Summary
Synopsis: Probucol1 is a cholesterol-lowering drug without structural similarities to other lipid-lowering agents. It reduces serum cholesterol levels by about 10 to 15% in most patients with hypercholesterolaemia, but does not appear to lower serum triglyceride levels, and thus would seem to be useful primarily in patients with hypercholesterolaemia alone (type Ha hyperlipoproteinaemia). Comparative studies with bile acid-binding resins, which are also useful in type IIa patients, have not been done. Probucol’s effect on the serum concentrations of lipoprotein cholesterol fractions needs to be further clarified in additional studies, but it appears to mainly lower low density lipoprotein cholesterol levels.
In all studies in man reported thus far probucol has been well tolerated, only a few patients discontinuing treatment due to side-effects. It is given in tablet form in a twice daily dose. Its relative ease of administration compared with bile acid-binding resins, if accompanied by equivalent effectiveness, would offer a considerable advantage in a group of patients in whom drug therapy, once begun, is usually continued for a long period; but whether or not probucol is as effective as these agents has not been demonstrated in comparative studies.
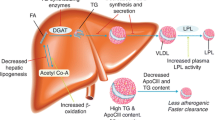
Pharmacodynamic studies: Addition of probucol to the diet of rats and mice reduced serum cholesterol levels without changing liver cholesterol concentrations, unlike clofibrate and colestipol (other lipid-lowering. drugs) which reduced liver cholesterol. In studies in volunteers with high normal or moderately elevated serum cholesterol levels, receiving their regular diet, 375 to 3000mg of probucol daily for 6 weeks lowered serum cholesterol levels by about 30%; although in therapeutic trials (see section 3) the response was usually less. Increasing the dose beyond 750mg daily to 3000mg per day did not produce a significantly greater response in volunteers. Twice daily doses were more effective than a single daily dose. The mechanism of probucol’s cholesterol-lowering activity has not been clearly demonstrated, but some authors have suggested that inhibition of lipoprotein formation and/or impaired intestinal mucosal transport of cholesterol may be involved.
Pharmacokinetic studies: There is little published information on the pharmacokinetic properties of probucol in man. Largely from unpublished information it appears that absorption after oral administration of single doses is limited and variable. During chronic administration plasma levels increase gradually, reaching a steady state after 3 to 4 months of treatment. In animal studies probucol was retained in adipose tissue, the concentration in body fat being 100 times that in the plasma after 2 years of administration to monkeys. In rats and dogs the bile was a major route of elimination of probucol after a single intravenous dose. In man about 80% of a single radioactive dose, administered to patients who had received 1g of probucol daily for 3 weeks, was excreted in the faeces in the first 4 days after administration, but some radioactivity was still detectable in the plasma after 50 days. At 6 weeks and at 6 months after discontinuing probucol in 8 patients who had received 1g of probucol daily for 1 year, plasma levels had decreased by only 60% and 80%, respectively.
Therapeutic trials: Probucol has been studied in a reasonably large number of patients in open trials and in a smaller number of patients in placebo-controlled studies. Like the bile acid-binding resins (cholestyramine, colestipol), probucol appears to be primarily useful in patients with hypercholesterolaemia alone (type IIa hyperlipoproteinaemia), but comparative studies with these agents have not been reported.
In most studies probucol usually lowered serum cholesterol levels by about 10 to 15% (although some patients, especially with severe primary hypercholesterolaemia, have failed to respond), the maximum effect occurring after 1 to 3 months of administration. Serum cholesterol levels have been lowered by about the same extent in patients with hypercholesterolaemia alone and in patients with mixed hypercholesterolaemia and hypertriglyceridaemia. In the best designed controlled trial, probucol reduced serum cholesterol levels 13% more than could be achieved by diet alone in 30 patients with familial (type Ha or IIb) hypercholesterolaemia, while a placebo did not improve the response achieved with a fat-restricted diet alone. Although both high density and low density lipoprotein cholesterol were reduced in this study, the low density fraction accounted for most of the total serum cholesterol decrease. Additional studies are required to further clarify the drug’s effect on serum lipoprotein cholesterol fractions.
