Summary
Synopsis: Omeprazole1 is a substituted benzimidazole derivative which markedly inhibits basal and stimulated gastric acid secretion. It has a unique mode of action, irreversibly blocking the so-called proton pump of the parietal cell which is supposedly the terminal step in the acid secretory pathway.
In animals, on a weight basis, omeprazole is 2 to 10 times more potent than cimetidine in inhibiting gastric acid secretion. Toxicological studies in rats have shown that very high doses of omeprazole administered for 2 years produce hyperplasia of gastric enterochromaffin-like cells and carcinoids, a few with proliferations into the submucosa. The significance of such findings to the clinical situation is wholly speculative and requires further research. Preliminary studies in patients with duodenal ulcers or Zollinger-Ellison syndrome have found no mucosal changes which would suggest that the drug represents a risk for development of carcinoid tumours at therapeutic dosages.
In patients with duodenal ulcers omeprazole, at dosages of at least 20mg once daily, produced ulcer healing rates of between 60 and 100% after 2 weeks and between 90 and 100% after 4 weeks, even in patients resistant to treatment with H2-receptor antagonists. Comparative trials clearly demonstrated that omeprazole 20 to 40mg administered once daily was significantly more effective than usual dosage regimens of cimetidine and ranitidine in healing duodenal ulcers during 2 to 4 weeks of treatment. At present no data are available evaluating omeprazole as maintenance therapy once ulcers have healed. Other clinical trials have also shown that omeprazole is effective for treating gastric ulcers, ulcerative peptic oesophagitis, and Zollinger-Ellison syndrome. In patients with Zollinger-Ellison syndrome the profound and long lasting antisecretory activity of omeprazole may make it the drug of choice for treating the massive acid hypersecretion associated with the disease, especially when H2-receptor antagonists are ineffective. During clinical trials reported to date omeprazole has been very well tolerated but further clinical experience is essential to fully evaluate its safety profile.
Thus, omeprazole represents a pharmacologically unique antisecretory drug which is very effective for rapidly healing peptic ulcers and peptic oesophagitis, and for reducing gastric acid hypersecretion in patients with Zollinger-Ellison syndrome. If the apparent absence of undesirable mucosal morphological changes during treatment with usual doses in patients with peptic ulcer disease is confirmed, it may be a major advance in the treatment of these diseases.
Pharmacodynamic Studies: In vitro and in vivo animal studies demonstrated that omeprazole produces long lasting inhibition of gastric acid secretion which is likely due to non-competitive binding of a proton-activated derivative to parietal cell (H+/K+)-ATPase. Such a mechanism, at the terminal stage of the acid secreting process, means a reduction of intragastric acidity can now be achieved independent of the nature of the primary stimulus. Comparative studies in animals found omeprazole to be some 2 to 10 times more potent than cimetidine on a weight basis.
Single-dose studies in man (healthy volunteers and patients with duodenal ulcer disease or Zollinger-Ellison syndrome) have shown that omeprazole inhibits both basal and stimulated gastric acid secretion in a dose-dependent manner. Following repeat once daily administration, omeprazole has an increasing effect on acid secretion which appears to stabilise after about 3 days. Short term studies indicate that 20 to 30mg once daily is the optimum dosage regimen in healthy volunteers and patients with duodenal ulcer disease in remission; this virtually abolishes gastric acidity within 6 hours and reduces stimulated acid output after 24 hours by 60 to 70%.
In addition to its effects on gastric acidity, omeprazole reduces the total volume of gastric juice secreted and inhibits pepsin output. However, these changes are not as consistent or as great as the effect on acid secretion. Omeprazole 0.35 mg/kg administered intravenously did not significantly affect basal or stimulated intrinsic factor secretion. Furthermore, omeprazole does not seem to have any significant influence on gastric emptying rate, or on the majority of gastrointestinal hormones — apart from gastrin. Short periods of treatment with omeprazole administered once daily usually resulted in elevated serum gastrin levels. Such hypergastrinaemia occurs secondary to a pronounced reduction of intragastric acidity, and returns to normal levels within 1 to 2 weeks of stopping treatment.
Orally, but not parenterally, administered omeprazole seems to be cytoprotective in some animal models of peptic ulcer disease such as Shay ulcers, stress-induced ulcers, and ulcers induced by various necrotising agents. The mechanisms involved are not fully understood but appear to be independent of the established antisecretory properties of omeprazole.
Toxicological studies in rats have demonstrated that supramaximal doses of omeprazole administered for long periods cause gastric enterochromaffin-like cell hyperplasia and carcinoids, a few with proliferations into the submucosa. It has been suggested that hypergastrinaemia, induced by the profound inhibition of gastric secretion causes these changes; their relevance to the therapeutic use of omeprazole remains speculative and further studies are required.
Pharmacokinetic Studies: The absorption characteristics of omeprazole are both formulation- and dose-dependent. Following administration of the drug as a buffered oral solution, buffered encapsulated uncoated granules, or as capsules of enteric-coated granules, mean peak plasma omeprazole concentrations were attained after 20 minutes, 30 minutes, and between 2 and 5 hours, respectively. Interestingly, increased doses of omeprazole produced disproportionately larger increases in mean peak plasma concentration and systemic availability. Similarly, repeat once daily administration for 5 to 7 days resulted in significant elevations of mean peak plasma concentration and area under the plasma concentration-time curve. Since omeprazole is acid labile, these findings could possibly indicate that the antisecretagogue improves its own absorption and relative bioavailability by inhibiting acid secretion. An alternative explanation involves saturation of enzymes responsible for the first-pass metabolism of omeprazole.
