Summary
Synopsis
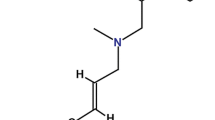
Tioconazole 1 is a substituted imidazole antimicrobial agent structurally related to other drugs in this group. It has been shown to have a broad spectrum of activity in vitro against dermatophytes and yeasts, as well as against some chlamydia, trichomonads and Gram-positive bacteria. Both open and controlled clinical trials have clearly demonstrated the efficacy and safety of topical preparations of tioconazole for treating superficial dermatophyte or yeast infections of the skin and vaginal candidiasis. In comparative studies it was at least as effective as alternative imidazole antifungal drugs, and in a few trials significantly greater efficacy has been reported for tioconazole, compared with clotrimazole, miconazole, econazole and systemic ketoconazole. Preliminary studies in other clinical areas suggest tioconazole may be useful for treating onychomycosis (in a special nail formulation), napkin-rash due to Candida albicans, impetigo, and vaginal trichomoniasis, although comparative studies are needed in each of these settings to clearly assess its relative place in therapy.
Thus, tioconazole is an effective and well tolerated treatment for vaginal candidiasis and superficial fungal infections of the skin.
Pharmacodynamic Studies
In standard in vitro sensitivity tests tioconazole has been shown to have activity against a wide range of fungi (mainly dermatophytes and yeasts), as well as some chlamydia, trichomonads and Gram-positive bacteria. For most organisms tested, minimum inhibitory concentrations of tioconazole were often 2- to 4-fold lower than for miconazole. However, some studies have not shown such marked differences between these 2 drugs. In such studies, variations in experimental conditions (type of media, presence of horse serum, inoculum size, and incubation time) produced unpredictable changes in the in vitro activity of tioconazole and other imidazole antifungal drugs.
Additional comparative studies have demonstrated that tioconazole has considerably greater fungicidal activity than clotrimazole, econazole, ketoconazole, and miconazole against Candida albicans and other Candida species. Tioconazole was also rapidly fungicidal against selected strains of Trichophyton rubrum and Trichophyton mentagrophytes. In vivo animal studies confirmed the activity of tioconazole against experimental candidiasis and experimental dermatophytosis but also showed that it was ineffective against experimental coccidioidomycosis.
The precise mechanism of action of tioconazole has not been conclusively established although, like other imidazole antifungal drugs, it appears to act primarily on cell membrane systems. Recent evidence suggests that it may have 2 modes of action: a fungistatic mechanism at low concentrations which seems to be related to inhibition of the synthesis of ergosterol a cell membrane component, and a fungicidal action at higher concentrations which is due to direct damage of the cell wall. Interestingly, in an in vitro system tioconazole was actively fungicidal against both logarithmic and stationary phase cells of Candida albicans and Candida parapsilosis, in contrast to other imidazoles tested which were inactive against stationary phase organisms.
Pharmacokinetic Studies
Minimal systemic absorption of tioconazole has been demonstrated following the application of 2% vaginal cream, 6% vaginal ointment or a 300mg pessary to women with vaginal candidiasis, 1 or 2% dermal cream to the skin of patients, and 28% nail solution to the forearm skin of volunteers. Animal studies have confirmed minimal systemic exposure after l4C-tioconazole was applied dermally or intravaginally.
Therapeutic Trials
Tioconazole has been studied in relatively large numbers of patients with superficial fungal infections of the skin or vaginal candidiasis and in a smaller number of patients with superficial bacterial infections, onychomycosis or vaginal trichomoniasis.
Open studies in patients with superficial dermatophyte or yeast infections of the skin demonstrated that once or twice daily treatment with topical tioconazole 1% cream resulted in complete (clinical and mycological) cure rates of between 60 and 98% within 2 to 6 weeks. One study showed that once daily administration was as effective as twice daily administration; if this is confirmed in a few additional trials it will be a worthwhile advantage, simplifying dosage regimens. In comparative clinical trials in patients with fungal skin infections tioconazole cream was significantly superior to placebo cream and produced rates of cure equivalent to those of alternative imidazole antifungal drugs. Indeed, some investigators reported trends in favour of tioconazole compared with miconazole dermal cream, and others significantly better cure rates with tioconazole compared with topical clotrimazole. Analysis of response rates according to the type of infecting organism generally did not identify any consistent significant differences between the various imidazole drugs. However, in isolated therapeutic trials tioconazole 1 or 2% cream was more effective against Trichophyton rubrum (than miconazole and clotrimazole), Trichophyton mentagrophytes (than miconazole, econazole, and clotrimazole), Malasse zia furfur (than miconazole and clotrimazole), and Candida albicans (than clotrimazole).
