Abstract
Blood pressure levels are strongly predictive of the risks of first-ever and recurrent stroke. The benefits of blood pressure-lowering therapy for the prevention of fatal and non-fatal stroke in middle-aged individuals are well established. However, until recently, there has been uncertainty about the consistency of such benefits across different patient groups and in particular, for older people and in those with a history of stroke. This paper discusses the evidence surrounding the effectiveness of blood pressure-lowering therapy, specifically in older patients with a history of stroke, with particular attention paid to the results from the Perindopril Protection Against Recurrent Stroke Study (PROGRESS).
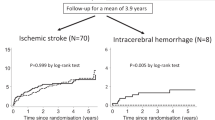
PROGRESS was a randomised, double-blind, placebo-controlled trial of 6105 individuals with a history of cerebrovascular disease recruited from 172 hospital outpatient clinics in ten countries. Participants (mean age 64 years; range 26–91 years) were randomly assigned to receive active treatment with an ACE inhibitor-based blood pressure-lowering regimen (perindopril) with or without addition of the diuretic indapamide, or matched placebo. At the end of follow up (mean of 4 years), active treatment reduced the incidence of total stroke by 28% (95% CI 17–38%) and the rate of major vascular events by 26% (95% CI 16–34%). Importantly, benefits of treatment were consistent across key patient subgroups, including those with and without hypertension, patients who were Asian and non-Asian, and for both ischaemic and haemorrhagic strokes subtypes.
Current evidence is now strong for clinicians to consider blood pressure-lowering therapy as pivotal in the prevention of stroke, especially in patients with a known history of cerebrovascular disease (and vascular disease, in general), irrespective of blood pressure levels, as soon as patients are clinically stable after an acute stroke or other vascular event. Additional age-specific analyses of the PROGRESS data, together with those from other completed trials, will provide more reliable information about the size of the benefits of blood pressure-lowering therapy, specifically for different age groups, and particularly in the oldest old (those aged >80 years). In the meantime though, an ACE inhibitor plus diuretic treatment regimen that maximises the degree of blood pressure reduction has a good safety profile and is an effective treatment that should be considered in all patients with stroke, including the elderly.


Similar content being viewed by others
References
Murray CJL, Lopez AD. Global health statistics. Geneva: World Health Organization, 1996
World Health Organization. The World Health Report 2002. Reducing risks, promoting healthy life. Geneva: World Health Organization, 2002
Bonita R. Epidemiology of stroke. Lancet 1992; 339(8789): 342–4
Whelton PK. Epidemiology of hypertension. Lancet 1994; 344(8915): 101–6
Franklin SS, Gustin IV W, Wong ND, et al. Hemodynamic patterns of age-related changes in blood pressure: The Framingham Heart Study. Circulation 1997; 96(1): 308–15
Burt VL, Culter JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population: data from the health examination surveys, 1960 to 1991. Hypertension 1995; 26(1): 60–9
MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease: part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990; 335: 765–74
Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, coronary heart disease: part 2, short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet 1990; 336: 827–38
Progress Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 2001; 358(9287): 1033–41
Kilander L Boberg M, Lithell H. How do we treat, or not treat, high blood pressure in the oldest old? Blood Press 1997; 6: 372–6
Sowers JR, Lester M. Hypertension, hormones, and aging. J Lab Clin Med 2000; 135(5): 379–86
Prospective Studies Collaboration. Cholesterol, diastolic blood pressure and stroke; 13,000 strokes in 45,000 people in 45 prospective cohorts. Lancet 1995; 346: 1647–53
Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol and stroke in Eastern Asia. Lancet 1998; 352(9143): 1801–7
Asia Pacific Cohort Studies Collaboration. Determinants of cardiovascular disease in the Asia Pacific region: protocol for a collaborative overview of cohort studies. CVD Prevention 1999; 2: 281–9
Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–13
Asia Pacific Cohort Studies Collaboration. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens 2003. In Press
Anonymous. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991; 265(24): 3255–64
Dahlof B, Lindeholm LH, Hansson L, et al. Morbidity and mortality in the Swedish trial in old patients with hypertension (STOP-Hypertension). Lancet 1991; 304: 1281–4
Peart S BP, Broughton PB, Dollery C, et al. Medical Research Council trial of hypertension in older adults: principal results. BMJ 1992; 293: 1281–5
Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet 1997; 350: 757–64
Hansson L, Lithell H, Skoog I, et al. Study on cognition and prognosis in the elderly (SCOPE). Blood Press 1999; 8: 177–83
Dahlöf B, Devereux RB, Kieldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359: 995–1003
ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomised to angiotensinconverting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-lowering Treatment to Prevent Heart Attack trial (ALLHAT). JAMA 2002; 288: 2981–97
MacMahon S, Rodgers A. The effects of antihypertensive treatment on vascular disease: reappraisal of the evidence in 1994. J Vasc Med Biol 1993; 4(5–6): 265–71
MacMahon S, Rodgers A. The effects of blood pressure reduction in older patients: an overview of five randomized controlled trials in elderly hypertensives. Clin Exp Hypertens 1993; 15(6): 967–78
Insua JT, Sacks HS, Lau TS, et al. Drug treatment of hypertension in the elderly: a meta-analysis. Ann Intern Med 1994; 121(5): 355–62
