Abstract
Apomorphine, a short-acting dopamine D1 and D2 receptor agonist, was the first dopamine receptor agonist used to treat Parkinson’s disease. Subcutaneous apomorphine is currently used for the management of sudden, unexpected and refractory levodopa-induced ‘off’ states in fluctuating Parkinson’s disease either as intermittent rescue injections or continuous infusions. Other indications include the challenge test for determining the dopaminergic responsiveness and finding the appropriate dose of the drug in intermittent subcutaneous administration.
Except for a rapid on- and offset of the antiparkinsonian response with subcutaneous apomorphine, the magnitude and pattern of the motor response to single dose of subcutaneously administered apomorphine is qualitatively comparable to that of oral levodopa. Seventy-five percent of patients achieve a clinically significant improvement with a dose of apomorphine 4mg.
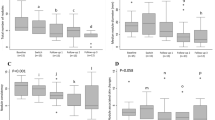
The efficacy of intermittent subcutaneous apomorphine injections as an add-on to levodopa therapy in advanced Parkinson’s disease was explored in one short-term, randomised, double-blind, placebo-controlled trial, one short-term and six long-term, open-label, uncontrolled studies, including a total of 195 patients. These studies provide evidence that this mode of administration was successful in aborting ‘off’ periods and improving Parkinson’s disease motor scores, but tended to increase dyskinesias. No levodopa-sparing effect was observed.
Eleven long-term, open-label, uncontrolled studies, including a total of 233 patients evaluated the efficacy of continuous subcutaneous apomorphine infusions in monotherapy or as an add-on to levodopa therapy in advanced Parkinson’s disease. These studies proved that subcutaneous apomorphine infusions are successful in aborting ‘off’ periods, reducing dyskinesias and improving Parkinson’s disease motor scores with the added benefit of a substantial levodopa-sparing effect.
The apomorphine challenge test has at least 80% overall predictive ability to clinically diagnose Parkinson’s disease across the different stages of the disease and parkinsonian syndromes. Similarly, those data also indicate that the apomorphine challenge test has a >80% ability to predict dopaminergic responsiveness across all stages of Parkinson’s disease.
Adverse events are usually mild and consist predominantly of cutaneous reactions and neuropsychiatric adverse effects. The incidence of adverse effects is higher in patients receiving continuous infusion than in those receiving intermittent pulsatile administration.
Based on the results of these studies it is recommended that subcutaneous apomorphine either as intermittent injections or continuous infusions should be offered to any suitable Parkinson’s disease patient who has difficulties in his/her management with conventional therapy. Low-dose levodopa therapy in combination with waking-day hours subcutaneous apomorphine infusion would probably be the most efficient treatment. Continuous subcutaneous apomorphine infusions should be evaluated before more invasive measures or neurosurgical interventions are contemplated.








Similar content being viewed by others
References
Ehringer H, Hornykiewicz O. Verteilung von Noradrenalin und Dopamin (3-Hydroxytyramin) im Gehirn des Menschen und ihr Verhalten bei Erkrankungen der extrapyramidalen Systems. Klin Wochenschrift 1960; 38: 1236–9