During a multicentre clinical trial tioconazole 1% cream cured 78% of infants with napkin rash primarily caused by Candida albicans and, in addition, also cured 8 of 17 infants with impetigo primarily caused by Staphylococcus aureus. Another unpublished multicentre study showed that a specially formulated 28% nail solution of tioconazole produced some degree of improvement in approximately 70% of patients. The results from these preliminary investigations are encouraging but comparative studies are needed to clearly define the relative place of tioconazole in the treatment of such infections.
Both multiple dose regimens (100mg as 2% cream or 1 vaginal pessary for 3, 6 or 14 consecutive nights) and a single dose regimen (300mg as a single dose of 6% ointment or 1 vaginal pessary) of tioconazole have been used in patients with vaginal candidiasis. Although the various formulations and dosage schedules have not been extensively compared, data from several individual clinical trials, and from an international research programme which pooled data from several trials, provide evidence that they produce comparably high (between 70 and 90%) rates of cure. Persistence of cure rates (4 to 6 weeks after treatment with tioconazole) were also very high (80 to 95%) in women with vaginal candidiasis. Most signs and symptoms of the disease such as pruritus, rash, burning, discharge, and dyspareunia were either completely alleviated by tioconazole, or treatment reduced them from being a severe problem to a minor one. Tioconazole caused no drug-related complications in pregnant women who were followed to term after treatment for candidiasis. In comparative clinical trials intravaginally administered tioconazole was at least as effective as other imidazole antifungal drugs; some studies demonstrated significant advantages compared with clotrimazole vaginal cream, econazole vaginal cream, and systemic ketoconazole. Significantly higher short term cure rates were observed for tioconazole compared with pooled data for various alternative imidazole antifungal agents, in an international clinical research programme which evaluated more than 1000 patients with vaginal candidiasis.
A preliminary study in 20 patients with vaginal trichomoniasis showed that intravaginal tioconazole (5g of 2% cream once nightly for 3 days) was effective in about 80% of patients. Symptoms of the disease were markedly reduced, 12 of 19 patients considered the treatment to be very good, and approximately 80% of the group were microbiologically cured 30 and 60 days after treatment. As encouraging as these results appear, additional comparative studies are essential to clearly define the relative place of tioconazole in the treatment of vaginal trichomoniasis.
Side Effects
Topical preparations of tioconazole have been well tolerated in the majority of patients. The only adverse experiences reported have been local reactions such as redness, burning and itching. In comparative clinical trials the incidence of such effects has generally been of the same order for tioconazole as for other imidazole antifungal drugs. In one comparative study tioconazole 6% vaginal ointment caused markedly fewer side effects than systemically administered ketoconazole.
Dosage and Administration
In dermatomycoses, topical preparations of tioconazole 1% (cream, powder, lotion, and spray solution) should be applied once daily (dermal cream) or twice daily, night and morning, and the duration of treatment should be individualised to take into account the site of infection and the invading pathogen. For the treatment of nail infections a 28% nail solution has been formulated and it should be applied twice daily for prolonged periods, usually of at least 6 months.
In vaginal candidiasis, various formulations of tioconazole are available for application deep into the vagina. The recommended dosage is 100mg (5g of 2% cream or a 100mg vaginal pessary) once nightly for 3 days for the majority of patients. Alternatively, a single dose of tioconazole 300mg (5ml of 6% ointment or a 300mg vaginal pessary) may be administered. This regimen may be repeated 1 week later for the small number of patients who improved with the first dose but did not achieve complete cure.
