Abstract
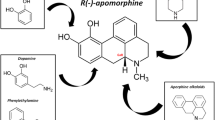
In the treatment of patients with Parkinson’s disease, apomorphine has an established place as a back-up therapy if other antiparkinsonian drugs, such as levodopa and oral dopamine agonists, have not controlled the existing response fluctuations. Apomorphine is a synthetic derivative of morphine, with a totally distinct pharmacological profile. It is a very lipophilic compound which is easily (auto)oxidised. This (auto)oxidation is the main metabolic route besides glucuronidation and sulphation, which are both responsible for about 10% of the metabolic transformation.
Apomorphine quickly passes the nasal and intestinal mucosa as well as the blood-brain barrier (depending on the administration route). Many routes of administration have been explored, but subcutaneous, sublingual, nasal and rectal administration are used in clinical practice. The volume of distribution varies between 1 and 2 times bodyweight. The elimination half-life is very short (30 to 90 min) depending on the type of parenteral administration. Apomorphine is a high clearance drug (3 to 5 L/kg/h) and is mainly excreted and metabolised by the liver. Only 3 to 4% is excreted unchanged in the urine.
The clinical effect of apomorphine can be linked directly to its concentration in the cerebrospinal fluid. Consequently, a 2-compartment model can be used to predict the clinical effects of apomorphine. The pharmacokinetic-pharmacodynamic data reflect the clinical observations of steep dose-effect curves if apomorphine is used in patients with random ‘on-off’ fluctuations. These dose-effect curves are less steep in stable or ‘wearing-off’ (end-of-dose deterioration) patients.
Intravenous infusions of apomorphine in combination with timed motor assessments can be used clinically to characterise the therapeutic window of a particular patient if dyskinesia persists after single injections of apomorphine. If more population data become available, the population pharmacokinetics-pharmacodynamics of apomorphine could be helpful in predicting the clinical effects of apomorphine in the several subgroups of patients with Parkinson’s disease.
Similar content being viewed by others
References
Parkinson J. An essay on the shaking palsy. London: Whittingham and Rowland, 1817.
Weil E. De L’apomorphine dans certain troubles nerveux. Lyon Med 1884; 48: 411–9.
Ernst AM. Relation between action of dopamine and apomorphine and the O-methylated derivatives upon the CNS. Psychopharmacologia 1965; 7: 391–9.
Wachtel H. Antiparkinsonian dopamine agonists: a review of the pharmacokinetics and neuropharmacology in animals and humans. J Neural Transm 1991; 3: 151–201.
Cotzias GC, Papavasiliou PS, Tolosa ES, et al. Treatment of Parkinson’s disease with apomorphines. N Engl J Med 1976; 294: 567–72.
Agid Y, Bonnet AM, Pollak P, et al. Bromocriptine associated with a peripheral dopamine blocking agent in treatment of Parkinson’s disease. Lancet 1979; I: 570–2.
Stibe CMH, Lees AJ, Kempster PA, et al. Subcutaneous apomorphine in parkinsonian on-off oscillations. Lancet 1988; I: 403–6.
Lundgren P, Landersjo L. Stability and stabilization of apomorphine hydrochloride in aqueous solution. Acta Pharm Suec 1970; 7: 133–48.
van Laar T, Jansen ENH, Essink AWG, et al. Intranasal apomorphine in parkinsonian on-off fluctuations. Arch Neurol 1992; 49: 482–4.
van Laar T, Jansen ENH, Neef C, et al. Pharmacokinetics and clinical efficacy of rectal apomorphine in patients with Parkinson’s disease: a study of five different suppositories. Mov Disord 1995; 10 (4): 433–9.
van Laar T, Neef C, Danhof M, et al. A new sublingual formulation of apomorphine in the treatment of patients with Parkinson’s disease. Mov Disord 1996; 11 (6): 633–8.
Gancher ST, Nutt JG, Woodward WR. Absorption of apomorphine by various routes in parkinsonism. Mov Disord 1991; 6: 212–6.
Priston MJ, Sewell GJ. Novel liquid Chromatographic assay for the low-level determination of apomorphine in plasma. J Chromatogr B 1996; 681: 161–7.