Marsden CD, Parkes JD, Quinn N. Fluctuations and disability in Parkinson’s disease: clinical aspects. In: Marsden CD, Fahn S, editors. Movement disorders. London: Butterworth Scientific, 1982: 96–122
Cantello R, Gilli M, Riccio A, et al. Mood changes associated with ‘end-of-dose’ deterioration in Parkinson’s disease: a controlled study. J Neurol Neurosurg Psychiatry 1986; 49: 1182–90
Hardie RJ, Lees AJ, Stern GM. On-off fluctuations in Parkinson’s disease: a clinical and neuropharmacological study. Brain 1984; 107: 487–506
Nissenbaum H, Quinn NP, Brown RG, et al. Mood swings with the ‘on-off’ phenomenon in Parkinson’s disease. N Engl J Med 1987; 310: 483–8
Quinn NP, Lang AE, Koller WC, et al. Painful Parkinson’s disease. Lancet 1986; I: 1366–9
Marsden CD, Parkes JD. Success and problems of long-term levodopa therapy in Parkinson’s disease. Lancet 1977; I: 345–9
Strange PG. Dopamine receptors in the basal ganglia: relevance to Parkinson’s disease. Mov Disord 1994; 8: 263–70
Robertson GS, Robertson HA. Synergistic effects of Dl and D2 dopamine agonists on turning behaviour in rats. Brain Res 1986; 384: 387–90
Lange KW, Rausch WD, Gsell W, et al. Neuroprotection by dopamine agonists. J Neural Transm Suppl 1994; 43: 183–201
Bedard PJ, Blanchet PJ, Levesque D, et al. Pathophysiology of L-dopa-induced dyskinesias. Mov Disord 1999; 14Suppl. 1: 4–8
Grondin R, Bedard PJ, Britton DR, et al. Potential therapeutic use of the selective dopamine Dl receptor agonist, A-86929: an acute study in parkinsonian levodopa-primed monkeys. Neurology 1997; 49: 421–6
Millan MJ, Maiofiss L, Cussac D, et al. Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes. J Pharmacol Exp Ther 2002; 303: 791–804
Newman-Tancredi A, Cussac D, Audinot V, et al. Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. II. Agonist and antagonist properties at subtypes of dopamine D(2)-like receptor and alpha(l)/alpha(2)-adrenoceptor. J Pharmacol Exp Ther 2002; 303: 805–14
Newman-Tancredi A, Cussac D, Quentric Y, et al. Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. III. Agonist and antagonist properties at serotonin, 5-HT(l) and 5-HT(2), receptor subtypes. J Pharmacol Exp Ther 2002; 303: 815–22
Montastruc JL, Rascol O, Senard JM. Current status of dopamine agonists in Parkinson’s disease management. Drugs 1993; 46: 384–93
Wachtel H. Antiparkinsonian dopamine agonists: a review of the pharmacokinetics and neuropharmacology in animals and humans. J Neural Transm Park Dis Dement Sect 1991; 3: 151–201
Levant B, Dung Ling Z, Carvey PM. Dopamine D3 receptors: relevance for the drug treatment of Parkinson’s disease. CNS Drugs 1999; 12: 391–402
Piercey MF, Hoffmann WE, Smith MW, et al. Inhibition of dopamine neuron firing by pramipexole, a dopamine D3 receptor-preferring agonist: comparison to other dopamine receptor agonists. Eur J Pharmacol 1996; 312: 35–44
Deleu D, Northway MG, Hanssens Y. Clinical pharmacokinetic and pharmacodynamic properties of drugs used in the treatment of Parkinson’s disease. Clin Pharmacokinet 2002; 41: 261–309
Matthiessen A, Wright CRA. Researches into the chemical constitution of the opium bases. Part 1: on the action of hydrochloric acid on morphia. Proc R Soc Lond B Biol Sci 1869; 17: 455–60
Neumeyer JL, Lal S, Baldessarini RJ. Historical highlights of the chemistry, pharmacology, and early clinical uses of apomorphine. In: Gessa GL, Corsini GU, editors. Apomorphine and other dopaminomimetics. Vol 1. Basic pharmacology. New York: Raven Press, 1981: 1–17
