vitro and clinical correlates of mefloquine resistance of Plasmodium falciparum in eastern Thailand. American Journal of Tropical Medicine and Hygiene 44: 553–559, May 1991
Childs GE, Wimonwattrawatee T, Pooyindee N. Evaluation of an in vitro assay system for drug susceptibility of field isolates of Plasmodium falciparum from southern Thailand. American Journal of Tropical Medicine and Hygiene 38: 19–23, 1988
Childs GE, Pang L, Wimonwattrawatee T, Pooyindee N, Nanakorn A, et al. In vitro mefloquine resistance of Plásmodium falciparum isolated from the Burmese border region of Thailand. South East Asian Journal of Tropical Medicine and Public Health 18: 438–443, 1987
Childs GE, Lambros C, Notsch JD, Pamplin CL, Davidson DE Jr. Comparison of in vitro and in vivo antimalarial activities of 9-phenanthrenecarbinols. Annals of Tropical Medicine and Parasitology 78: 13–20, 1984
Chitchang S, Wongteptien S. A clinical trial of halofantrine in acute uncomplicated malaria in Thai soldiers. Parasitology Today (Suppl.): 21–26, 1989
Cosgriff TM, Boudreau EF, Pamplin CL, Doberstyn EB, Desjardins RE, et al. Evaluation of the antimalarial activity of the phenanthrenemethanol halofantrine (WR 171,669). American Journal of Tropical Medicine and Hygiene 31: 1075–1079, 1982
Cosgriff TM, Pamplin CL, Canfield CJ, Willet GP. Mefloquine failure in a case of falciparum malaria induced with a multidrug-resistant isolate in a non-immune subject. American Journal of Tropical Medicine and Hygiene 34: 692–693, 1985
Coulaud JP, Le Bras J, Matheron S, Moriniere B, Saimot AG, et al. Treatment of imported cases of falciparum malaria in France with halofantrine. Transactions of the Royal Society of Tropical Medicine and Hygiene 80: 615–616, 1986
Cowman AF, Foote SJ. Chemotherapy and drug resistance in malaria. International Journal for Parasitology 20: 503–513, 1990
Deloron P, Le Bras J, Ramanamirija JA, Coulanges P. Plasmodium falciparum in Madagascar: in vivo and in vitro sensitivity to seven drugs. Annals of Tropical Medicine and Parasitology 79: 357–365, 1985
Desjardins RE, Canfield CJ, Haynes JD, Chulay JD. Quantitative assessment of antimalarial activity in vitro by a semiautomated microdilution technique. Antimicrobial Agents and Chemotherapy 16: 710–718, 1979
Editorial. Halofantrine in the treatment of malaria. Lancet 2: 537–538, 1989
Ekanem OJ, Weisfeld JS, Salako LA, Nahlen BL, Ezedinachi EN, et al. Sensitivity of Plasmodium falciparum to chloroquine and sulfadoxine/pyrimethamine in Nigerian children. Bulletin of the World Health Organization 68: 45–52, 1990
Ezeamuzie IC, Igbigbi PS, Ambakederemo AW, Abila B, Nwaejike IN. Halofantrine-induced pruritus amongst subjects who itch to chloroquine. Journal of Tropical Medicine and Hygiene 94: 184–188, 1991
Felix R, Gay F, Lyagoubi A, Bustos MDG, Diquet B, et al. Cross resistance with mefloquine and halofantrine in a case of falciparum malaria contracted in Sierra Leone. Bulletin de la Société de Pathologie Exotique et de ses Filiales 83: 43–45, 1990
Fleckenstein L, Pamplin III CL, von Bredow J, Heiffer MH, Canfield CJ. Comparative pharmacokinetics (PK) of new antimaterials. Abstract B49. Clinical Pharmacology and Therapeutics 33: 234, 1983
Foote S, Cowman A. Drug resistance in malaria: a developing disaster? Todays Life Science: 18–24, 1989
