Abstract
Observational studies have documented that women take a variety of medications during pregnancy. It is well known that pregnancy can induce changes in the plasma concentrations of some drugs. The use of mechanistic-based approaches to drug interactions has significantly increased our ability to predict clinically significant drug interactions and improve clinical care. This same method can also be used to improve our understanding regarding the effect of pregnancy on pharmacokinetics of drugs.
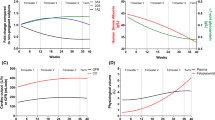
Limited studies suggest bioavailability of drugs is not altered during pregnancy. Increased plasma volume and protein binding changes can alter the apparent volume of distribution (Vd) of drugs. Through changes in Vd and clearance, pregnancy can cause increases or decreases in the terminal elimination half-life of drugs. Depending on whether a drug is excreted unchanged by the kidneys or which metabolic isoenzyme is involved in the metabolism of a drug can determine whether or not a change in dosage is needed during pregnancy. The renal excretion of unchanged drugs is increased during pregnancy. The metabolism of drugs catalysed by select cytochrome P450 (CYP) isoenzymes (i.e. CYP3A4, CYP2D6 and CYP2C9) and uridine diphosphate glucuronosyltransferase (UGT) isoenzymes (i.e. UGT1A4 and UGT2B7) are increased during pregnancy. Dosages of drugs predominantly metabolised by these isoenzymes or excreted by the kidneys unchanged may need to be increased during pregnancy in order to avoid loss of efficacy. In contrast, CYP1A2 and CYP2C19 activity is decreased during pregnancy, suggesting that dosage reductions may be needed to minimise potential toxicity of their substrates.
There are limitations to the available data. This analysis is based primarily on observational studies, many including small numbers of women. For some isoenzymes, the effect of pregnancy on only one drug has been evaluated. The full-time course of pharmacokinetic changes during pregnancy is often not studied. The effect of pregnancy on transport proteins is unknown. Drugs eliminated by non-CYP or non-UGT pathways or multiple pathways will need to be evaluated individually. In conclusion, by evaluating the pharmacokinetic data of a variety of drugs during pregnancy and using a mechanistic-based approach, we can start to predict the effect of pregnancy for a large number of clinically used drugs. However, because of the limitations, more clinical, evidence-based studies are needed to fully elucidate the effects of pregnancy on the pharmacokinetics of drugs.






Similar content being viewed by others
References
Glover DD, Amonkar M, Rybeck BF, et al. Prescription, over-the-counter, and herbal medicine use in a rural, obstetric population. Am J Obstet Gynecol 2003; 188: 1039–45
Bodendorfer TW, Briggs GG, Gunning JE. Obtaining drug exposure histories during pregnancy. Am J Obstet Gynecol 1979; 135: 490–4
Andrade SE, Gurwitz JH, Davis RL, et al. Prescription drug use in pregnancy. Am J Obstet Gynecol 2004; 191: 398–407
Anderson G. A mechanistic approach to antiepileptic drug interactions. Ann Pharmacoth 1998; 32: 554–63
Yan Z, Caldwell GW. Metabolism profiling, and cytochrome P450 inhibition and induction in drug discovery. Curr Top Med Chem 2001; 1: 403–25
Yao C, Levy RH. Inhibition-based metabolic drug-drug interactions: predictions from in vitro data. J Pharm Sci 2002; 91: 1923–35