Weill E. De l’apomorphine dans certains troubles nerveux. Lyon Med 1884; 48: 411–9
Schwab RS, Amador LV, Lettvin JY. Apomorphine in Parkinson’s disease. Trans Am Neurol Assoc 1951; 76: 251–3
Cotzias GC, Papavasiliou PS, Tolosa ES, et al. Similarities between neurologic effects of L-dopa and apomorphine. N Engl J Med 1970; 282: 31–2
Duby SE, Cotzias GC, Papavasiliou PS, et al. Injected apomorphine and orally administered levodopa in Parkinsonism. Arch Neurol 1972; 27: 474–80
Cotzias GC, Papavasiliou PS, Tolosa ES, et al. Treatment of Parkinson’s disease with aporphines: possible role for growth hormone. N Engl J Med 1976; 297: 567–72
Lees AJ. Dopamine agonists in Parkinson’s disease: a look at apomorphine. Fundam Clin Pharmacol 1993; 7: 121–8
Barker R, Duncan J, Lees AJ. Subcutaneous apomorphine as a diagnostic test for dopaminergic responsiveness in parkinsonian syndromes. Lancet 1989; I: 675–8
Gottlieb S. FDA committee recommends approval for Viagra rival. BMJ 2000; 320: 1094
Hagell P, Odin O. Apomorphine in the treatment of Parkinson’s disease. J Neurosci Nurs 2001; 33: 21–38
Corsini GU, Del Zompo M, Gessa GL, et al. Therapeutic efficacy of apomorphine combined with an extracerebral inhibitor of dopamine receptors in Parkinson’s disease. Lancet 1979; I: 954–6
Olanow CW, Watts RL, Koller WC. An algorithm (decision tree) for the management of Parkinson’s disease (2001): treatment guidelines. Neurology 2001; 56 (11 Suppl. 5): S1–S88
Scarzella L, Delsedime M, Ferrero B, et al. Apomorphine SC treatment in parkinsonian patients with long term L-DOPA syndrome during L-DOPA drug holiday. J Neural Transm Suppl 1995; 45: 163–70
Nutt JG, Gancher ST, Woodward WR. Does an inhibitory action of levodopa contribute to motor fluctuations? Neurology 1988; 38: 1553–7
Harder S, Baas H, Demisch L, et al. Dose response and concentration response relationship of apomorphine in patients with Parkinson’s disease and end-of-dose akinesia. Int J Clin Pharmacol Ther 1998; 36: 355–62
Verhagen Metman L, Locatelli ER, Bravi D, et al. Apomorphine responses in Parkinson’s disease and the pathogenesis of motor complications. Neurology 1997; 48: 369–72
Gancher ST, Woodward WR, Gliessman P, et al. The shortduration response to apomorphine: implications for the mechanism of dopaminergic effects in parkinsonism. Ann Neurol 1990, 5
Harder S, Baas H, Rietbrock S. Concentration-effect relationship of levodopa in patients with Parkinson’s disease. Clin Pharmacokinet 1995; 29: 243–56
Hughes AJ, Lees AJ, Stern GM. Apomorphine in the diagnosis and treatment of parkinsonian tremor. Clin Neuropharmacol 1990; 13: 312–7
Kempster PA, Frankel JP, Stern GM, et al. Comparison of motor response to apomorphine and levodopa in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1990; 53: 1004–7
Hughes AJ, Bishop S, Stern GM, et al. The motor response to repeated apomorphine administration in Parkinson’s disease. Clin Neuropharmacol 1991; 14: 209–13
van Laar T, Jansen EN, Essink AW, et al. A double-blind study of the efficacy of apomorphine and its assessment in ‘off’-periods in Parkinson’s disease. Clin Neurol Neurosurg 1993; 95: 231–5
Nicolle E, Pollak P, Serre-Debeauvais F, et al. Pharmacokinetics of apomorphine in parkinsonian patients. Fundam Clin Pharmacol 1993; 7: 245–52
Gancher ST, Woodward WR Boucher B, et al. Peripheral pharmacokinetics of apomorphine in humans. Ann Neurol 1989; 26: 232–8