Following intravenous administration omeprazole plasma concentrations decline biexponentially. The apparent volume of distribution of omeprazole is about 0.3 to 0.4 L/kg which is compatible with localisation of the drug in extracellular water. Penetration of omeprazole into red blood cells is low, whereas its plasma protein binding is high — between 95 and 96% in human plasma.
Omeprazole is eliminated rapidly and almost completely by metabolism; no unchanged drug has been recovered in the urine. Following absorption, 3 metabolites of omeprazole have been identified: a sulphone derivative, a sulphide derivative and hydroxyomeprazole. Peak plasma concentrations of the sulphone metabolite are attained shortly after those of unchanged omeprazole, 0.4 to 1.7 hours after peak omeprazole concentrations following administration of capsules of enteric-coated granules. However, unidentified metabolites of omeprazole had a very similar plasma concentration-time curve as the parent drug — in terms of peak concentration and the time to achieve it. Following administration of 14C-omeprazole approximately 60% of total radioactivity is recovered in the urine within 6 hours. Over a 4-day period about 80% of the administered dose was recovered in the urine and the remainder in the faeces. Total plasma clearance is relatively high (32 to 40 L/h) and most studies have reported a mean elimination half-life of omeprazole in healthy subjects of between 0.5 and 1.5 hours (usually about 1 hour).
There are limited data available concerning the pharmacokinetic properties of omeprazole in patients with peptic ulcer disease or Zollinger-Ellison syndrome.
The pharmacokinetic profile of omeprazole does not seem to be altered in patients with chronic renal failure and is not influenced by haemodialysis.
Omeprazole plasma concentration does not correlate with its antisecretory activity at a given time-point; indeed, the drug markedly inhibits acid secretion long after plasma concentrations have decreased below detection limits. However, there does seem to be a significant correlation between antisecretory activity and area under the plasma concentration-time curve.
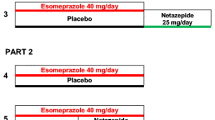
Therapeutic Trials: Clinical trials have demonstrated that omeprazole at dosages of at least 20mg once daily produces a duodenal ulcer healing rate of between 60 and 100% within 2 weeks and between 90 and 100% within 4 weeks. Dose-finding studies showed that an optimal dosage of omeprazole is between 20 and 40mg once daily. Open clinical studies have confirmed these very high rates of duodenal ulcer healing even in a small group of patients who were refractory to treatment with H2-receptor antagonists (alone or in combination with other antiulcer drugs). Appropriately designed comparative clinical trials clearly demonstrated that once-daily administration of omeprazole 20 to 40mg produces significantly more rapid healing of duodenal ulcers after 2 to 4 weeks of treatment than the H2-receptor antagonists cimetidine and ranitidine. Additionally, omeprazole 20mg and 40mg once daily elicited significantly greater symptom relief than ranitidine 150mg twice daily, whereas in 2 other studies 30mg and 20mg of omeprazole were indistinguishable from cimetidine 1000 mg/day and ranitidine 300 mg/day, respectively, in this respect. Other clinical studies have shown that omeprazole administered once daily may be effective for treating gastric ulcers and ulcerative peptic oesophagitis. Indeed, omeprazole 40mg once daily was significantly superior to ranitidine 150mg twice daily in 178 patients with reflux oesophagitis. Furthermore, in a double-blind multicentre trial in 184 outpatients with gastric ulceration, omeprazole 20mg once daily was as effective as ranitidine 150mg twice daily and healed 95% of gastric ulcers within 8 weeks.
In patients with Zollinger-Ellison syndrome, omeprazole is a highly potent and long acting antisecretagogue which many authors consider will become the drug of choice for controlling the massive acid hypersecretion associated with the disease. For patients with Zollinger-Ellison syndrome who are resistant to H2-receptor antagonists, omeprazole offers a valuable therapeutic alternative to surgery (partial or total gastrectomy) with its inherent risks.
Side Effects: Preliminary experience with omeprazole has found the antisecretagogue to be well-tolerated, producing no consistent side effects or changes in laboratory variables. Wider clinical usage with careful surveillance is needed to fully evaluate the side effect profile of omeprazole.
Dosage and Administration: The usual oral adult dosage of omeprazole seems to be 20mg once daily before breakfast for 2 to 4 weeks for duodenal ulcers and 4 to 8 weeks for gastric ulcers. In patients with Zollinger-Ellison syndrome omeprazole dosage should be individualised so that the smallest dose is administered which reduces gastric acid secretion to less than 10 mEq for the last hour before the next dose. At present, insufficient data are available for dosage recommendations in children.