Ito K, Brown HS, Houston JB. Database analyses for the prediction of in vivo drug-drug interactions from in vitro data. Br J Clin Pharmacol 2004; 57: 473–86
Mirochnick M, Capparelli E. Pharmacokinetics of antiretrovirals in pregnant women. Clin Pharmacokinet 2004; 43: 1071–87
Loebstein R, Lalkin A, Koren G. Pharmacokinetic changes during pregnancy and their clinical relevance. Clin Pharmacokinet 1997; 33: 328–43
Little BB. Pharmacokinetics during pregnancy: evidence-based maternal dose formulation. Obstet Gynecol 1999; 93: 858–68
Loebstein R, Koren G. Clinical relevance of therapeutic drug monitoring during pregnancy. Ther Drug Monit 2002; 24: 15–22
Mitani GM, Steinberg I, Lien EJ, et al. The pharmacokinetics of antiarrhythmic agents in pregnancy and lactation. Clin Pharmacokinet 1987; 12: 253–91
Pennell PB. Antiepileptic drug pharmacokinetics during pregnancy and lactation. Neurology 2003; 61: S35–42
Philipson A. Pharmacokinetics of antibiotics in pregnancy and labour. Clin Pharmacokinet 1979; 4: 297–309
Yerby MS, Friel PN, McCormick K. Antiepileptic drug disposition during pregnancy. Neurology 1992; 42 Suppl. 5: 12–6
O’Hare MF, Leahey W, Murnaghan GA, et al. Pharmacokinetics of sotalol during pregnancy. Eur J Clin Pharmacol 1983; 24: 521–4
Philipson A. Pharmacokinetics of ampicillin during pregnancy. J Infect Dis 1977; 136: 370–6
Philipson A, Stiernstedt G, Ehrnebo M. Comparison of the pharmacokinetics of cephradine and cefazolin in pregnant and non-pregnant women. Clin Pharmacokinet 1987; 12: 136–44
Knutti R, Rothweiler H, Schlatter C. Effect of pregnancy on the pharmacokinetics of caffeine. Eur J Clin Pharmacol 1981; 21: 121–6
Aldridge A, Bailey J, Neims AH. The disposition of caffeine during and after pregnancy. Semin Perinatol 1981; 5: 310–4
Bologa M, Tang B, Klein J, et al. Pregnancy-induced changes in drug metabolism in epileptic women. J Pharmacol Exp Ther 1991; 257: 735–40
Tsutsumi K, Kotegawa T, Matsuki S, et al. The effect of pregnancy on cytochrome P4501A2, xanthine oxidase, and N-acetyltransferase activities in humans. Clin Pharmacol Ther 2001; 70: 121–5
Wadelius M, Darj E, Frenne G, et al. Induction of CYP2D6 in pregnancy. Clin Pharmacol Ther 1997; 62: 400–7
Hogstedt S, Lindberg B, Rane A. Increased oral clearance of metoprolol in pregnancy. Eur J Clin Pharmacol 1983; 24: 217–20
Hogstedt S, Lindberg B, Peng DR, et al. Pregnancy-induced increase in metoprolol metabolism. Clin Pharmacol Ther 1985; 37: 688–92
Heikkinen T, Ekblad U, Palo P, et al. Pharmacokinetics of fluoxetine and norfluoxetine in pregnancy and lactation. Clin Pharmacol Ther 2003; 73: 330–7
Wisner KL, Perel JM, Wheeler SB. Tricyclic dose requirements across pregnancy. Am J Psychiatry 1993; 150: 1541–2
Ohkita C, Goto M. Increased 6-hydroxycortisol excretion in pregnant women: implication of drug-metabolizing enzyme induction. DICP 1990; 24: 814–6
Kosel BW, Beckerman KP, Hayashi S, et al. Pharmacokinetics of nelfinavir and indinavir in HIV-1-infected pregnant women. AIDS 2003; 17: 1195–9
Prevost RR, Akl SA, Whybrew WD, et al. Oral nifedipine pharmacokinetics in pregnancy-induced hypertension. Pharmacotherapy 1992; 12: 174–7
Tomson T, Lindbom U, Ekqvist B, et al. Epilepsy and pregnancy: a prospective study of seizure control in relation to free and total plasma concentrations of carbamazepine and phenytoin. Epilepsia 1994; 35: 122–30