Colosimo C, Merello M, Hughes AJ, et al. Motor response to acute dopaminergic challenge with apomorphine and levodopa in Parkinson’s disease: implications for the pathogenesis of the on-off phenomenon. J Neurol Neurosurg Psychiatry 1996; 60: 634–7
Merello M, Pikielny R, Cammarota A, et al. Comparison of subcutaneous apomorphine versus dispersible madopar latency and effect duration in Parkinson’s disease patients: a double-blind single-dose study. Clin Neuropharmacol 1997; 20: 165–7
Rodriguez M, Lera G, Vaamonde J, et al. Motor response to apomorphine and levodopa in asymmetric Parkinson’s disease. J Neurol Neurosurg Psychiatry 1994; 57: 562–6
Sam E, Jeanjean AP, Maloteaux JM, et al. Apomorphine pharmacokinetics in parkinsonism after intranasal and subcutaneous application. Eur J Drug Metab Pharmacokinet 1995; 20: 27–33
Nutt JG, Carter JH. Apomorphine can sustain the long-duration response to L-DOPA in fluctuating PD. Neurology 2000; 54: 247–50
Dewey Jr RB, Hutton JT, Le Witt PA, et al. A randomized, double-blind, placebo-controlled trial of subcutaneously injected apomorphine for parkinsonian off-state events. Arch Neurol 2001; 58: 1385–92
Frankel JP, Lees AJ, Kempster PA, et al. Subcutaneous apomorphine in the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry 1990; 53: 96–101
Esteban Muñoz J, Marti MJ, Marin C, et al. Long-term treatment with intermittent intranasal or subcutaneous apomorphine in patients with levodopa-related motor fluctuations. Clin Neuropharmacol 1997; 20: 245–52
Pietz K, Hagell P, Odin P. Subcutaneous apomorphine in late stage Parkinson’s disease: a long-term follow-up. J Neurol Neurosurg Psychiatry 1998; 65: 709–16
Gancher ST, Nutt JG, Woodward WR. Diurnal responsiveness to apomorphine. Neurology 1987; 37: 1250–3
Hughes AJ, Lees AJ, Stern GM. The motor response to sequential apomorphine in parkinsonian fluctuations. J Neurol Neurosurg Psychiatry 1991; 54: 358–60
Grandas F, Obeso JA. Motor response following repeated apomorphine administration is reduced in Parkinson’s disease. Clin Neuropharmacol 1989; 12: 14–22
Gancher ST, Nutt JG, Woodward WR. Time course of tolerance to apomorphine in parkinsonism. Clin Pharmacol Ther 1992; 52: 504–10
Gancher ST, Woodward WR, Nutt JG. Apomorphine tolerance in Parkinson’s disease: lack of a dose effect. Clin Neuropharmacol 1996; 19: 59–64
Obeso JA, Luquin MR, Grandas F, et al. Motor response to repeated dopaminergic stimulation in Parkinson’s disease. Clin Neuropharmacol 1992; 15: 75–9
Hughes AJ, Bishop S, Kleedorfer B, et al. Subcutaneous apomorphine in Parkinson’s disease: response to chronic administration for up to five years. Mov Disord 1993; 8: 165–70
Gancher ST, Nutt JG, Woodward WR. Apomorphine infusional therapy in Parkinson’s disease: clinical utility and lack of tolerance. Mov Disord 1995; 10: 37–43
Colzi A, Turner K, Lees AJ. Continuous subcutaneous waking day apomorphine in the long-term treatment of levodopa induced interdose dyskinesias in Parkinson’s disease. J Neurol Neurosurg Psychiatry 1998; 64: 573–6
Lozano AM, Lang AE, Levy R, et al. Neuronal recordings in Parkinson’s disease patients with dyskinesias induced by apomorphine. Ann Neurol 2000; 47 (4 Suppl. 1): S141–6
Levy R, Dostrovsky JO, Lang AE, et al. Effects of apomorphine on subthalamic nucleus and globus pallidus internus neurons in patients with Parkinson’s disease. J Neurophysiol 2001; 86: 249–60
Merello M, Lees AJ, Balej J, et al. GPi firing rate modification during beginning-of-dose motor deterioration following acute administration of apomorphine. Mov Disord 1999; 14: 481–3