Similar content being viewed by others
References
Akuse JT. Assessment of the efficacy of tioconazole (Trosyd) 300mg ovules in vaginal candidosis. Current Therapeutic Research 36: 409–413, 1984
Alabi GO.: Clinical trials of tioconazole (Trosyd) in dermatophyte infection in Ibadan, Nigeria. Current Therapeutic Research 37: 254–258, 1985
Ånséhn S, Nilsson L. Direct membrane-damaging effect of ketoconazole and tiaconazole on Candida albicans demonstrated by bioluminescent assay of ATP. Antimicrobial Agents and Chemotherapy 26: 22–25, 1984
Artner J, Fuchs G. Open studies of the efficacy, tolerance, systemic absorption and vaginal persistence following a single application of tioconazole ointment in the treatment of patients with vaginal candidiasis. Gynäkologische Rundschau 23 (Suppl. 1): 12–19, 1983a
Artner J, Fuchs G. Double-blind comparison of the efficacy, tolerance and safety of tioconazole and placebo in patients with vaginal candidiasis and the assessment of systemic absorption. Gynäkologische Rundschau 23 (Suppl. 1): 20–24, 1983b
Beggs WH. The effect of antifungal imidazoles on resting cells of Candida parapsilosis. IRCS Medical Science Library Compendium II: 677–678, 1983
Beggs WH. Fungicidal activity of tioconazole in relation to growth phase of Candida albicans and Candida parapsilosis. Antimicrobial Agents and Chemotherapy 26: 699–701, 1984
Borgers M. Mechanism of action of antifungal drugs, with special reference to the imidazole derivatives. Reviews o8 Infectious Diseases 2: 520–534, 1980
Bowman K, Gurwith D, Gurwith M, Mathes B, Moorer G, et al. Comparative study of tiaconazole (UK-20,349) and clotrimazole in the treatment of vaginal candidiasis. Abstract no. 980. Program and Abstracts of the 23rd Interscience Conference on Antimicrobial Agents and Chemotherapy, Las Vegas, Nevada, 24–26 October, 1983
Carmona O, Pino T, Gonzalez I, Silva H. Evaluation of tioconazole in the treatment of vaginal trichomoniasis. Current Therapeutic Research 38: 474–480, 1985
Clayton YM. Treatment available for mycoses. In Rieth (Ed.) A comprehensive guide to the therapeutic use of Tioconazole, pp. 21–41, Pharma Libri, Chicago, 1983
Clayton YM, Hay RJ, McGibbon DH, Pye RJ. Double blind comparison of the efficacy of tioconazole and miconazole for the treatment of fungal infection of the skin or erythrasma. Clinical and Experimental Dermatology 7: 543–549, 1982
Cohen J. Antifungal chemotherapy. Lancet 2: 532–537, 1982
Cohen J. Open comparison of the efficacy, toleration and safety of tioconazole cream and econazole ovules used in the 3-day treatment of patients with vaginal candidiasis. Gynäkologische Rundschau 23 (Suppl. 1): 25–28, 1983
Davidson EAF, Oates JK. Double-blind comparison of tioconazole and miconazole in patients with vaginal yeast infection. In Nelson & Grassi (Eds) Current Chemotherapy and Infectious Disease, Vol. 11. pp. 968, The American Society for Microbiology, Washington, 1980
Davies AR, Marriott MS. Inhibitory effects of imidazole antifungals on the yeast-mycelial transformation in Candida albicans. Microbios Letters 17: 155–158, 1981
Fredriksson T. Treatment of Dermatomycoses with topical tioconazole and miconazole. Dermatologica 166 (Suppl. 1): 14–19, 1983
Gjønnaess H, Jerve F, Bergen T. Tioconazole 2% cream in vaginal candidosis: systemic absorption and results of three days’ treatment compared to clotrimazole vaginal tablets. Current Therapeutic Research 30: 995–1004, 1981
Grigoriu D, Grigoriu A. Double-blind comparison of the efficacy, toleration and safety of tioconazole base 1% and econazole nitrate 1% creams in the treatment of patients with fungal infections of the skin or erythrasma. Dermatologica 166 (Suppl. 1): 8–13, 1983
Grigoriu A, Grigoriu D, Delacrétaz J. Die genito-glutaeale Candidosis des Kleinkindes. Behandlung mit Trosyd (tioconazol). Mykosen 27: 290–294, 1984
Hay RJ. Superficial and deep mycoses: the extent of the problem. In Levine (Ed.) Ketoconazole in the Management of Fungal Disease, pp. 1–13, ADIS Press, Auckland, 1982