Gawienowski M, Benet LZ, Fleckenstein L, Lin ET. Ion-paired liquid chromatographic method for the analysis of blood and plasma for the antimalarial drug halofantrine and its putative mono-debutylated metabolite. Journal of Chromatography 430: 412–419, 1988
Gay F, Binet MH, Bustos MDG, Rouveix B, Danis M, et al. Mefloquine failure in child contracting falciparum malaria in West Africa. Lancet 1: 120–121, 1990a
Gay F, Bustos DG, Diquet B, Rojas Rivero L, Litaudon M, et al. Cross-resistance between mefloquine and halofantrine. Lancet 2: 1262, 1990b
Gay F, Bustos D, Caumes E, Litaudon M, Diquet B, Datry A, et al. Insuffisance d’une cure d’halofantrine sur un paludisme a Plasmodium falciparum chloroquinoresistant contracté en Sierra Leone. Annales de Médecine Interne 141: 493–494, 1990c
Geary TG, Divo AA, Jensen JB. Activity of quinolone-containing antimalarials against chloroquine-sensitive and -resistant strains of Plasmodium falciparum in vitro. Transactions of the Royal Society of Tropical Medicine and Hygiene 81: 499–503, 19
Geary TG, Divo AA, Jensen JB. Stage specific actions of antimalarial drugs on Plasmodium falciparum in culture. American Journal of Tropical Medicine and Hygiene 40: 240–244, 1989
Hallwood PM, Horton RJ, O’Sullivan KM, Parr SN. Halofantrine and pruritus. Lancet 2: 397–398, 1989
Hiremath CB. Absorption, distribution, and excretion of α-(2-di-n-butyl-amino-ethyl)-1,3, dichloro-6-trifluoromethyl-9-phen-anthrene methanol-C14 hydrochloride (WR-171,669-C14) in rats and rhesus monkeys. Abstract 1478. Pharmacology 33: 472, 1974
Hoffman SL, Dimpudus AJ, Campbell JR, Marwoto HA, Sukri N, et al. RII and RIII type resistance of Plasmodium falciparum to combination of mefloguine and sulfadoxine/pyrimethamine in Indonesia. Lancet 2: 1039–1040, 1985
Horton RJ, Parr SN, Bokor LC. Clinical experience with halofantrine in the treatment of malaria. Drugs Under Experimental and Clinical Research 16: 497–503, 1990
Horton RJ, Parr SN. Halofantrine: an overview of efficacy and safety. Parasitology Today (Suppl.): 65–79, 1989
Horton RJ. Introduction of halofantrine for malaria treatment. Parasitology Today 4: 238–239, 1988
Karbwang J, Milton KA, Na Bangchang K, Ward SA, Edwards G, et al. Pharmacokinetics of halofantrine in Thai patients with acute uncomplicated falciparum malaria. British Journal of Clinical Pharmacology 31: 484–487, 1991
Keeratithakul D, Teja-Isavadharm P, Shanks GD, Webster HK, Edstein MD. An improved high-performance liquid Chromatographie method for the simultaneous measurement of halofantrine and desbutylhalofantrine in human serum. Therapeutic Drug Monitoring 13: 64–68, 1991
Khan MA, Rehman GN, Qazi SA. Halofantrine hydrochloride-efficacy and safety in children with acute malaria. Journal of the Pakistan Medical Association 40: 8–10, 1991
Lambros C, Davis DR, Lewis GE Jr. Antimalarial drugs susceptibility of Plasmodium falciparum isolates from forest fringe dwelling aborigines (Orang Asli) of peninsular Malaysia. American Journal of Tropical Medicine and Hygiene 41: 3–8, 1989
Le Bras J, Hatin I, Trape JF, Diallo S, Verdier F. Susceptibility of Plasmodium falciparum to mefloquine in an urban area in Senegal. Abstract S4. D17. Bulletin Société Française de Parasitologie 8 (Suppl. 1): 461, 1990
Louis JP, Hengy C, Louis FJ, Gazin P, Jambou R, Gardon J, et al. Surveillance epidemiologique de la chimiosensibilite de Plasmodium falciparum aux antimalariques au Cameroun (tests in-vivo et in-vitro). International Symposium on Malaria, p. 58, Marseille, June 13–15, 1991