Similar content being viewed by others
References
Allen JM, Adrian TE, Webster J, Howe A, Bloom SR. Effect of single dose of omeprazole on the gastrointestinal peptide response to food. Hepato-gastroenterology 31: 44–46, 1984
Bardhan KD, Bianch Porro G, Bose K, Hinchliffe RFC, Lazzaroni M, et al. Comparison of two different doses of omeprazole versus ranitidine in duodenal ulcer (DU) healing. Gut 26: A557–A558, 1985
Batzri S, Dubois A, Harmon JW, Moskowitz D. Demonstration of direct influence of histamine H2-receptors on gastric emptying in guinea pig using histamine antagonists and omeprazole. Gastroenterology 88: 1318, 1985
Batzri S, Weichbrod RH, Harmon JW, Dubois A. Acid secretion in a chronic awake guinea pig model: effects of omeprazole and cimetidine. Gastroenterology 86: 1022, 1984
Beil W, Hackbarth I. Acid activation of omeprazole is important for its selective action on parietal cell K+/H+-ATPase. Naunyn — Schmiedebergs Archives of Pharmacology 329 (Suppl.): R65, 1985
Beil W, Mädge S, Hannemann H, Zimmer KO, Sewing K-Fr. Characteristics of K+/H+-ATPase inhibition by omeprazole and omeprazole sulfide. Hepato-gastroenterology 32: 47, 1985
Beil W, Sewing K-Fr. Inhibition of partially purified K+/H+-ATPase from guinea-pig isolated and enriched parietal cells by substituted benzimidazoles. British Journal of Pharmacology 82: 651–657, 1984
Beil W, Sewing KF. Acid activation makes omeprazole a specific K+/H+-ATPase inhibitor. Gastroenterology 88: 1320, 1985
Berglindh T, Hansen D, Bergqvist E. Irreversible inhibition by omeprazole. The in vivo-in vitro connection. Gastroenterology 88: 1322, 1985
Berglindh T, Sachs G. Emerging strategies in ulcer therapy: pumps and receptors. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 7–14, 1985
Blanchi A, Delchier J-C, Soule J-C, Payen D, Bader J-P. Control of acute Zollinger-Ellison syndrome with intravenous omeprazole. Lancet 2: 1223–1224, 1982
Blanchi A, Rotenberg A, Soulé J-C, Delchier J-C, Morin T, et al. Traitement de l’ulcère duodénal en poussée par l’oméprazole. Gastroentérologie Clinique et Biologique 8: 943–946, 1984
Blom H. Effects of long term treatment with omeprazole on the gastric mucosal morphology. Scandinavian Journal of Gastroenterology 19(Suppl. 98): 55, 1984
Bowman WC, Rand MJ (Eds). Textbook of Pharmacology, 2nd ed., Blackwell Scientific Publications, Oxford, 1980
Brändström A, Lindberg P, Junggren U. Structure activity relationships of substituted benzimidazoles. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 15–22, 1985
Brogden RN, Carmine AA, Heel RC, Speight TM, Avery GS. Ranitidine. Drugs 24: 267–303, 1982
Brogden RN, Heel RC, Speight TM, Avery GS. Cimetidine. Drugs 15: 93–131, 1978
Bytzer P, Bekker C, Bukhave K, Rask-Madsen J. Gastric prostaglandin E2 release following acid reduction by cimetidine, omeprazole, and parietal cell vagotomy (PCV) in duodenal ulcer patients. Acta Medica Scandinavica (Suppl. 685): 47, 1984
Cederberg C, Ekenved G, Lind T, Olbe L. Acid inhibitory characteristics of omeprazole in man. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 105–112, 1985
Cederberg C, Lind T, Axelson M, Olbe L. Long term acid inhibitory effect of different daily doses of omeprazole 24 hours after dosing. Gastroenterology 86: 1043, 1984
Classen M, Dammann HG, Domschke W, Hengels KJ, Hüttemann W, et al. Kurzzeit-Therapie des Ulcus duodeni mit Omeprazol und Ranitidin. Deutsche Medizinische Wochenschrift 110: 210–215, 1985a
Classen M, Dammann HG, Domschke W, Hüttemann W, Londong W, et al. Abheilungsraten nach Omeprazol- und Ranitidin- Behandlung des Ulcus ventriculi. Deutsche Medizinische Wochenschrift 110: 628–633, 1985b
Cooperative Study. Omeprazole in duodenal ulceration: acid inhibition, symptom relief, endoscopic healing, and recurrence. British Medical Journal 289: 525–528, 1984
Daly MJ, Pottage A. Antisecretory drugs and gastric cancer. British Medical Journal 291: 900, 1985a
Daly MJ, Pottage A. Antisecretory drugs and gastric cancer. British Medical Journal 291: 1646–1647, 1985b
Dammann HG, Blum AL, Lux G, Rehner M, Riechen EO, et al. Unterschiedliche Heilungstendenz der Refluxösophagitis nach Omeprazol und Ranitidin. Deutsche Medizinische Wochenschrift 111: 123–128, 1986
Dammann HG, Müller P, Seitz HK, Simon B. Säuresekretionsverhalten unter einer mehrtägigen Omeprazol-Gabe. Schweizerische Medizinische Wochenschrift 113: 895–898, 1983
Défize J, Pals G, Frants RR, Westerveld BD, Festen HPM, et al. The influence of omeprazole on the synthesis and secretion of pepsinogen in isolated rabbit gastric glands. Biochemical Pharmacology 34: 3693–3699, 1985
Dent J, Downton J, Buckle P, Heddle R, Toouli J, et al. Omeprazole heals peptic esophagitis by elevation of intragastric pH. Gastroenterology 88: 1363, 1985
Dent J, Heddle R, Downton J, Mackinnon J, Toouli J, Lewis I. Omeprazole heals ulcerative peptic esophagitis. Gastroenterology 86: 1062, 1984