Muguet D, Broussolle E, Chazot G. Apomorphine in patients with Parkinson’s disease. Biomed Pharmacother 1995; 49: 197–209
van der Geest R, Kruger P, Gubbens-Stibbe JM, et al. Assay of R-apomorphine, S-apomorphine, apocodeine, isoapocodeine and their glucuronide and sulfate conjugates in plasma and urine of patients with Parkinson’s disease. J Chromatogr B Biomed Sci Appl 1997; 702: 131–41
van der Geest R, van Laar T, Kruger PP, et al. Pharmaco-kinetics, enantiomer interconversion, and metabolism of R-apomorphine in patients with idiopathic Parkinson’s disease. Clin Neuropharmacol 1998; 21: 159–68
Holford NH, Sheiner LB. Understanding the dose-effect relationship: clinical application of pharmacokinetic-pharmacodynamic models. Clin Pharmacokinet 1981; 6: 429–53
Przedborski S, Levivier M, Raftopoulos C, et al. Peripheral and central pharmacokinetics of apomorphine and its effect on dopamine metabolism in humans. Mov Disord 1995; 10: 28–36
Hofstee DJ, Neef C, van Laar T, et al. Pharmacokinetics of apomorphine in Parkinson’s disease: plasma and cerebrospinal fluid levels in relation to motor responses. Clin Neuropharmacol 1994; 17: 45–52
Poewe W, Kleedorfer B, Gerstenbrand F, et al. Die Behandelung von Parkinsonpatienten mit L-dopa-wirkungsfluktuation mittels subkutanen Apomorphingaben. Acta Neurol 1989; 16: 73–7
Østergaard L, Werdelin L, Odin P, et al. Pen injected apomorphine against off phenomena in late Parkinson’s disease: a double blind, placebo-controlled study. J Neurol Neurosurg Psychiatry 1995; 58: 681–7
Merello M, Leigurda R. Treatment of motor fluctuations in Parkinson’s disease with subcutaneous injections of apomorphine [in Spanish]. Medicina (B Aires) 1995; 55: 5–10
Stibe C, Lees A, Kempster PA, et al. Subcutaneous apomorphine in parkinsonian on-off oscillations. Lancet 1988; I(8582): 403–6
Stocchi F, Bramante L, Monge A, et al. Apomorphine and lisuride infusion: a comparative chronic study. Adv Neurol 1993; 60: 653–5
Poewe W, Kleedorfer B, Wagner M, et al. Continuous subcutaneous apomorphine infusions for fluctuating Parkinson’s disease. Adv Neurol 1993; 60: 656–9
Wenning GK, Bösch S, Luginger E, et al. Effects of long-term, continuous subcutaneous apomorphine infusions on motor complications in advanced Parkinson’s disease. Adv Neurol 1999; 80: 545–8
Stocchi F, Vacca L, De Pandis MF, et al. Subcutaneous continuous apomorphine infusion in fluctuating patients with Parkinson’s disease: long-term results. Neurol Sci 2001; 22: 93–4
Kaňovsky P, Kubová D, Bareš M, et al. Levodopa-induced dyskinesias and continuous subcutaneous infusions of apomorphine: results of a two-year, prospective follow-up. Mov Disord 2002; 17: 188–91
Manson AJ, Turner K, Lees AJ. Apomorphine monotherapy in the treatment of refractory motor complications of Parkinson’s disease: long-term follow-up study of 64 patients. Mov Disord 2002; 17: 1235–41
Christmas TJ, Kempster PA, Chappie CR, et al. Role of subcutaneous apomorphine in parkinsonian voiding dysfunction. Lancet 1988; II: 1451–3
Mathers SE, Kempster PA, Swash M, et al. Constipation and paradoxical puborectalis contraction in anismus and Parkinson’s disease: a dystonic phenomenon? J Neurol Neurosurg Psychiatry 1988; 51: 1503–7
Mathers SE, Kempster PA, Law P, et al. Anal sphincter dysfunction in Parkinson’s disease. Arch Neurol 1989; 46: 1061–4