McLaughlin GL, Decrind C, Dayal-Drager R, Hassan-King M, Subramanian S, et al. Optimization of a rapid nonisotopic DNA probe assay for Plasmodium falciparum in the Gambia. Journal of Clinical Microbiology 29: 1517–1519, 1991
Maegraith B. In Adams & Maegraith Clinical and tropical diseases, 7th ed., Blackwell Scientific Publications, Oxford, 1980
Maisonneuve H, Joly F, John M, Carles G, Rossignol JF. Effectiveness of halofantrine in Plasmodium falciparum and Plasmodium vivax malaria in a resistance area (French Guiana). Presse Médicale 17: 99–102, 1988
Mashako MNL, Kingway MP, Kayembe N. Treatment of falciparum malaria with halofantrine hydrochloride in a drug resistant region. Analysis of 54 pediatrie cases. Annales de la Société Belge de Médecine Tropicale 70: 25–32, 1990
Milton KA, Edwards G, Ward SA, Orme ML’E, Breckenridge AM. Pharmacokinetics of halofantrine in man: effects of food and dose size. British Journal of Clinical Pharmacology 28: 71–77, 1989
Milton KA, Ward SA, Edwards G. Determination of halofantrine and its principal metabolite desbutylhalofantrine in biological fluids by reversed-phase high-performance liquid chromatography. Journal of Chromatography 433: 339–344, 1988
Monson MH, Kyle DE, Ayoade M, Oduola J, Broadbent P. Multiple drug resistance of Plasmodium falciparum in Liberia. Transactions of the Royal Society of Tropical Medicine and Hygiene 83: 311–312, 1989
Nosten F, ter Kuile F, Chongsuphajaisiddhi T, Na Bangehang K, Kwarbang J, et al. Mefloquine pharmacokinetics and resistance in children with acute falciparum malaria. British Journal of Clinical Pharmacology 31: 556–559, 1991a
Nosten F, ter Kuile F, Chongsuphajaisiddhi T, Luxemburger C, Webster HK, et al. Mefloquine-resistant falciparum malaria on the Thai-Burmese border. Lancet 1: 1140–1143, 1991b
Oduola AMJ, Milhous WK, Weatherly NF, Bowdre JH, Desjardins RE. Plasmodium falciparum: induction of resistance to mefloquine in cloned strains by continuous drug exposure in vitro. Experimental Parasitology 67: 354–360, 19
Oduola AMJ, Salako LA, Milhous WK, Walker O, Desjardins RE. Reduced in-vitro susceptibility to mefloquine in West African isolates of Plasmodium falciparum. Lancet 2: 1304–1305, 1987
Panisko DM, Keystone JS. Treatment of malaria — 1990. Drugs 39: 160–189, 1990
Parkinson D, Balmer V, Ajdukiewicz A, Korinohowa A, Kere N. The effectiveness of halofantrine for the treatment of acute malaria in adults in the Solomon Islands. Parasitology Today (Suppl.): 27–35, 1989
Peters W. Changing pattern of antimalarial drug resistance. Journal of the Royal Society of Medicine 82: 14–17, 1989
Peters W. Plasmodium: resistance to antimalarial drugs. Annales de Parasitologie Humaine et Comparee 65: 103–106, 1990
Peters W, Robinson BL, Ellis DS. The chemotherapy of rodent malaria XLII. Halofantrine and halofantrine resistance. Annals of Tropical Medicine and Parasitology 81: 639–646, 1987
Phillips RE, Looareesuwan S, White NJ, Chanthavanich P, Karbwang J, et al. Hypoglycaemia and antimalarial drugs: quinidine and release of insulin. British Medical Journal 292: 1319–1321, 1986
Rab SM, Saeed Sheikhani M, Mahmoud SA, Jaffary SIH. The efficacy of halofantrine hydrochloride in acute malaria: a study of 74 patients from Karachi, Pakistan. Parasitology Today (Suppl.): 37–44, 1989