Tomson T, Lindbom U, Ekqvist B, et al. Disposition of carbamazepine and phenytoin in pregnancy. Epilepsia 1994; 35: 131–5
Yerby MS, Friel PN, McCormick K, et al. Pharmacokinetics of anticonvulsants in pregnancy: alternations in plasma protein binding. Epilepsy Res 1990; 5: 223–8
Wilson CM, Dundee JW, Moore J, et al. A comparison of the early pharmacokinetics of midazolam in pregnant and non-pregnant women. Anaesthesia 1987; 42: 1057–62
Acosta EP, Zorrilla C, Van Dyke R, et al. Pharmacokinetics of saquinavir-SGC in HIV-infected pregnant women. HIV Clin Trials 2001; 2: 460–5
Acosta EP, Bardeguez A, Zorrilla CD, et al. Pharmacokinetics of saquinavir plus low-dose ritonavir in human immunodeficiency virus-infected pregnant women. Antimicrob Agents Chemother 2004; 48: 430–6
Stek A, Mirochnick M, Capparelli E, et al. Reduced lopinavir exposure during pregnancy: preliminary pharmacokinetic results from PACTG 1026 [abstract no. LbOrB08]. XV International Aids Conference; 2004 Jul 11–18; Bangkok. Epub eJIAS 2004 Jul 11; 1 (1)
Pennell PB, Newport DJ, Stowe ZN, et al. The impact of pregnancy and childbirth on the metabolism of lamotrigine. Neurology 2004; 62: 292–5
de Haan GJ, Edelbroek P, Segers J, et al. Gestation-induced changes in lamotrigine pharmacokinetics: a monotherapy study. Neurology 2004; 63: 571–3
Tran TA, Leppik IE, Blesi K, et al. Lamotrigine clearance during pregnancy. Neurology 2002; 59: 251–5
Ohman I, Vitols S, Tomson T. Lamotrigine in pregnancy: pharmacokinetics during delivery, in the neonate and during lactation. Epilepsia 2000; 41: 709–13
Watts DH, Brown ZA, Tartaglione T, et al. Pharmacokinetic disposition of zidovudine during pregnancy. J Infect Dis 1991; 163: 226–32
O’sullivan MJ, Boyer PJ, Scott GB, et al. The pharmacokinetics and safety of zidovudine in the third trimester of pregnancy for women infected with human immunodeficiency virus and their infants: phase I acquired immunodeficiency syndrome clinical trials group study (protocol 082). Zidovudine Collaborative Working Group. Am J Obstet Gynecol 1993; 168: 1510–6
Gerdin E, Salmonson T, Lindberg B, et al. Maternal kinetics of morphine during labour. J Perinat Med 1990; 18: 479–87
Tomson G, Lunell NO, Sundwall A, et al. Placental passage of oxazepam and its metabolism in mother and newborn. Clin Pharmacol Ther 1979; 25: 74–81
Chamberlain A, White S, Bawdon R, et al. Pharmacokinetics of ampicillin and sulbactam in pregnancy. Am J Obstet Gynecol 1993; 168: 667–73
Assael BM, Como ML, Miraglia M, et al. Ampicillin kinetics in pregnancy. Br J Clin Pharmacol 1979; 8: 286–8
Philipson A, Stiernstedt G. Pharmacokinetics of cefuroxime in pregnancy. Am J Obstet Gynecol 1982; 142: 823–8
Nathorst-Boos J, Philipson A, Hedman A, et al. Renal elimination of ceftazidime during pregnancy. Am J Obstet Gynecol 1995; 172: 163–6
Heikkila A, Erkkola R. Pharmacokinetics of piperacillin during pregnancy. J Antimicrob Chemother 1991; 28: 419–23
Heikkila A, Pyykko K, Erkkola R, et al. The pharmacokinetics of mecillinam and pivmecillinam in pregnant and non-pregnant women. Br J Clin Pharmacol 1992; 33: 629–33
Hurst AK, Shotan A, Hoffman K, et al. Pharmacokinetic and pharmacodynamic evaluation of atenolol during and after pregnancy. Pharmacotherapy 1998; 18: 840–6
Thorley KJ, McAinsh J, Cruickshank JM. Atenolol in the treatment of pregnancy-induced hypertension. Br J Clin Pharmacol 1981; 12: 725–30