Hay RJ. A medical review of tioconazole and other antifungal imidazoles. In Rieth (Ed.) A comprehensive guide to the therapeutic use of Tioconazole, pp. 43–64, Pharma Libri, Chicago, 1983
Hay RJ, Mackie RM, Clayton YM. Tioconazole nail solution — an open study of its efficacy in onychomycosis. Clinical and Experimental Dermatology 10: 111–115, 1985
Heel RC. Vaginal candidosis. In Levine (Ed.) Ketoconazole in the Management of Fungal Disease, pp. 98–102, ADIS Press, Auckland, 1982
Heel RC, Brogden RN, Carmine A, Speight TM, Avery GS. Ketoconazole: a review of its therapeutic efficacy in superficial and systemic fungal infections. Drugs 23: 1–36, 1982
Heel RC, Brogden RN, Speight TM, Avery GS. Econazole: a review of its antifungal activity and therapeutic efficacy. Drugs 16: 177–201, 1978
Henderson JT, Neilson W, Wilson AB, Jevons S. Tioconazole in the treatment of vaginal candidiasis. Gynäkologische Rundschau 23 (Suppl. 1): 42–60, 1983
Houang ET, Lawrence AG. Systemic absorption and persistence of tioconazole in vaginal fluid after insertion of a single 300 mg tioconazole ovule. Antimicrobial Agents and Chemotherapy 27: 964–965, 1985
Itam IH. Tioconazole in vaginal candiasis: an open evaluation of two formulations in St. Margaret Maternity Hospital, Calabar. Current Therapeutic Research 37: 1048–1053, 1985
Jevons S, Gymer GE, Brammer KW, Cox DA, Leeming MRG. Antifungal activity of tioconazole (UK-20,349), a new imidazole derivative. Antimicrobial Agents and Chemotherapy 15: 597–602, 1979
Johnson EM, Richardon MD, Warnock DW. Effect of imidazole antifungals on the development of germ tubes by strains of Candida albicans. Journal of Antimicrobial Chemotherapy 12: 303–316, 1983
Kashin P, Phyfferoen MC, Gibbs DL. A comparative study of once versus twice daily treatment of superficial dermatophyte and yeast infections with tioconazole (1%) cream. Journal of International Medical Research 13: 85–95, 1985
Khan HM, Ahmed M, Islam N, Ali S. New 1-substituted imidazole — tioconazole — in the treatment of superficial dermal mycoses. Current Therapeutic Research 35: 768–771, 1984
Krohn K, Vinnerberg A. Open comparison of the efficacy, toleration and safety of tioconazole and econazole in the 3-day treatment of vaginal candidiasis. Gynäkologische Rundschau 23 (Suppl. 1): 29–32, 1983
Kuokkanen K. Topical tioconazole in Dermatomycosis. Mykosen 25: 274–280, 1982
Lefler E, Stevens DA. Inhibition and killing of Candida albicans in vitro by five imidazoles in clinical use. Antimicrobial Agents and Chemotherapy 25: 450–454, 1984
Levine HB. Experimental pre-clinical index of anti-fungal activity. 13th International Congress of Chemotherapy, Vienna, Austria, August 28–September 2, 1983
Levine HB, Stevens DA, Cobb JM, Gebhardt AE. Miconazole in coccidioidomycosis. Journal of Infectious Diseases 132: 407–414, 1975
Marriott MS. Inhibition of sterol biosynthesis in Candida albicans by imidazole-containing antifungals. Journal of General Microbiology 117: 253–255, 1980
Marriott MS, Baird JRC, Brammer KW, Faulkner JK, Halliwell G, et al. Tioconazole, a new imidazole-antifungal agent for the treatment of Dermatomycoses. Antifungal and Pharmacologic properties. Dermatologica 116 (Suppl. 1): 1–7, 1983a
Marriott MS, Brammer KW, Faccini J, Faulkner JK, Jevons S, et al. Tioconazole, a new broad-spectrum antifungal agent: preclinical studies related to vaginal candidiasis. Gynäkologische Rundschau 23 (Suppl. 1): 1–11, 1983b
Obasi OE. The treatment of superficial dermatophyte infections with tioconazole in Kaduna, Nigeria. Current Therapeutic Research 37: 1062–1071, 1985
Odds FC. Laboratory evaluation of antifungal agents: a comparative study of five imidazole derivatives of clinical importance. Journal of Antimicrobial Chemotherapy 6: 749–761, 1980
Oittner R. Open comparison of the efficacy, toleration and safety of tioconazole cream used for either 3- or 6-day treatment of patients with vaginal candidiasis. Gynäkologische Rundschau 23 (Suppl. 1): 33–36, 1983
Okafor E, Osunkwo IC, Okoro AN. Tioconazole in dermatophyte infections. Current Therapeutic Research 37: 1054–1057, 1985