There have been variable changes in serum triglyceride levels during probucol administration in therapeutic trials. Thus, triglyceride concentrations have markedly decreased in a few patients with very high (600 to 3000mg/100ml) pretreatment levels, but conversely large increases in triglyceride levels have occasionally occurred (Nash, 1975). In most patients however, there has either been no change, or only a slight increase or decrease.
Side-effects: Although the number of long-term studies is limited, in short term trials and in a smaller number of patients treated for several years probucol has been well tolerated. Only a few patients have discontinued treatment due to side-effects. The most common adverse reaction has been diarrhoea (or loose stools), the reported incidence of which has varied widely in therapeutic trials (from 2 to 30%). Other gastrointestinal symptoms such as flatulence, nausea, and abdominal pain have also been reported. An idiosyncratic reaction characterised by dizziness and palpitations in 1 patient has been observed. 2 studies have reported mild, transient eosinbphilia in 10 to 30% of patients.
Dosage and administration: Like other lipid-lowering drugs, probucol should be used only as a supplement to other appropriate therapeutic rneasures, such as diet and attempted reduction to ideal weight, or treatment of an underlying cause of hypercholesterolaemia to reduce serum cholesterol levels; and only when appropriate dietary regimens alone have been proven inadequate. Although it may lower elevated cholesterol levels in patients with mixed hyperlipidaemia (hypercholesterolaemia with hypertriglyceridaemia), it is not intended for use when hypertriglyceridaemia is the primary concern.
The recommended adult dosage is 500mg twice daily taken with the morning and evening meals. Adequate baseline studies of both serum cholesterol and triglyceride levels should be performed to facilitate periodic monitoring during drug administration. A favourable trend in cholesterol serum levels should occur in the first 2 months of treatment, but subsequent periodic monitoring of cholesterol levels should also be undertaken to determine if the drug remains effective over longer periods. Probucol should be discontinued if a persistent, marked rise in serum triglyceride levels which does not respond to restricted alcohol intake and other appropriate dietary measures occurs.
Similar content being viewed by others
References
Arnold, J.A.; Martin, D.; Taylor, H.L.; Christian, D.R. and Heeg, J.F.: Absorption and excretion studies of the hypocholesterolemic agent 4,4’-(isopropylidenedithio)bis(2,6-di-t-butylphenol) (DH-581) in man. Presented at the Federated Societies of Experimental Biology and Medicine Annual Meeting, Atlantic City, New Jersey (1970)
Barnhart, J.W.; Johnson, J.D.; Rytter, D.J. and Failey, R.B.: The effect of probucol (DH-581) on cholesterol metabolism. Presented at the 4th International Symposium on Drugs Affecting Lipid Metabolism, Philadelphia, USA (1971)
Barnhart, J.W.; Rytter, D.J. and Molello, J.A.: An overview of the biochemical pharmacology of probucol. Lipids 12: 29 (1977)
Barnhart, J.W.; Sefranka, J.A. and Mclntosh, D.D.: Hypocholesterolemic effect of 4,4’-(isopropylidenedithio)-bis(2,6-di-t-butylphenol) (Probucol). American Journal of Clinical Nutrition 23: 1229 (1970)
Brown, H.B. and de Wolfe, V.G.: The additive effect of probucol on diet in hyperlipidemia. Clinical Pharmacology and Therapeutics 16: 44 (1974)