Essink AWG, Lohuis CPGG, Klein Elhorst JT, et al. Selective and quantitative isolation and determination of apomorphine in human plasma. J Chromatogr B 1991; 570: 419–24.
Van der Geest R, Kruger P, Gubbens-Stibbe JM, et al. Assay of R-apomorphine, S-apomorphine, apocodeine, isoapocodeine and their glucuronide and sulphate conjugates in plasma and urine of patients with Parkinson’s disease. J Chromatogr B 1997; 702: 131–41.
Kaul PN, Brochman-Hanssen E, Way EL. Biological disposition of apomorphine. Urinary excretion and organ distribution of apomorphine. J Pharm Sci 1961; 50: 244–7.
Kaul PN, Conway MW. Induction and inhibition of in vivo glucuronidation of apomorphine in mice. J Pharm Sci 1971; 60: 93–5.
Missala K, Lal S, Sourkes TL. O-methylation of apomorphine and the metabolic prolongation of apomorphine-induced stereotyped behaviour. Eur J Pharmacol 1973; 22: 54–8.
Burkman AM. Some kinetic and thermodynamic characteristics of apomorphine degra dation. J Pharm Sci 1965; 54: 325–6.
Priston MJ, Sewell GJ. The analysis of apomorphine formulations for ambulatory infusions. Pharm Sci 1995; 1: 91–4.
Goldman ME, Kebabian JW. Aporphine enantiomers: interactions with D1 and D2 dopamine receptors. Mol Pharmacol 1984; 25: 18–23.
Van der Geest R, Van Laar T, Kruger PP, et al. Pharmacokinetics, enantiomer interconversion and metabolism of R-apomorphine in patients with idiopathic Parkinson’s disease. Clin Neuropharmacol 1998; 21: 159–68.
Danhof M, Mandema JW, Stijnen AM. Pharmacokinetic complexities of in vivo pharmacodynamic investigations. In: van Boxtel CJ, Holford NHG, Danhof M, editors. The in vivo study of drug action — concepts and applications of kineticdynamic modeling. Amsterdam: Elsevier Science Publishers, 1992: 31–60.
Przedborski S, Levivier M, Raftopoulos C, et al. Peripheral and central pharmacokinetics of apomorphine and its effect on dopamine metabolism in humans. Mov Disord 1995; 10: 28–36.
Gancher ST, Woodward WR, Gliessman P, et al. The short-duration response to apomorphine: implications for the mechanism of dopaminergic effects in parkinsonism. Ann Neurol 1990; 17: 45–52.
Hofstee DJ, Neef C, van Laar T, et al. Pharmacokinetics of apomorphine in Parkinson’s disease: plasma and cerebrospinal fluid levels in relation to motor responses. Clin Neuropharmacol 1994; 17: 45–52.
Dewey RB, Maraganore DM, Ahlskog JE, et al. A double-blind placebo-controlled study of intranasal apomorphine spray as a rescue agent for off-states in Parkinson’s disease. Mov Disord 1998; 13: 782–7.
Lees AJ, Montastruc JL, Turjanski N, et al. Sublingual apomorphine in Parkinson’s disease [comments]. J Neurol Neurosurg Psychiatry 1989; 51: 1440.
Gancher ST, Woodward WR, Boucher B, et al. Peripheral pharmacokinetics of apomorphine in humans. Ann Neurol 1989; 26: 232–8.
Gancher GT, Nutt JG, Woodward WR. Time course of tolerance to apomorphine in parkinsonism. Clin Pharmacol Ther 1992; 52: 504–10.
Nicolle E, Pollak P, Serre-Debeauvais F, et al. Pharmacokinetics of apomorphine in parkinsonian patients. Fundam Clin Pharmacol 1993; 7: 245–52.
Van Laar T, Van der Geest R, Danhof M, et al. Stepwise intravenous infusion of apomorphine to determine the therapeutic window in patients with Parkinson’s disease. Clin Neuropharmacol 1998; 21: 152–8.