Hebert MF, Carr DB, Anderson GD, et al. Pharmacokinetics and pharmacodynamics of atenolol during pregnancy and postpartum. J Clin Pharmacol 2005; 45: 25–33
Luxford AM, Kellaway GS. Pharmacokinetics of digoxin in pregnancy. Eur J Clin Pharmacol 1983; 25: 117–21
Schou M, Amdisen A, Steenstrup OR. Lithium and pregnancy: II. Hazards to women given lithium during pregnancy and delivery. BMJ 1973; 2: 137–8
Ensom MH, Stephenson MD. Pharmacokinetics of low molecular weight heparin and unfractionated heparin in pregnancy. J Soc Gynecol Investig 2004; 11: 377–83
Blomback M, Bremme K, Hellgren M, et al. A pharmacokinetic study of dalteparin (Fragmin) during late pregnancy. Blood Coagul Fibrinolysis 1998; 9: 343–50
Casele HL, Laifer SA, Woelkers DA, et al. Changes in the pharmacokinetics of the low-molecular-weight heparin enoxaparin sodium during pregnancy. Am J Obstet Gynecol 1999; 181: 1113–7
Dean M, Stock B, Patterson RJ, et al. Serum protein binding of drugs during and after pregnancy in humans. Clin Pharmacol Ther 1980; 28: 253–61
Benet LZ, Hoener BA. Changes in plasma protein binding have little clinical relevance. Clin Pharmacol Ther 2002; 71: 115–21
Vajda FJ, O’Brien TJ, Hitchcock A, et al. The Australian registry of anti-epileptic drugs in pregnancy: experience after 30 months. J Clin Neurosci 2003; 10: 543–9
Kaneko S, Kondo T. Antiepileptic agents and birth defects: incidence, mechanisms and prevention. CNS Drugs 1995; 3: 41–55
Morgan DJ, Smallwood RA. Clinical significance of pharmacokinetic models of hepatic elimination. Clin Pharmacokinet 1990; 18: 61–76
Wrighton SA, Stevens JC. The human hepatic cytochrome P450 involved in drug metabolism. Crit Rev Toxicol 1992; 22: 1–21
Fisher MB, Paine MF, Strelevitz TJ. The role of hepatic and extrahepatic UDP-glucuronosyltransferases in human drug metabolism. Drug Metab Rev 2001; 33: 273–97
Mackenzie PI, Owens IS, Burchell B, et al. The UDP glucuronosyltransferase gene superfamily: recommended nomenclature update based on evolutionary divergence. Pharmacogenetics 1997; 7: 255–9
Burchell B, Brierley CH, Rance D. Specificity of human UDP-glucuronosyltransferases and xenobiotic glucuronidation. Life Sci 1995; 57: 1819–31
Kalow W, Tang BK. Caffeine as a metabolic probe: exploration of the enzyme-inducing effect of cigarette smoking. Clin Pharmacol Ther 1991; 49: 44–8
Han XM, Ou-Yang DS, Lu PX, et al. Plasma caffeine metabolite ratio (17X/137X) in vivo associated with G-2964A and C734A polymorphisms of human CYP1A2. Pharmacogenetics 2001; 11: 429–35
Nordmark A, Lundgren S, Ask B, et al. The effect of the CYP1A2 *1F mutation on CYP1A2 inducibility in pregnant women. Br J Clin Pharmacol 2002; 54: 504–10
Sachse C, Bhambra U, Smith G, et al. Polymorphisms in the cytochrome P450 CYP1A2 gene (CYP1A2) in colorectal cancer patients and controls: allele frequencies, linkage disequilibrium and influence on caffeine metabolism. Br J Clin Pharmacol 2003; 55: 68–76
Miners JO, McKinnon RA. CYP1A. In: Levy RH, Thummel KE, Trager WF, et al., editors. Metabolic drug interactions. Philadelphia (PA): Lippincott Williams & Wilkins, 2000: 61–73
Gardner MJ, Schatz M, Cousins L, et al. Longitudinal effects of pregnancy on the pharmacokinetics of theophylline. Eur J Clin Pharmacol 1987; 32: 289–95