Ekman L, Hansson E, Havu N, Carlsson E, Lundberg C. Toxicological studies on omeprazole. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 53–69, 1985
Elashoff JD, Grossman MI. Smoking and duodenal ulcer. Gastroenterology 79: 181, 1980
Elder JB. Inhibition of acid and gastric carcinoids. Gut 26: 1279–1283, 1985
Festen HPM, Thijs JC, Lamers CBHW, Jansen JMBJ, Pals G, et al. Effect of oral omeprazole on serum gastrin and serum pepsinogen I levels. Gastroenterology 85: 1030–1034, 1984
Fiasse R, Tomé G, Dive Ch. L’Oméprazole, médicament d’avenir pour le traitment du syndrome de Zollinger-Ellison et de l’ulcère duodénal? Acta Gastro-Enterologica Belgica 47: 555–568, 1984
Fimmel CJ, Berger MM, Blum AL. Dissociated response of acid and pepsin secretion to omeprazole in an in vitro perfused mouse stomach. American Journal of Physiology 247: G240–G247, 1984
Fimmel CJ, Blum AL. Substituierte Benzimidazole — eine neue Dimension der Ulkustherapie? Wiener Klinische Wochenschrift 4: 149–153, 1984
Fryklund J, Wallmark B, Larsson H, Helander HF. Effect of omeprazole on gastric secretion in H+, K+-ATPase and in pepsinogen-rich cell fractions from rabbit gastric mucosa. Biochemical Pharmacology 33: 273–280, 1984
Ganser AL, Forte JG. K+-stimulated ATPase in purified microsomes of bullfrog oxyntic cells. Biochimica et Biophysica Acta 307: 169–180, 1973
Goto Y, Olbe L, Walsh JH, Debas HT. Prevention of stress ulceration by omeprazole is due to its antisecretory action. Gastroenterology 86: 1094, 1984
Gugler R, Jensen JC. Omeprazole inhibits elimination of diazepam. Lancet 1: 969, 1984
Gugler R, Jensen JC. Omeprazole inhibits oxidative drug metabolism. Gastroenterology 89: 1235–1241, 1985
Gustavsson S, Adami H-O, Lööf L, Nyberg A, Nyrén O. Rapid healing of duodenal ulcers with omeprazole. Lancet 2: 124–125, 1983
Gustin MC, Goodman DBP. Isolation of brush-border membrane from the rabbit descending colon epithelium. Partial characterization of a unique K+-activated ATPase. Journal of Biological Chemistry 256: 10651–10656, 1981
Helander HF. Stereological data on parietal and endocrine cells of the gastric corpus in patients treated with omeprazole. Gastroenterology 88: 1416, 1985
Helander H, Ramsay C-H, Regårdh C-G. Localization of omeprazole and metabolites in the mouse. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 95–104, 1985
Helander HF, Smolka A, Ramsay C-H, Sachs G, Fellenius E. Localization of gastric K+, H+-ATPase. Hepato-gastroenterology 30: 74, 1983
Henry DA, Gerkens JF, Brent P, Somerville K. Inhibition of drug metabolism by omeprazole. Lancet 2: 46–47, 1984a
Henry DA, Somerville KW, Kitchingman G, Langman MJS. Omeprazole: effects on oxidative drug metabolism. British Journal of Clinical Pharmacology 18: 195–200, 1984b
Hetzel DJ, Dent J, Laurence BH, Reed WD, Narielvala F, et al. Omeprazole heals reflux oesophagitis: a placebo controlled trial. Gut 27: A609, 1986
Hetzel DJ, Shearman DJC. Omeprazole inhibition of nocturnal gastric secretion in patients with duodenal ulcer. British Journal of Clinical Pharmacology 18: 587–590, 1984
Hoffmann K-J. Identification of the main urinary metabolites of omeprazole after an oral dose to rats and dogs. In press, 1986
Hoffmann K-J, Renberg L, Olovson S-G. Comparative metabolic disposition of oral doses of omeprazole in the dog, rat, and mouse. In press, 1986
Horowitz M, Hetzel DJ, Buckle PJ, Chatterton BE, Shearman DJC. The effect of omeprazole on gastric emptying in patients with duodenal ulcer disease. British Journal of Clinical Pharmacology 18: 791–794, 1984
Howden CW, Forrest JAH, Reid JL. Effects of single and repeated doses of omeprazole on gastric acid and pepsin secretion in man. Gut 25: 707–710, 1984a
Howden CW, Kenyon CJ, Beastall GH, Reid JL. Inhibition by omeprazole of adrencortical response to ACTH: clinical studies and experiments on bovine adrenal cortex in vitro. Clinical Science 70: 99–102, 1986
Howden CW, Meredith PA, Forrest JAH, Reid JL. Oral pharmacokinetics of omeprazole. European Journal of Clinical Pharmacology 26: 641–643, 1984b
Howden CW, Payton CD, Meredith PA, Hughes DMA, Macdougall AL, et al. Antisecretory effect and oral pharmacokinetics of omeprazole in patients with chronic renal failure. European Journal of Clinical Pharmacology 28: 637–640, 1985
Howden CW, Payton CD, Meredith PA, Macdougall AI, Reid JL, et al. Influence of haemodialysis on the antisecretory effect and oral pharmacokinetics of omeprazole in chronic renal failure. Gut 25: A1182, 1984c
Howden CW, Reid JL. Omeprazole, a gastric ‘proton pump inhibitor’: lack of effect on renal handling of electrolytes and urinary acidification. European Journal of Clinical Pharmacology 26: 639–640, 1984
Howden CW, Reid JL, Forrest JAH. Effect of omeprazole on gastric acid secretion in human volunteers. Gut 24: 497, 1983