Hunter PC, Crameri J, Austin S, et al. Response of parkinsonian swallowing dysfunction to dopaminergic stimulation. J Neurol Neurosurg Psychiatry 1997; 63: 579–83
Tison F, Wiart L, Guatterie M, et al. Effects of central dopaminergic stimulation by apomorphine on swallowing disorders in Parkinson’s disease. Mov Disord 1996; 11: 729–32
Factor SA, Brown DL, Molho ES. Subcutaneous apomorphine injections as a treatment for intractable pain in Parkinson’s disease. Mov Disord 2000; 15: 167–9
Kempster PA, Lees AJ, Crichton P, et al. Off-period belching due to a reversible disturbance of oesophageal motility in Parkinson’s disease and its treatment with apomorphine. Mov Disord 1989; 4: 47–52
Bareš M, Brazdil M, Kanovsky P, et al. The effect of apomorphine administration on smooth pursuit ocular movements in early Parkinsonian patients. Parkinsonism Relat Disord 2003; 9: 139–44
Deleu D. Neurology in clinical practice: an algorithmic approach [online]. Available from URL: http//www.neuroweb.us/ [Accessed 2004 Feb 25]
Hughes AJ, Colosimo C, Kleedorfer B, et al. The dopaminergic response in multiple system atrophy. J Neurol Neurosurg Psychiatry 1992; 55: 1009–13
Wenning C, Ben-Shlomo Y, Magalhaes M, et al. Clinicopathological study of 35 cases of multiple system atrophy. J Neurol Neurosurg Psychiatry 1995; 58: 160–6
Litvan I, Mangone CA, McKee, et al. Natural history of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome) and clinical predictors of survival: a clinicopathological study. J Neurol Neurosurg Psychiatry 1996; 61: 615–20
Hughes AJ. Apomorphine test in the assessment of parkinsonian patients: a meta-analysis. Adv Neurol 1999; 80: 363–8
MacMahon. Use of apomorphine in clinical practice. Adv Neurol 1999; 80: 529–33
Rossi P, Colosimo C, Moro E, et al. Acute challenge with apomorphine and levodopa in Parkinsonism. Eur Neurol 2000; 43: 95–101
Oertel WH, Gasser T, Ippisch R, et al. Apomorphine test for dopaminergic responsiveness. Lancet 1989; I: 1262–3
Hughes AJ, Lees AJ, Stern GM. Apomorphine test to predict dopaminergic responsiveness in parkinsonian syndromes. Lancet 1990; 336: 1262–3
Hughes AJ, Lees AJ, Stern GM. Challenge test to predict the dopaminergic response in untreated Parkinson’s disease. Neurology 1991; 41: 1723–5
D’Costa DF, Abbott RJ, Pye IF, et al. The apomorphine test in parkinsonian syndromes. J Neurol Neurosurg Psychiatry 1991; 54: 870–2
Gasser T, Schwarz J, Arnold G, et al. Apomorphine test for dopaminergic responsiveness inpatients with previously untreated Parkinson’s disease. Arch Neurol 1992; 49: 1131–4
Bonuccelli U, Piccini P, Del Dotto P, et al. Apomorphine test in de novo Parkinson’s disease. Funct Neurol 1992; 7: 295–8
Bonuccelli U, Piccini P, Del Dotto P, et al. Apomorphine test for dopaminergic responsiveness: a dose assessment study. Mov Disord 1993; 8: 158–64
Schelosky L, Hierholzer J, Wissel J, et al. Correlation of clinical response in apomorphine test with D2-receptor status as demonstrated by I123IBZM-SPECT. Mov Disord 1993; 8: 453–8
Baas H, Harder S, Biircklin F, et al. Pharmacodynamics of levodopa coadministered with apomorphine in parkinsonian patients with end-of-dose motor fluctuations. Clin Neuropharmacol 1998; 21: 86–92
Contin M, Riva R, Martinelli P, et al. Longitudinal monitoring of the levodopa concentration-effect relationship in Parkinson’s disease. Neurology 1994; 44: 1287–92
Acland KM, Churchyard A, Fletcher CL, et al. Panniculitis in association with apomorphine infusion. Br J Dermatol 1998; 138: 480–2