Sutton PL, Rose JQ, Goldstein S, et al. Theophylline pharmacokinetics during pregnancy and post partum [abstract]. J Allergy Clin Immunol 1980; 65: 117
Messina ES, Tyndale RF, Sellers EM. A major role for CYP2A6 in nicotine C-oxidation by human liver microsomes. J Pharmacol Exp Ther 1997; 282: 1608–14
Dempsey D, Tutka P, Jacob III P, et al. Nicotine metabolite ratio as an index of cytochrome P450 2A6 metabolic activity. Clin Pharmacol Ther 2004; 76: 64–72
Dempsey D, Jacob III P, Benowitz NL. Accelerated metabolism of nicotine and cotinine in pregnant smokers. J Pharmacol Exp Ther 2002; 301: 594–8
Oscarson M. Genetic polymorphisms in the cytochrome P450 2A6 (CYP2A6) gene: implications for interindividual differences in nicotine metabolism. Drug Metab Dispos 2001; 29: 91–5
Bajpai M, Roskos LK, Shen DD, et al. Roles of cytochrome P4502C9 and cytochrome P4502C19 in the stereoselective metabolism of phenytoin to its major metabolites. Drug Metab Dispos 1996; 24: 1401–3
Mamiya K, Ieiri I, Shimamoto J, et al. The effects of genetic polymorphisms of CYP2C9 and CYP2C19 on phenytoin metabolism in Japanese adult patients with epilepsy: studies in stereoselective hydroxylation and population pharmacokinetics. Epilepsia 1998; 39: 1317–23
Dansky L, Andermann E, Sherwin A, et al. Plasma levels of phenytoin during pregnancy and the puerperium. In: Janz D, Dam M, Richens A, et al., editors. Epilepsy, pregnancy, and the child. New York: Raven Press, 1982: 155–62
Bardy AH, Hiilesmaa VK, Teramo KA. Serum phenytoin during pregnancy, labor and puerperium. Acta Neurol Scand 1987; 75: 374–5
Bardy AH, Teramo KA, Hiilesmaa VK. Apparent plasma clearance of phenytoin, phenobarbitone, primidone, and carbamazepine during pregnancy: results of the prospective Helsinki study. In: Janz D, Dam M, Richens A, et al., editors. Epilepsy, pregnancy, and the child. New York: Raven Press, 1982: 141–5
Chen SS, Perucca E, Lee JN, et al. Serum protein binding and free concentration of phenytoin and phenobarbitone in pregnancy. Br J Clin Pharmacol 1982; 13: 547–52
Levy RH. Cytochrome P450 isozymes and antiepileptic drug interactions. Epilepsia 1995; 36 Suppl. 5: S8–13
Helsby NA, Ward SA, Edwards G, et al. The pharmacokinetics and activation of proguanil in man: consequences of variability in drug metabolism. Br J Clin Pharmacol 1990; 30: 593–8
Helsby NA, Ward SA, Howells RE, et al. In vitro metabolism of the biguanide antimalarials in human liver microsomes: evidence for a role of the mephenytoin hydroxylase (P450 MP) enzyme. Br J Clin Pharmacol 1990; 30: 287–91
McGready R, Stepniewska K, Seaton E, et al. Pregnancy and use of oral contraceptives reduces the biotransformation of proguanil to cycloguanil. Eur J Clin Pharmacol 2003; 59: 553–7
Ward SA, Helsby NA, Skjelbo E, et al. The activation of the biguanide antimalarial proguanil co-segregates with the mephenytoin oxidation polymorphism: a panel study. Br J Clin Pharmacol 1991; 31: 689–92
McGready R, Stepniewska K, Edstein MD, et al. The pharmacokinetics of atovaquone and proguanil in pregnant women with acute falciparum malaria. Eur J Clin Pharmacol 2003; 59: 545–52
Cascorbi I. Pharmacogenetics of cytochrome P4502D6: genetic background and clinical implication. Eur J Clin Invest 2003; 33 Suppl. 2: 17–22
Shimada T, Yamazaki H, Mimura M, et al. Interindividual variation in human liver cytochrome P450 enzymes involved in the oxidation of drugs, carcinogens, and toxic chemicals: studies with the microsomes of 30 Japanese and 30 Caucasians. J Pharmacol Exp Ther 1994; 270: 414–23