Brusco, O.J.; Bacigaluppi, M.E. and Coppola, LB.: Hypocholesterolemic effect of DH 581 (probucol) — long-term studies. Presented at the 9th International Congress of Nutrition, Mexico, September 3rd–9th (1972)
Brusco, O.J.; Oriozabala, M.A. and Arakaki, R.: Acciondel nuevo hipocolesterolemizante DH-581 (ditiobisfenol) en humanos. La Prensa Medica Argentina 58: 1587 (1971)
Canosa, F. and Boyle, E.: Hypolipidemic effect of addition of either niacin, cholestyramine, or Atromid-S on subjects receiving probucol. Presented at the Annual Meeting of the American Oil Chemists Society, New Orleans, USA, April 21st–24th (1976)
Canosa, F.; Boyle, E. and Aparicio, A.: Long-term hypocholesterolemic drug therapy with probucol (DH-581) in human subjects. Presented at the American Society for Clinical Pharmacology and Therapeutics Meeting, Washington, D.C., March 20–21 (1975)
Also published in abstract form in Clinical Pharmacology and Therapeutics 17: 230 (1975)
Carlson, L.A.; Danielson, M.; Ekberg, I.; Klintemar, B. and Rosenhamer, G.: Reduction of myocardial reinfarction by the combined treatment with clofibrate and nicotinic acid. Atherosclerosis 28: 81 (1977)
Colmore, J.: DH-581: A new cholesterol lowering agent. Presented at the American Society for Clinical Pharmacology and Therapeutics Meetings, Atlantic City, New Jersey, May 3rd (1969)
Danowski, T.S.; Vester, J.W.; Sunder, J.H.; Gonzalez, A.R.; Khurana, R.C. and Jung, Y.: Endocrine and metabolic indices during administration of a lipophilic bis-phenol, probucol. Clinical Pharmacology and Therapeutics 12: 929 (1971)
Davignon, J.: Clofibrate and DH-581 in the long-term treatment of primary hyperlipoproteinemia. Proceedings of the Third International Symposium on Atherosclerosis, West Berlin. Springer-Verlag, Berlin (1974)
Drake, J.W.; Bradford, R.H.; McDearmon, M. and Furman, R.H.: The effect of [4,4’-(isopropylidenedithio)bis(2,6-di-t-butylphenol)] (DH-581) on serum lipids and lipoproteins in human subjects. Metabolism 18: 916 (1969)
Duncan, C.H. and Best, M.M.: The additive effects of clofibrate and probucol (DH-581) on rat serum cholesterol. Atherosclerosis 17: 161 (1973)
Harris, R.S.; Gilmore, H.R.; Bricker, L.A.; Kiem, I.M. and Rubin, E.: Long-term oral administration of probucol [4,4’-(isopropylidenedithio)bis(2,6-di-t-butylphenoO] (DH-581) in the management of hypercholesterolaemia. Journal of the American Geriatrics Society 22: 167 (1974)
Kalams, Z.; Dacquisto, M. and Kornett, G.S.: Biphenabid (probucol): A new hypocholesterolemic agent. Current Therapeutic Research 13: 692(1971)
Kritchevsky, D.: Newer hypolipidemic agents. Federation Proceedings 30: 835 (1971)
Kritchevsky, D.; Kim, H.K. and Tepper, S.A.: Influence of 4,4’-(isopropylidenedithio)bis(2,6-di-t-butylphenol) (DH-581) on experimental atherosclerosis in rabbits. Proceedings of the Society for Experimental Biology and Medicine 136: 1216 (1971)
LeLorier, J.; DuBreuil-Quidoz, S.; Lussier-Cacan, S.; Huang, Y.-S. and Davignon, J.: Diet and probucol in lowering cholesterol concentrations. Archives of Internal Medicine 137: 1429 (1977)
LeLorier, J.; Enjalbert, M.; Quidoz, S.D.; Cancan, S.L. and Davignon, J.: Effect of probucol on clofibrate resistant familial hypercholesterolaemia. Annals of the Royal College of Physicians and Surgeons of Canada, p.35, January (1978)
Levy, R.I. and Rifkind, B.M.: Lipid lowering drugs and hyperlipidaemia. Current Therapeutics 14: 101 (1973)