Raccurt CP, Ribou G, Lambert MT, Bouloumie J, Macaigne F, et al. Halofantrine in the malaria treatment. Bulletin de la Société de Pathologie Exotique et de ses Filiales 82: 368–372, 1989
Richard-Lenoble D, Kombila M, Martz M, Gendrel D, Gendrel C, et al. Efficacy, safety and acceptability of halofantrine in the treatment of acute Plasmodium falciparum malaria in African children (Gabon). Parasitology Today (Suppl.): 59–63, 1989
Rieckmann KH, Sax LJ, Campbell GH, Mrema JE. Drug sensitivity of Plasmodium falciparum: an in-vitro microtechnique. Lancet 1: 22–23, 1978
Rinehart J, Arnold J, Canfield CJ. Evaluation of two phenan-threnemethanols for antimalarial activity in man: WR 122,455 and WR 171,669. American Journal of Tropical Medicine and Hygiene 25: 769–774, 1976
Ringwald P, Le Bras J, Voyer C, Coulaud J-P. Reduced in vitro susceptibility to halofantrine of Plasmodium falciparum in West Africa. Lancet 1: 421–422, 1990
Roblot F, Becoq-Giraudon B, Roué R, Litaudon M, Breux J-P, et al. Crise convulsive au cours d’un traitement par halofantrine. Abstract S4. C62. Bulletin Société Française de Parasitologie 8 (Suppl.1): 445, 1990
Rojas Rivera L, Gay F, Bustos DG, Turk P, Poirier L, et al. In vitro cross-resistance between mefloquine and halofantrine in Plasmodium falciparum induced by mefloquine. Abstract S9. D31. Bulletin Société Française de Parasitologie 8 (Suppl. 1): 1118, 1990
Roué R, Debord T. Preliminary results. Efficacy, safety of halofantrine in the treatment of a first Plasmodium falciparum malaria attack in adults. Abstract TuP-1-6. Excerpta Medica International Congress Series no. 810: 129, 1988
Salako LA, Sowunmi A, Walker O. Evaluation of the clinical efficacy and safety of halofantrine in falciparum malaria in Ibadan, Nigeria. Transactions of the Royal Society of Tropical Medicine and Hygiene 84: 644–647, 1990
Schildbach S, Wernsdorfer WH, Suebsaeng L, Rooney W. In vitro sensitivity of multiresistant Plasmodium falciparum to new candidate antimalarial drugs in Western Thailand. Southeast Asia Journal of Tropical Medicine and Public Health 21: 29–38, 1990
Schmidt LH, Crosby R, Rasco J, Vaughan D. Antimalarial activities of various 9-phenanthrenemethanols with special attention to WR-122,455 and WR-171,669. Antimicrobials Agents and Chemotherapy 14: 292–314, 1978
Schuster BG, Canfield CJ. Preclinical studies with halofantrine. Parasitology Today (Suppl.): 3–13, 1989
Shanks GD, Watt G, Edstein MD, Webster HK, Suriyamongkol V, et al. Halofantrine for the treatment of mefloquine chemoprophylaxis failures in Plasmodium falciparum infections. American Journal of Tropical Medicine and Hygiene 45: 488–491, 1991
Simon F, Le Bras J, Gaudebout C, Girard PM. Reduced sensitivity of Plasmodium falciparum to mefloquine in West Africa. Lancet 1: 467–468, 1988
Smrkovski LL, Buck RL, Alcantara AK, Rodriguez CS, Uylanco CV. In vitro mefloquine resistant Plasmodium falciparum from the Philippines. Lancet 2: 322, 1982
Sowunmi A, Walker O, Salako LA. Pruritus and antimalarial drugs in Africans. Lancet 2: 213, 1989
Veenendaal JR, Parkinson AD, Kere N, Rieckmann KH, Edstein MD. Pharmacokinetics of halofantrine and n-desbutylhalofantrine in patients with falciparum malaria following a multiple dose regimen of halofantrine. European Journal of Clinical Pharmacology 41: 161–164, Aug 1991