Mathias AA, Unadkat JD. The role of CYP3A in accelerated oral clearance of anti-HIV drugs during pregnancy [abstract]. Drug Metab Rev 2004; 36 Suppl. 1: 143
Green MD, Bishop WP, Tephley TR. Expressed human UGT1.4 protein catalyzes the formation of quaternary ammonium-linked glucuronides. Drug Metab Dispos 1995; 23: 299–302
Barbier O, Turgeon D, Girard C, et al. 3′-azido-3′-deoxythimidine (AZT) is glucuronidated by human UDP-glucuronosyltransferase 2B7 (UGT2B7). Drug Metab Dispos 2000; 28: 497–502
Coffman BL, Rios GR, King CD, et al. Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab Dispos 1997; 25: 1–4
Sperling RS, Roboz J, Dische R, et al. Zidovudine pharmacokinetics during pregnancy. Am J Perinatol 1992; 9: 247–9
Court MH, Duan SX, Guillemette C, et al. Stereoselective conjugation of oxazepam by human UDP-glucuronosyltransferases (UGTs): S-oxazepam is glucuronidated by UGT2B15, while R-oxazepam is glucuronidated by UGT2B7 and UGT1A9. Drug Metab Dispos 2002; 30: 1257–65
Greenblatt DJ, Divoll M, Harmatz JS, et al. Oxazepam kinetics: effect of age and sex. J Pharmacol Exp Ther 1980; 215: 86–91
Tang BK, Kadar D, Qian L, et al. Caffeine as a metabolic probe: validation of its use for acetylator phenotyping. Clin Pharmacol Ther 1991; 49: 648–57
Handschin C, Meyer UA. Induction of drug metabolism: the role of nuclear receptors. Pharmacol Rev 2003; 55: 649–73
Wang H, LeCluyse EL. Role of orphan nuclear receptors in the regulation of drug-metabolising enzymes. Clin Pharmacokinet 2003; 42: 1331–57
Mackenzie PI, Gregory PA, Gardner-Stephen DA, et al. Regulation of UDP glucuronosyltransferase genes. Curr Drug Metab 2003; 4: 249–57
Dickins M. Induction of cytochromes P450. Curr Top Med Chem 2004; 4: 1745–66
Masuyama H, Hiramatsu Y, Mizutani Y, et al. The expression of pregnane X receptor and its target gene, cytochrome P450 3A1, in perinatal mouse. Mol Cell Endocrinol 2001; 172: 47–56
Madan A, Graham RA, Carroll KM, et al. Effects of prototypical microsomal enzyme inducers on cytochrome P450 expression in cultured human hepatocytes. Drug Metab Dispos 2003; 31: 421–31
Laine K, Tybring G, Bertilsson L. No sex-related differences but significant inhibition by oral contraceptives of CYP2C19 activity as measured by the probe drugs mephenytoin and omeprazole in healthy Swedish white subjects. Clin Pharmacol Ther 2000; 68: 151–9
Palovaara S, Tybring G, Laine K. The effect of ethinyloestradiol and levonorgestrel on the CYP2C19-mediated metabolism of omeprazole in healthy female subjects. Br J Clin Pharmacol 2003; 56: 232–7
Tamminga WJ, Wemer J, Oosterhuis B, et al. CYP2D6 and CYP2C19 activity in a large population of Dutch healthy volunteers: indications for oral contraceptive-related gender differences. Eur J Clin Pharmacol 1999; 55: 177–84
McCune JS, Lindley C, Decker JL, et al. Lack of gender differences and large intrasubject variability in cytochrome P450 activity measured by phenotyping with dextromethorphan. J Clin Pharmacol 2001; 41: 723–31
Sabers A, Ohman I, Christensen J, et al. Oral contraceptives reduce lamotrigine plasma levels. Neurology 2003; 61: 570–1
Abernethy DR, Greenblatt DJ, Ochs HR, et al. Lorazepam and oxazepam kinetics in women on low-dose oral contraceptives. Clin Pharmacol Ther 1983; 33: 628–32