Humphries, TJ, Ekenved G. The therapeutic dose response profit for oral omeprazole in the acute therapy of duodenal ulcer: a summary. American Journal of Gastroenterology 80: 861, 1985
Hüttemann W, Rotner HG, duBosque G, Rehner M, Hebbeln H, et al. 20 versus 30mg omeprazole once daily: effect on healing rates in 115 duodenal ulcer patients. Digestion 33: 117–120, 1986
Im WB, Blakeman DP, Davis JP. Irreversible inactivation of rat gastric (H+-K+)-ATPase in vivo by omeprazole. Biochemical and Biophysical Research Communications 126: 78–82, 1985a
Im WB, Blakeman DP, Sachs G. Reversal of antisecretory activity of omeprazole by sulfhydryl compounds in isolated rabbit gastric glands. Biochimica et Biophysica Acta 845: 54–59, 1985b
Im WB, Sih JC, Blakeman DP, McGrath JP. Omeprazole, a specific inhibitor of gastric (H+-K+)-ATPase, is a H+-activated oxidizing agent of sulfhydryl groups. Journal of Biological Chemistry 260: 4591–4597, 1985c
Jack D, Poynter D, Smith RN. Antisecretory drugs and gastric cancer. British Medical Journal 291: 675, 1985
Keeling DJ, Fallowfield C, Milliner KJ, Tingley SK, Ife RJ, et al. Studies on the mechanism of action of omeprazole. Biochemical Pharmacology 34: 2967–2973, 1985
Kittang E, Aadland E, Schjønsby H. Effect of omeprazole on the secretion of intrinsic factor, gastric acid and pepsin in man. Gut 26: 594–598, 1985
Kollberg B, Isenberg JI, Johansson C. Cytoprotective effect of omeprazole on the rat gastric mucosa. In Allen et al. (Eds) Mechanisms of mucosal protection in the upper gastrointestinal tract, pp. 351–356, Raven Press, New York, 1984
Konturek SJ, Brzozowski T, Radecki T. Protective action of omeprazole, a benzimidazole derivative, on gastric mucosal damage by aspirin and ethanol in rats. Digestion 27: 159–164, 1983
Konturek SJ, Cieszkowski M, Kwiecién N, Konturek J, Tasler J, et al. Effect of omeprazole, a substituted benzimidazole, on gastrointestinal secretions, serum gastrin, and gastric mucosal blood flow in dogs. Gastroenterology 86: 71–77, 1984a
Konturek SJ, Kweicién N, Obtutowicz W, Kopp B, Olesky J. Action of omeprazole (a benzimidazole derivative) on secretory responses to sham feeding and pentagastrin and upon serum gastrin and pancreatic polypeptide in duodenal ulcer patients. Gut 25: 14–18, 1984b
Korman MG, Hansky J, Eaves ER, Schmidt GT. Influence of cigarette smoking on healing and relapse in duodenal ulcer disease. Gastroenterology 85: 871–874, 1983
Lagerström P-O, Persson B-A. Determination of omeprazole and metabolites in plasma and urine by liquid chromatography. Journal of Chromatography 309: 347–356, 1984
Lamers CBHW, Jansen JBMJ. Inhibition of gastric acid secretion in Zollinger-Ellison syndrome by omeprazole, a potent and long-acting antisecretory drug. Gut 23: A907, 1982
Lamers CBHW, Lind T, Moberg S, Jansen JBMJ, Olbe L. Omeprazole in Zollinger-Ellison syndrome. New England Journal of Medicine 310: 758–761, 1984
Lamers CBHW, Teunissen L, Jansen JBMJ. Absorption of omeprazole in Zollinger-Ellison syndrome is accelerated by alkali. Gut 26: A1134–A1135, 1985
Langman MJS. Antisecretory drugs and gastric cancer. British Medical Journal 290: 1850–1852, 1985
Larsen KR, Maas VA, Carlsson E. The effects of omeprazole, a proton pump inhibitor, on pentagastrin-stimulated blood flow and oxygen consumption in the ex-vivo canine gastric chamber. Gastroenterology 86: 1153, 1984
Larson GM, Sullivan HW. Omeprazole, a long-lasting inhibitor of gastric secretion. Journal of Surgical Research 36: 503–507, 1984
Larsson H, Carlsson E, Håkansson R, Mattsson H, Sundler F. Relation of plasma gastrin concentrations and oxyntic mucosal ECL density during inhibition of gastric acid secretion in the rat. Gut 26: A558, 1985a
Larsson H, Carlsson E, Junggren U, Olbe L, Sjöstrand SE, et al. Inhibition of gastric acid secretion by omeprazole in the dog and rat. Gastroenterology 85: 900–907, 1983
Larsson H, Carlsson E, Mattsson H, Lundell L, Sundler F, et al. Plasma gastrin and gastric enterochromaffinlike cell activation and proliferation. Gastroenterology 90: 391–399, 1986
Larsson H, Carlsson E, Sundell G. Effects of omeprazole and cimetidine on gastric acid secretion and right atrial beating frequency in isolated organ preparations from the guinea pig. Digestion 29: 12–18, 1984
Larsson H, Mattson H, Sundell G, Carlsson E. Animal pharmacodynamics of omeprazole. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 23–26, 1985b
Larsson H, Ryberg B. Omeprazole increases K+ net flow during stimulated conditions in the mammalian gastric mucosa in vitro. Physiologist 26: A116, 1983
Lauritsen K, Rune SJ, Bytzer P, Kelbaek H, Jensen KG, et al. Effect of omeprazole and cimetidine on duodenal ulcer. New England Journal of Medicine 312: 958–961, 1985
Lee FI. Antisecretory drugs and gastric cancer. British Medical Journal 291: 1723, 1985