Verhagen Metman L, Locatelli ER, Bravi D, et al. Apomorphine responses in Parkinson’s disease and the pathogenesis of motor complications. Neurology 1997; 48: 369–72.
Pollak P, Champay AS, Hommel M, et al. Subcutaneous apomorphine in Parkinson’s disease [letter]. J Neurol Neurosurg Psychiatry 1989; 52: 544.
Corboy DL, Wagner ML, Sage JI. Apomorphine for motor fluctuations and freezing in Parkinson’s disease. Ann Pharmacother 1995; 29: 282–8.
Hughes AJ, Bishop S, Kleedorfer B, et al. Subcutaneous apomorphine in Parkinson’s disease; response to chronic administration for up to five years. Mov Disord 1993; 6: 165–70.
Kraegen EW, Chrischolm DJ. Pharmacokinetics of insulin: implications for continuous subcutaneous insulin infusion therapy. Clin Pharmacokinet 1985; 10: 303–14.
Sam E, Sarre S, Michotte Y, et al. Distribution of apomorphine enantiomers in plasma, brain tissue and striatal extracellular fluid. Eur J Pharmacol 1997; 329: 9–15.
Neef C, Jelliffe RW, Van Laar T, et al. Population pharmacokinetics of apomorphine in patients with Parkinson’s disease. Drug Invest 1994; 7: 183–90.
Frankel JP, Lees AJ, Kempster PA, et al. Subcutaneous apomorphine in the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry 1990; 53: 96–101.
Durif F, Jeanneau E, Serre-Debeauvais D, et al. Relation between plasma concentration and clinical efficacy after sublingual single dose apomorphine in Parkinson’s disease. Eur J Clin Pharmacol 1991; 41: 493–4.
Hughes AJ, Bishop S, Lees AJ, et al. Rectal apomorphine in Parkinson’s disease. Lancet 1991; 337: 118.
Van der Geest R, Danhof M, Bodde HE. Iontophoretic delivery of apomorphine; in vitro optimisation and validation. Pharm Res 1997; 14: 1797–802.
Van der Geest R, Van Laar T, Gubbens-Stibbe JM, et al. Iontophoretic delivery of R-apomorphine: an in vivo study in patients with Parkinson’s disease. Pharm Res 1997; 14: 1803–9.
Hughes AJ, Lees AJ, Stern GM. The motor response to sequential apomorphine in parkinsonian fluctuations. J Neurol Neurosurg Psychiatry 1991; 54: 358–60.
Grandas F, Gancher S, Lera G, et al. Time interval between repeated injections conditions: the duration of motor improvement to apomorphine in Parkinson’s disease. Neurology 1992; 42: 1287–90.
Gancher ST, Woodward WR, Nutt JG. Apomorphine tolerance in Parkinson’s disease: lack of a dose effect. Clin Neuropharmacol 1996; 19: 59–64.
Baas H, Harder S, Burklin F, et al. Pharmacodynamics of levodopa co-administered with apomorphine in Parkinsonian patients with end-of-dose motor fluctuations. Clin Neuropharmacol 1998; 21: 86–92.
Gjedde A, Wong DF. Modeling neuroreceptor binding of radioligands in vivo. In: Frost JJ, Wagner HN, editors. Quantitative imaging: neuroreceptors, neurotransmitters and enzymes. New York: Raven Press, 1990: 51–80.
Kapoor R, Turjanski M, Frankel, et al. Intranasal apomorphine: a new treatment in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1990; 53: 1015.
Nutt JG, Holford NHG. The response to levodopa in Parkinson’s disease: imposing pharamcological law and order. Ann Neurol 1996; 39: 561–73.
Harder S, Baas H, Röger S, et al. PK-PD relationship of apomorphine in patients with Parkinson’s Disease [abstract PIII-77]. Clin Pharmacol Ther 1995; 59 (2): 207.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neef, C., van Laar, T. Pharmacokinetic-Pharmacodynamic Relationships of Apomorphine in Patients with Parkinson’s Disease. Clin Pharmacokinet 37, 257–271 (1999). https://doi.org/10.2165/00003088-199937030-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-199937030-00004