Stoehr GP, Kroboth PD, Juhl RP, et al. Effect of oral contraceptives on triazolam, temazepam, alprazolam, and lorazepam kinetics. Clin Pharmacol Ther 1984; 36: 683–90
Miners JO, Attwood J, Birkett DJ. Influence of sex and oral contraceptive steroids on paracetamol metabolism. Br J Clin Pharmacol 1983; 16: 503–9
Balogh A, Klinger G, Henschel L, et al. Influence of ethinylestradiol-containing combination oral contraceptives with gestodene or levonorgestrel on caffeine elimination. Eur J Clin Pharmacol 1995; 48: 161–6
Pollock BG, Wylie M, Stack JA, et al. Inhibition of caffeine metabolism by estrogen replacement therapy in post-menopausal women. J Clin Pharmacol 1999; 39: 936–40
Gabbay V, O’Dowd MA, Mamamtavrishvili M, et al. Clozapine and oral contraceptives: a possible drug interaction. J Clin Psychopharmacol 2002; 22: 621–2
Tornatore KM, Kanarkowski R, McCarthy TL, et al. Effect of chronic oral contraceptive steroids on theophylline disposition. Eur J Clin Pharmacol 1982; 23: 129–34
Stevens JC, Hines RN, Gu C, et al. Developmental expression of the major human hepatic CYP3A enzymes. J Pharmacol Exp Ther 2003; 307: 573–82
Koukouritaki SB, Manro JR, Marsh SA, et al. Developmental expression of human hepatic CYP2C9 and CYP2C19. J Pharmacol Exp Ther 2004; 308: 965–74
Syme MR, Paxton JW, Keelan JA. Drug transfer and metabolism by the human placenta. Clin Pharmacokinet 2004; 43: 487–514
Hakkola J, Pasanen M, Hukkanen J, et al. Expression of xenobiotic-metabolizing cytochrome P450 forms in human full-term placenta. Biochem Pharmacol 1996; 51: 403–11
Hakkola J, Raunio H, Purkunen R, et al. Detection of cytochrome P450 gene expression in human placenta in first trimester of pregnancy. Biochem Pharmacol 1996; 52: 379–83
Collier AC, Ganley NA, Tingle MD, et al. UDP-glucuronosyl-transferase activity, expression and cellular localization in human placenta at term. Biochem Pharmacol 2002; 63: 409–19
Nakai A, Sekiya I, Oya A, et al. Assessment of the hepatic arterial and portal venous blood flows during pregnancy with Doppler ultrasonography. Arch Gynecol Obstet 2002; 266: 25–9
Robson SC, Mutch E, Boys RJ, et al. Apparent liver blood flow during pregnancy: a serial study using indocyanine green clearance. Br J Obstet Gynaecol 1990; 97: 720–4
Davison JM, Dunlop W. Renal hemodynamics and tubular function normal human pregnancy. Kidney Int 1980; 18: 152–61
Dunlop W. Serial changes in renal haemodynamics during normal human pregnancy. Br J Obstet Gynaecol 1981; 88: 1–9
Davison JM, Dunlop W, Ezimokhai M. 24-hour creatinine clearance during the third trimester of normal pregnancy. Br J Obstet Gynaecol 1980; 87: 106–9
Inui KI, Masuda S, Saito H. Cellular and molecular aspects of drug transport in the kidney. Kidney Int 2000; 58: 944–58
Koren G, Farine D, Maresky D, et al. Significance of the endogenous digoxin-like substance in infants and mothers. Clin Pharmacol Ther 1984; 36: 759–64
Rotmensch HH, Rotmensch S, Elkayam U. Management of cardiac arrhythmias during pregnancy: current concepts. Drugs 1987; 33: 623–33
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The author has no conflicts of interest directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderson, G.D. Pregnancy-Induced Changes in Pharmacokinetics. Clin Pharmacokinet 44, 989–1008 (2005). https://doi.org/10.2165/00003088-200544100-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200544100-00001