Lewin MJM. Oméprazole: un nouveau mécanisme d’action et une efficacité sans précédent dans le traitement de l’hypersécrétion acide gastrique. Gastroentérologie Clinique et Biologique 8: 939–942, 1984
Lind T, Cederberg C, Ekenved G, Haglund U, Olbe L. Effect of omeprazole — a gastric proton pump inhibitor — on pentagastrin stimulated acid secretion in man. Gut 24: 270–276, 1983
Lind T, Moore M, Olbe L. Intravenous omeprazole: effect on 24-hour intragastric pH in duodenal ulcer patients. In press, 1986
Lloyd-Davies KA, Rutgersson K, Sölvell L. Omeprazole in Zollinger-Ellison syndrome: four-year international study. Submitted for publication, 1986
Londong W, Londong V, Cederberg C, Steffen H. Dose-response study of omeprazole on meal-stimulated gastric acid secretion and gastrin release. Gastroenterology 85: 1373–1378, 1983
Lööf L, Adami H-O, Gustavsson S, Nyberg A, Nyrén O, Lundborg P. Omeprazole: no evidence for frequent hepatic reactions. Lancet 1: 1347–1348, 1984
Lorentzon P, Eklundh B, Brändström A, Wallmark B. The mechanism for inhibition of gastric (H+ + K+)-ATPase by omeprazole. Biochimica et Biophysica Acta 817: 25–32, 1985
Mattsson H, Andersson K, Larsson H. Omeprazole provides protection against experimentally induced gastric mucosal lesions. European Journal of Pharmacology 91: 111–114, 1983
Mattsson H, Carlsson K, Carlsson E. Omeprazole is devoid of effect on alkaline secretion in isolated guinea pig antral mucosa. In Allen et al. (Eds) Mechanisms of mucosal protection in the upper gastrointestinal tract, pp. 141–146, Raven Press, New York, 1984
McArthur KE, Collen MJ, Maton PN, Cherner JA, Howard JM, et al. Omeprazole: effective, convenient therapy for Zollinger-Ellison syndrome. Gastroenterology 88: 939–944, 1985
Mignon M, Alcabes G, Lehy T, Nguyen Phuoc BK, Vatier J, et al. Modifications sécrétoires, pHmétriques, et ultrastructurales gastriques au cours d’un traitment prolongé par l’oméprazole dans une forme sévère de syndrome de Zollinger-Ellison. Gastroentérologie Clinique et Biologique 8: 947–954, 1984
Mihaly GW, Prichard PJ, Smallwood RA, Yeomans ND, Louis WJ. Simultaneous high-performance liquid chromatographic analysis of omeprazole and its sulphone and sulphide metabolites in human plasma and urine. Journal of Chromatography 278: 311–319, 1983
Miyake H, Fukuda K, Masuda Y, Okabe S. Effects of a proton pump inhibitor, omeprazole, on healing of acetic acid-induced gastric ulcers in rats. Gastroenterology 88: 1504, 1985
Müller P, Dammann HG, Seitz H, Simon B, Kommerell B. Repeated omeprazole administration and human gastric secretion. Italian Journal of Gastroenterology 16: 6–8, 1984a
Müller P, Dammann HG, Simon B. Human acid secretion during and after 18 days’ treatment with omeprazole. Italian Journal of Gastroenterology 17: 96–97, 1985
Müller P, Dammann H-G, Simon B. Akute Schädigung der Magenschleimhaut durch Acetylsalicylsäure. Arzneimittel-Forschung 36: 265–268, 1986
Müller P, Seitz HK, Simon B, Dammann HG, Feurle G, et al. Vierwöchige Omeprazol-Gabe: Einfluβ auf Säureverhalten und basale Hormonspiegel. Zeitschrift für Gastroenterologie 22: 236–240, 1984b
Naesdal J, Andersson T, Bodemar G, Larsson R, Regårdh CG, et al. Pharmacokinetics of 14C omeprazole in patients with impaired renal function. Scandinavian Journal of Gastroenterology 20(Suppl. 113): 34, 1985a
Naesdal J, Bodemar G, Walan A. Effect of omeprazole, a substituted benzimidazole, on 24-h intragastric acidity in patients with peptic ulcer disease. Scandinavian Journal of Gastroenterology 19: 916–922, 1984
Naesdal J, Lind T, Bergsåker-Aspöy J, Bernklev T, Farup PG, et al. The rate of healing of duodenal ulcers during omeprazole treatment. Scandinavian Journal of Gastroenterology 20: 691–695, 1985b
Öberg K, Lindström H. Reduction of gastric hypersecretion in Zollinger-Ellison syndrome with omeprazole. Lancet 1: 66–67, 1983
Olbe L, Berglindh T, Elander B, Helander H, Fellenius E, et al. Properties of a new class of gastric acid inhibitors. Scandinavian Journal of Gastroenterology 14(Suppl. 55): 131–135, 1979
Penston J, Wormsley KG. H2-Receptor antagonists and gastric cancer. Medical Toxicology 1: 163–168, 1986
Pilbrant Å, Cederberg C. Development of an oral formulation of omeprazole. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 113–120, 1985
Piper DW (Ed.). Peptic ulcer, ADIS Press, Auckland, 1982
Pounder RE. Doudenal ulcers that will not heal. Gut 25: 697–702, 1984
Poynter D, Pick CR, Harcourt RA, Selway SAM, Ainge G, et al. Association of long lasting unsurmountable histamine H2 blockade and gastric carcinoid tumours in the rat. Gut 26: 1284–1295, 1985
Prichard PJ, Rubinstein D, Jones DB, Dudley FJ, Smallwood RA, et al. Double blind comparative study of omeprazole 10mg and 30mg daily for healing duodenal ulcers. British Medical Journal 290: 601–603, 1985a