Warhurst DC, Diribe CO. Effect of halofantrine on the proton pump of intraerythocytic Plasmodium berghei. Abstract TuP-1-8. Excerpta Medica International Congress Series no. 810: 129, 1988
Warhurst DC. Antimalarial interaction with ferriprotoporphyrin IX monomer and its relationship to activity of the blood schizontocides. Annals of Tropical Medicine and Parasitology 81: 65–67, 1987
Warrell DA. Treatment of severe malaria. Journal of the Royal Society of Medicine 82 (Suppl. 17): 44–51, 1989
Watkins WM, Lury JD, Kariuki D, Koech DK, Oloo JA, et al. Efficacy of multiple-dose halofantrine in treatment of chloroquine-resistant falciparum malaria in children in Kenya. Lancet 2: 247–250, 1988
Webster HK, Boudreau EF, Pavanand K, Yongvanitchit K, Pang LW. Antimalarial drug susceptibility testing of Plasmodium falciparum in Thailand using a microdilution radioisotope method. American Journal of Tropical Medicine and Hygiene 34: 228–235, 1985a
Webster HK, Thaithong S, Pavanand K, Yongvanitchit K, Pinswasdi C, et al. Cloning and characterization of mefloquine-resistant Plasmodium falciparum from Thailand. American Journal of Tropical Medicine and Hygiene 34: 1022–1027, 1985b
Wellems TE, Walker-Jonah A, Panton LJ. Genetic mapping of the chloroquine-resistance locus on Plasmodium falciparum chromosone 7. Proceedings of the National Academy of Sciences of the United States of America 88: 3382–3386, 1991
Wirima J, Molyneux ME, Khoromana C, Gilles HM. Clinical trials with halofantrine hydrochloride in Malawi. Lancet 2: 250–252, 1988
WHO. International travel and health: vaccination requirements and health advice, WHO, Geneva, 1991
WHO Scientific Group on the Chemotherapy of Malaria. Practical chemotherapy of malaria: report of a WHO scientific group. WHO Technical Report Series no. 805, 1990
WHO Drug Information. Halofantrine in malaria. WHO Drug Information 2: 58–60, 1988
Wyler DJ. Plasmodium species (malaria). In Mandell et al. (Eds) Principles and Practice of Infectious Diseases, pp. 2056–2066, Churchill Livingstone, New York, 1990
Wyler DJ. Malaria — resurgence, resistance and research (first of two parts). New England Journal of Medicine 308: 875–940, 1983
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: G.E. Childs, Department of Chemical Information, Walter Reed Army Medical Institute of Research, Washington, DC, USA; A.F. Cowman, The Walter and Eliza Hall Institute of Medical Research, Royal Melbourne Hospital, Victoria, Australia; F. Gay, Département de Parasitologie et de Santé Publique, Hôpital Pitié Salpêzêtrière, Paris, France; J. Karbwang, Hospital for Tropical Diseases, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand; J. Le Bras, Centre National de Reference pour la Chimiosensibilite du Paludisme, Hôpital Bichat-Claude Bernard, Paris, France; K.A. Milton, Department of Pharmacology and Therapeutics, University of Liverpool, Liverpool, England; D.M. Panisko, Tropical Disease Unit, Toronto General Hospital, Toronto, Ontario, Canada; W. Peters, London School of Hygiene and Tropical Medicine (University of London), St Albans, Hertfordshire, England; J.R. Veneendaal, Army Malaria Research Unit, Milpo, Ingelburn, New South Wales, Australia.
Rights and permissions
About this article
Cite this article
Bryson, H.M., Goa, K.L. Halofantrine. Drugs 43, 236–258 (1992). https://doi.org/10.2165/00003495-199243020-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199243020-00009