Marshall, F.N. and Lewis, J.E.: Sensitisation to epinephrine-induced ventricular fibrillation produced by probucol in dogs. Toxicology and Applied Pharmacology 24: 594 (1973)
McCaughan, D.: Effect of probucol in lowering serum cholesterol: A double-blind study. Proceedings of the Third International Symposium on Atherosclerosis, West Berlin. Springer-Verlag, Berlin (1974)
McCaughan, D.: Probucol in the long-term management of hyperlipidemias. Presented at the Annual Meeting of the American Oil Chemists Society, New Orleans, April 21st–24th (1976)
Miettinen, T.A.: Mode of action of a new hypocholesterolaemic drug (DH-581) in familial hypercholesterolaemia. Atherosclerosis 15: 163 (1972)
Miettinen, T.A. and Toivonen, I.: Treatment of severe and mild hypercholesterolaemia with probucol and neomycin. Postgraduate Medical Journal 51 (Suppl. 8): 71 (1975)
Molello, J.A.; Gerbig, C.G. and Robinson, V.B.: Toxicity of [4,4’-(isopropylidenedithio)bis(2,6-di-t-butylphenol)], probucol, in mice, rats, dogs and monkeys: Demonstration of a species-specific phenomenon. Toxicology and Applied Pharmacology 24: 590 (1973)
Nash, D.T.: Probucol, a new cholesterol lowering drug. Journal of Medicine 6: 305 (1975)
Parsons, W.B.: Effect of a new cholesterol-reducing agent (probucol) in hyperlipoproteinemic humans. Circulation 45-46 (Suppl. 2): 16 (1972)
Parsons, W.B.: Effect of probucol in hyperlipidemic patients during two years of administration. American Heart Journal, in press (1978)
Phillips, W.A.; Prange, R.N. and Schultz, J.R.: Effects of colestipol hydrochloride, clofibrate and probucol in normocholesterolemic rats. Presented at the 30th Annual meeting, Council on Arteriosclerosis: American Society for the Study of Arteriosclerosis, November (1976)
Polachek, A.A.; Katz, H.M.; Sack, J.; Selig, J. and Littman, M.L.: Probucol in the long-term treatment of hypercholesterolaemia. Current Medical Research and Opinion 1: 323 (1973)
Salel, A.F.; Zelis, R.; Sodhi, H.S.; Price, J. and Mason, D.T.: Probucol: A new cholesterol-lowering drug effective in patients with type II hyperlipoproteinemia. Clinical Pharmacology and Therapeutics 20: 690 (1976)
Scott, P.J.: Lipid lowering drugs and coronary heart disease. Drugs 10: 218 (1975)
Taylor, H.L.; Nolan, R.B.; Tedeschi, R.E. and Maurath, C.J.: Combined results of the study of probucol at 1 gm/day in eight centers. Clinical Pharmacology and Therapeutics 23: 131 (1978)
Verstraete, M.: Antiplatelet agents in coronary disease: Are they of prophylactic value? Drugs 15: 464 (1978)
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: S.M. Grundy, Veterans Administration Hospital, La Jolla, California, USA; J.B. Hickie, University of New South Wales, Kensington, Australia; R.J. Levy, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Maryland, USA; B. Lewis, St. Thomas’s Hospital Medical School, London, England; P.J. Nestel, Baker Medical Research Institute, Prahran, Australia; M.F. Oliver, Royal Infirmary, Edinburgh, Scotland; A.J. Palmer, Prince Henry Hospital, Little Bay, Australia; P.J. Scott, University of Auckland School of Medicine, Auckland, New Zealand; R. Zelis, Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, Pennsylvania, USA.
‘Lorelco’ (Dow).
Rights and permissions
About this article
Cite this article
Heel, R.C., Brogden, R.N., Speight, T.M. et al. Probucol: A Review of its Pharmacological Properties and Therapeutic Use in Patients with Hypercholesterolaemia. Drugs 15, 409–428 (1978). https://doi.org/10.2165/00003495-197815060-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-197815060-00001