O’Neill East M, Henderson JT, Jevons S. Tioconazole in the treatment of fungal infections of the skin. Dermatologica 166 (Suppl. 1): 20–33, 1983
Osinusi BO, Ashiru JO. Tioconazole 6% vaginal ointment as a single dose treatment of vaginal candidiasis. Current Therapeutic Research 37: 1044–1047, 1985
Pye GW, Marriott MS. Inhibition of sterol C14 demethylation by imidazole-containing antifungals. Sabouraudia 20: 325–329, 1982
Robertson WH, Liss RH. Clinical and cytopathological assessment of tioconazole in vulvovaginal Candidiasis. 21st Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, 1981, abstract no. 666, 1981
Rohde-Werner H. Topical tioconazole versus systemic ketoconazole treatment of vaginal candidiasis. Journal of International Medical Research 12: 298–302, 1984
Sawyer PR, Brodgen RN, Pinder RM, Speight TM, Avery GS. Miconazole: a review of its antifungal activity and therapeutic efficacy. Drugs 9: 406–423, 1975a
Sawyer PR, Brogden RN, Pinder RM, Speight TM, Avery GS. Clotrimazole: a review of its antifungal activity and therapeutic efficacy. Drugs 9: 424–447, 1975b
Scott EM, Gorman SP, Wright LR. The effect of imidazoles on germination of arthrospores and microconidia of Trichophyton mentagrophytes. Journal of Antimicrobial Chemotherapy 13: 101–110, 1984
Siegel MR, Ragsdale NN. Antifungal mode of action of imidazole. Pesticide Biochemistry and Physiology 9: 48–56, 1978
Somorin AO. Clinical evaluation of tioconazole in dermatophyte infections. Current Therapeutic Research 37: 1058–1061, 1985
Speller DCE. Antifungal agents. Practitioner 223: 511–515, 1979
Sud IJ, Feingold DS. Heterogeneity of action mechanisms among antimycotic imidazoles. Antimicrobial Agents and Chemotherapy 20: 71–74, 1981a
Sud IJ, Feingold DS. Mechanisms of action of the antimycotic imidazoles. Journal of Investigative Dermatology 76: 438–441, 1981b
Tioconazole Study Group. Controlled comparative study of tioconazole cream for utility against dermatocandidiasis. (Translation from original Japanese.) Western Japan Journal of Dermatology 44: 425–443, 1982a
Tioconazole Study Group. Controlled comparative study of tioconazole cream for utility against tinea pedis and tinea versicolor. (Translation from original Japanese.) Western Japan Journal of Dermatology 44: 444–451, 1982b
van den Bossche H, Willemsems G, Cools W, Lauwers WFJ, Le Jeune L. Biochemical effects of miconazole on fungi. II. Inhibition of ergosterol biosynthesis in Candida albicans. Chemical-Biological Interactions 21: 59–78, 1978
Vander Ploeg DE, DeVillez L. A new topical antifungal drug: Tioconazole. International Journal of Dermatology 23: 681–683, 1984
Yoffe CA, Katz EA. Short term treatment of Trichomonas vaginalis with tioconazole cream, a new antifungal agent. Gynäkologische Rundschau 23 (Suppl. 1): 37–41, 1983
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: S. Ånséhn, Department of Clinical Bacteriology, The Medical School, Linköping, Sweden; W.H. Beggs, General Medical Research, Veterans Administration Medical Center, Minneapolis, Minnesota, USA; Y.M. Clayton, Department of Medical Mycology, The Institute of Dermatology, St John’s Hospital for Diseases of the Skin, London, England; T. Fredriksson, Department of Dermatology, Central Hospital, Västerås, Sweden; D. Grigoriu, Service de Vénaéréo-Dermatologie, Centre-Hospitalier Universitaire Vaudois, Lausanne, Switzerland; K. Kuokkanen, Department of Dermatology, University Central Hospital of Tampere, Tampere, Finland; F.C. Odds, Department of Microbiology, University of Leicester, Leicester, England; A.D. Russell, Welsh School of Pharmacy, University of Wales Institute of Science and Technology, Cardiff, Wales; D.W. Warnock, Department of Microbiology, Bristol Royal Infirmary, Bristol, England.
‘Trosyd’, ‘Gyno-Trosyd’ (Pfizer).
Rights and permissions
About this article
Cite this article
Clissold, S.P., Heel, R.C. Tioconazole. Drugs 31, 29–51 (1986). https://doi.org/10.2165/00003495-198631010-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-198631010-00003