Prichard PJ, Yeomans ND, Jones DB, Louis WJ, Smallwood RA. Effects of morning or evening dosage with 10mg omeprazole on 24 hour gastric pH in duodenal ulcer patients in remission. Gut 25: 1181, 1984
Prichard PJ, Yeomans ND, Mihaly GW, Jones DB, Buckle PJ, et al. Omeprazole: a study of its inhibition of gastric pH and oral pharmacokinetics after morning or evening dosage. Gastroenterology 88: 64–69, 1985b
Rabon E, Cuppoletti J, Malinowska D, Smolka A, Helander HF, et al. Proton secretion by the gastric parietal cell. Journal of Experimental Biology 106: 119–133, 1983
Rackur G, Bickel M, Fehlhaber H-W, Herling A, Hitzel V, et al. 2-([2-pyridylmethyl]sulfinyl)benzimidazoles: acid sensitive suicide inhibitors of the proton transport system in the parietal cell. Biochemical and Biophysical Research Communications 128: 477–484, 1985
Regårdh C-G, Gabrielsson M, Hoffman K-J, Löfberg I, Skåberg I. Pharmacokinetics and metabolism of omeprazole in animals and man — an overview. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 79–94, 1985
Saccomani G, Chang HH, Mihas AA, Crago S, Sachs G. An acid transporting enzyme in human gastric mucosa. Journal of Clinical Investigation 64: 627–635, 1979
Saccomani G, Shah G, Spenney G, Sachs G. Characterization of gastric mucosal membranes. VIII. Journal of Biological Chemistry 250: 4802–4809, 1975
Sachs G. Pump blockers and ulcer disease. New England Journal of Medicine 310: 785–786, 1984
Scandinavian Multicentre Study. Gastric acid secretion and duodenal ulcer healing during treatment with omeprazole. Scandinavian Journal of Gastroenterology 19: 882–884, 1984
Schulman N, Bank S, Kranz V. Effects of omeprazole on ethanol and cold-restraint stress induced gastric ulcers. Gastroenterology 86: 1239, 1984
Sewing K-Fr, Harms P, Schulz G, Hannemann H. Effect of substituted benzimidazoles on acid secretion in isolated and enriched guinea pig parietal cells. Gut 24: 557–560, 1983
Sewing KF, Beil W, Hannemann H. The in vitro inhibitory effect of omeprazole on parietal cell H+-transport is reversible. Gastroenterology 88: 1581, 1985
Sewing K-Fr, Hannemann H. Studies on the mechanism of action of omeprazole. Naunyn-Schmiedebergs Archives of Pharmacology 329 (Suppl.): R65, 1985
Sharma BK, Lundborg P, Pounder RE, Axelson M, Ohman M, et al. Acid secretory capacity after treatment with omeprazole. Gastroenterology 86: 1246, 1984a
Sharma BK, Santana IA, Walt RP, Pounder RE. Intragastric acidity after treatment with omeprazole. Gut 24: A973, 1983
Sharma BK, Santana IA, Wood EC, Walt RP, Pereira M, et al. Intragastric bacterial activity and nitrosation before, during, and after treatment with omeprazole. British Medical Journal 289: 717–719, 1984b
Sharma BK, Walt RP, Pounder RE, Gomes M De FA, Wood EC, Logan LH. Optimal dose of oral omeprazole for maximal 24 hour decrease of intragastric acidity. Gut 25: 957–964, 1984c
Skånberg I, Carlsson E, Karlsson A, Larsson H, Lofberg I, et al. The pharmacokinetics of omeprazole and correlation to inhibition of gastric acid secretion. Acta Physiologica Scandinavica 124(Suppl. 542): 266, 1985
Stachura J, Konturek SJ, Cieszkowsky M, Dabrós W, Zakrzewska J, et al. Comparison of the effect of omeprazole — a substituted benzimidazole — and ranitidine — a potent H2-receptor antagonist — on histamine-induced gastric acid secretion and the ultrastructure of canine parietal cells. Hepato-Gastroenterology 30: 205–210, 1983
Stenderup J, Mertz A, Wandall JH, Bonnevie O. The inhibition of gastric-acid secretion by Omeprazol in daily doses of 10 and 30mg. Scandinavian Journal of Gastroenterology Suppl. 98: 48, 1984
Stöckmann F, Fölsch UR, Bonatz G, Wülfrath M, Creutzfeldt W. Influence of a substituted benzimidazole (omeprazole) on rat gastric endocrine cells. Digestive Diseases and Sciences 29 (Suppl.): 835, 1984
Thompson JN, Barr JA, Collier N, Spencer J, Bush A, et al. Basal, sham feed and pentagastrin stimulated gastric acid, pepsin and electrolytes after omeprazole 20mg and 40mg daily. Gut 26: 1018–1024, 1985
Tytgat GNJ, Lamers CBHW, Wilson JA, Hameeteman W, Jansen JBMJ, et al. 100% healing with omeprazole of peptic ulcers resistant to histamine H2-receptor antagonists. Gastroenterology 88: 1620, 1985
Utley RJ, Salim ASM, Carter DC. Effect of cimetidine and omeprazole on aspirin- and taurocholate-induced gastric mucosal damage in the rat. Gut 26: 770–775, 1985a
Utley RJ, Wright R, Beastall GH, Carter DC. The effect of omeprazole on insulin induced gastric secretion in man. Scottish Medical Journal 30: 96–100, 1985b
Vezzadini P, Tomassetti P, Toni R, Bonora G, Labò G. Omeprazole in the medical treatment of Zollinger-Ellison syndrome. Current Therapeutic Research 35: 772–776, 1984
Walan A, Bardhan KD, Bianchi Porro G, Bose K, Hinchliffe RFC, et al. A comparison of two different doses of omeprazole versus ranitidine in duodenal ulcer healing. Gastroenterology 88: 1625, 1985