Gueyffier F, Boutitie F, Boissel JP, et al. INDANA: a metaanalysis on individual patient data in hypertension: protocol and preliminary results. Therapie 1995; 50(4): 353–62
Gueyffier F, Froment A, Gouton M. New meta-analysis of treatment trials of hypertension: improving the estimate of therapeutic benefit. J Hum Hypertens 1996; 10(1): 1–8
Messerli FH, Grossman E, Goldbourt U. Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review. JAMA 1998; 279(23): 1903–7
Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: metaanalysis of outcome trials. Lancet 2000; 355(9207): 865–72
Mulrow C, Lau J, Cornell J, et al. Pharmacotherapy for hypertension in the elderly. Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 1. Oxford: Update Software, 2002
Coope J, Warrender TS. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J (Clin Res Ed) 1986; 293(6555): 1145–51
Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000; 342(3): 145–53
Anonymous. Randomized double-blind comparison of a calcium antagonist and a diuretic in elderly hypertensives: National Intervention Cooperative Study in Elderly Hypertensives Study Group. Hypertension 1999; 34(5): 1129–33
Casiglia E, Spolaore P, Mazza A, et al. Effect of two different therapeutic approaches on total and cardiovascular mortality in a Cardiovascular Study in the Elderly (CASTEL). Jpn Heart J 1994; 35(5): 589–600
Gueyffier F, Bulpitt C, Boissel J, et al. Antihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. Lancet 1999; 353: 793–6
Gueyffier F, Boissel JP, Boutitie F, et al. Effect of antihypertensive treatment in patients having already suffered from stroke: gathering the evidence. The INDANA (Individual Data Analysis of Antihypertensive intervention trials) Project Collaborators. Stroke 1997; 28(12): 2557–62
Rodgers A, Neal B, MacMahon S. The effects of blood pressure lowering in cerebrovascular disease: an overview of randomized controlled trials. Neurol Rev Int 1997; 12(1): 12–5
PAT Collaborating Group. Post-stroke antihypertensive treatment study: a preliminary result. Chin Med J 1995; 108: 710–7
Bosch J, Yusuf S, Pogue J, et al. Use of ramipril in preventing stroke: double blind randomised trial. BMJ 2002; 324: 699–702
Meredith PA. Is postural hypotension a real problem with antihypertensive medication? Cardiology 2001; 96Suppl. 1: 19–24
Stewart IM. Relation of reduction in pressure to first myocardial infarction in patients receiving treatment for severe hypertension. Lancet 1979; I(8121): 861–5
Kannel WB, D’Agostino RB, Silbershatz H. Blood pressure and cardiovascular morbidity and mortality rates in the elderly. Am Heart J 1997; 134(4): 758–63
Cruickshank JM. The J curve lives [letter]. Lancet 1992; 339(8786): 187
Cruickshank JM. J curve in antihypertensive therapy: does it exist? A personal point of view. Cardiovasc Drugs Ther 1994; 8(5): 757–60
D’Agostino RB, Belanger AJ, Kannel WB, et al. Relation of low diastolic blood pressure to coronary heart disease death in presence of myocardial infarction: the Framingham Study. BMJ 1991; 303(6799): 385–9
Farnett L, Mulrow CD, Linn WD, et al. The J-curve phenomenon and the treatment of hypertension: is there a point beyond which pressure reduction is dangerous? JAMA 1991; 265(4): 489–95
Rodgers A, MacMahon S, Gamble G, et al. Blood pressure and risk of stroke in patients with cerebrovascular disease. The United Kingdom Transient Ischaemic Attack Collaborative Group. BMJ 1996; 313(7050): 147
Alderman MH. Blood pressure J-curve: is it cause or effect? Curr Opin Nephrol Hypertens 1996; 5(3): 209–13
Cruickshank JM, Thorp JM, Zacharias FJ. Benefits and potential harm of lowering high blood pressure. Lancet 1987; I(8533): 581–4
Cruickshank JM. Antihypertensive treatment and the J-curve. Cardiovasc Drugs Ther 2000; 14(4): 373–9
MacMahon S, Rodgers A, Neal B, et al. Blood pressure lowering for the secondary prevention of myocardial infarction and stroke. Hypertension 1997; 29(2): 537–8
Sleight P. Lowering of blood pressure and artery stiffness [letter]. Lancet 1997; 349(9048): 362
Neaton JD, Blackburn H, Jacob D, et al. Serum cholesterol level and mortality findings for men screened in the multiple risk factor intervention trial Research Group. Arch Intern Med 1992; 152(25): 814–20
McMurray J, McInnes GT. The J-curve hypothesis. Lancet 1992; 339(8792): 561–2
Pfeffer MA. Angiotensin-converting enzyme inhibition in congestive heart failure: benefit and perspective. Am Heart J 1993; 126 (3 Pt 2): 789–93
Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet 1999; 354(9192): 1751–6
Progress Collaborative Group. The lowering of blood-pressure after stroke [letter]. Lancet 2001; 358(9297): 1994–5
Horn J, de Haan RJ, Vermeulen M, et al. Very early nimodipine use in stroke (VENUS): a randomized, double-blind, placebo-controlled trial. Stroke 2001; 32(2): 461–5
Horn J, Limburg M. Calcium antagonists for ischemic stroke: a systematic review. Stroke 2001; 32(2): 570–6
Neal B, MacMahon S, Chapman N, et al. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists. Lancet 2000; 356(9246): 1955–64
Lonn EM, Yusuf S, Jha P, et al. Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation 1994; 90(4): 2056–69
Acknowledgements
Professor Anderson is a member of the PROGRESS Management Committee and Dr Ratnasabapathy was a Research Fellow associated with the PROGRESS study. Dr Lawes is supported by a Research Training Fellowship of the Health Research Council of New Zealand and is associated with the Asia Pacific Cohort Studies Collaboration. No external funds were used in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ratnasabapathy, Y., Lawes, C.M.M. & Anderson, C.S. The Perindopril Protection Against Recurrent Stroke Study (PROGRESS). Drugs Aging 20, 241–251 (2003). https://doi.org/10.2165/00002512-200320040-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200320040-00001