van Laar T, van Hilten B, Neef C, et al. The role of EDTA in provoking allergic reactions to subcutaneous infusions of apomorphine in patients with Parkinson’s disease: a histologic study. Mov Disord 1998; 13: 52–5
Ellis C, Lemmens G, Parkes JD, et al. Use of apomorphine in parkinsonian patients with neuropsychiatric complications to oral treatment. Parkinsonism Relat Disord 1997; 3: 103–7
Goulet M, Morissette M, Calon F, et al. Continuous or pulsatile chronic D2 dopamine receptor agonist (U91356A) treatment of drug-naive 4-phenyl-l,2,3,6-tetrahydropyridine monkeys differentially regulates brain D1 and D2 receptor expression: in situ hybridization histochemical analysis. Neuroscience 1997; 79: 497–507
Stocchi F, De Pandis MF, Delfino FA, et al. Transient atrial fibrillation after subcutaneous apomorphine bolus. Mov Disord 1996; 11: 584–5
Sabatini U, Rascol O, Rascol A, et al. Migraine attacks induced by subcutaneous apomorphine in two migrainous parkinsonian patients. Clin Neuropharmacol 1990; 13: 264–7
Vermersch P, Mounier-Vehier F, Caron J, et al. Severe oedema after subcutaneous apomorphine in Parkinson’s disease [letter]. Lancet 1989; II: 802
Loewe R, Puspok-Schwarz M, Petzelbauer P. Apomorphine hyperpigmentation [in German]. Hautarzt 2003; 54: 58–63
Homann CN, Wenzel K, Suppan K, et al. Sleep attacks in patients taking dopamine agonists: review. BMJ 2002; 324: 1483–7
Homann CN, Wenzel K, Suppan K, et al. Sleep attacks with apomorphine. Wien Klin Wochenschr 2002; 114: 430–1
Le WD, Jankovic J. Are dopamine receptor agonists neuroprotective in Parkinson’s disease? Drugs Aging 2001; 18: 389–96
Battaglia G, Busceti CL, Cuomo L, et al. Continuous subcutaneous infusion of apomorphine rescues nigro-striatal dopamine terminals following MPTP injection in mice. Neuropharmacology 2002; 42: 367–73
Gassen M, Glinka Y, Pinchasi B, etal. Apomorphine is a highly potent free radical scavenger in rat brain mitochondrial fraction. Eur J Pharm 1996; 308: 219–25
Grunblatt E, Mandel S, Gassen M, et al. Potent neuroprotective and antioxidant activity of apomorphine in MPTP and 6-hydroxydopamine induced neurotoxicity. J Neural Transm Suppl 1999; 55: 57–70
Grunblatt E, Mandel S, Berkuzki T, et al. Apomorphine protects against MPTP-induced neurotoxicity in mice. Mov Disord 1999; 14: 612–8
Piccini P, Weeks RA, Brooks DJ, et al. Alterations in opioid receptor binding in Parkinson’s disease patients with levodopa-induced dyskinesias. Ann Neurol 1997; 42: 720–6
Brotchie JM. Adjuncts to dopamine replacement: a pragmatic approach to reducing the problems of dyskinesia in Parkinson’s disease. Mov Disord 1998; 13: 871–6
Blanchet PJ, Calon F, Morissette M, et al. Regulation of dopamine receptors and motor behavior following pulsatile and continuous dopaminergic replacement strategies in the MPTP primate model. Adv Neurol 2001; 86: 337–44
Chase TN. The significance of continuous dopaminergic stimulation in the treatment of Parkinson’s disease. Drugs 1998; 55Suppl. 1: 1–9
Youdim MB, Gassen M, Gross A, et al. Iron chelating, antioxidant and cytoprotective properties of dopamine receptor agonist; apomorphine. J Neural Transm Suppl 2000; 58: 83–96
Acknowledgements
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deleu, D., Hanssens, Y. & Northway, M.G. Subcutaneous Apomorphine. Drugs Aging 21, 687–709 (2004). https://doi.org/10.2165/00002512-200421110-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200421110-00001