Walan A, Bergsåker-Aspöy J, Farup P, Gillberg R, Halvorsen L, et al. Four week study of the rate of duodenal ulcer healing with omeprazole. Gut 24: A972, 1983
Wallmark B, Brändström A, Larsson H. Evidence for acid-induced transformation of omeprazole into an active inhibitor of (H+ + K+)-ATPase within the parietal cell. Biochimica et Biophysica Acta 778: 549–558, 1984
Wallmark B, Carlsson E, Larsson H, Brändström A, Lindberg P. New inhibitors of gastric acid secretion: properties and design of H+, K+-ATPase blockers. In press, 1986
Wallmark B, Jaresten B-M, Larsson H, Ryberg B, Brändström A, et al. Differentiation among inhibitory actions of omeprazole, cimetidine, and SCN− on gastric acid secretion. American Journal of Physiology 245: 964–971, 1983
Wallmark B, Lorentzon P, Larsson H. The mechanism of action of omeprazole — a survey of its inhibitory actions in vitro. Scandinavian Journal of Gastroenterology 20(Suppl. 108): 37–52, 1985
Walt RP, Gomes M de FA, Wood EC, Logan LH, Pounder RE. Effect of daily oral omeprazole on 24 hour intragastric acidity. British Medical Journal 287: 12–14, 1983
Walt RP, Reynolds JR, Langman MJS, Smart HL, Kitchingman G, et al. Intravenous omeprazole rapidly raises intragastric pH. Gut 26: 902–906, 1985
Walt RP, Reynolds JR, Langman MJS, Smart HL, Somerville KW, et al. Intravenous omeprazole rapidly raises intragastric pH. Gut 25: A1139, 1984
Webster LK, Jones DB, Mihaly GW, Morgan DJ, Smallwood RA. Effect of hypoxia on the disposition of omeprazole and two metabolites by isolated perfused rat liver. Clinical and Experimental Pharmacology and Physiology (Suppl. 8): 47, 1984a
Webster LK, Jones DB, Mihaly GW, Morgan DJ, Smallwood RA. Effect of hypoxia on oxidative and reductive pathways of omeprazole metabolism by the isolated perfused rat liver. Biochemical Pharmacology 34: 1239–1245, 1985
Webster LK, Jones DB, Mihaly GW, Smallwood RA. Effect of omeprazole and polyethylene glycol-400 on antipyrine elimination by the isolated perfused rat liver. Journal of Pharmacy and Pharmacology 36: 470–472, 1984b
Webster LK, Jones DB, Smallwood RA. How potent is the inhibition of drug metabolism by omeprazole? Lancet 2: 761, 1984c
White JF. Omeprazole inhibits H+ secretion by Amphiuma jejunum. American Journal of Physiology 248: G256–G259, 1985
Wilson JA, Boyd EJS, Wormsley KG. Omeprazole inhibits nocturnal and pentagastrin-stimulated gastric secretion in man. Digestive Diseases and Sciences 29: 797–801, 1984
Wormsley KG. Intragastric bacterial activity and nitrosation before, during, and after treatment with omeprazole. British Medical Journal 289: 1007, 1984a
Wormsley KG. Assessing the safety of drugs for the long-term treatment of peptic ulcers. Gut 25: 1416–1423, 1984b
Wormsley KG. Antisecretory drugs and gastric cancer. British Medical Journal 291: 1504, 1985
Yamamoto O, Okada Y, Okabe S. Effects of a proton pump inhibitor, omeprazole, on gastric secretion and gastric and duodenal ulcers or erosions in rats. Digestive Diseases and Sciences 29: 394–401, 1984
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: W. Beil, Abteilung Allgemeine Pharmakologie, Medizinische Hochschule Hannover, Hannover, W. Germany; T. Berglindh, Center for Ulcer Research and Education, UCLA School of Medicine, Los Angeles, California, USA; J.D. Gardner, Department of Health & Human Services, National Institute of Health, Bethesda, Maryland, USA; C.W. Howden, Department of Materia Medica, Stobhill General Hospital, Glasgow, Scotland; M.J.S. Langman, Department of Therapeutics, University Hospital, Nottingham, England; W. Londong, Medizinische Klinik Innenstadt, University of Munich, Munich, West Germany; D.W. Piper, Royal North Shore Hospital, St Leonards, New South Wales, Australia; R.E. Pounder, Academic Department of Medicine, The Royal Free Hospital, London, England; G. Sachs, Center for Ulcer Research and Education, UCLA School of Medicine, Los Angeles, California, USA; K.-Fr. Sewing, Abteilung Allgemeine Pharmakologie, Medizinische Hochschule Hannover, Hannover, W. Germany; B. Simon, Gastroenterologische Abteilung, Medizinische Universitätsklinik, Heidelberg, W. Germany; A. Walan, Department of Internal Medicine, University Hospital, Linköping, Sweden; R.P. Walt, Department of Therapeutics, University Hospital, Nottingham, England; K.G. Wormsley, Ninewells Hospital, Ninewells, Dundee, Scotland; N.D. Yeomans, Department of Medicine, Austin Hospital, Heidelberg, Victoria, Australia.
‘Losec’, ‘Lozec’, ‘Losek’ (AB Hässle, Astra; not yet commercially available).
Rights and permissions
About this article
Cite this article
Clissold, S.P., Campoli-Richards, D.M. Omeprazole. Drugs 32, 15–47 (1986). https://doi.org/10.2165/00003495-198632010-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-198632010-00002