Summary
Synopsis
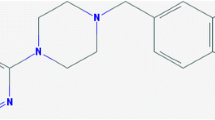
Pramipexole is an orally active non-ergoline dopamine agonist with selective activity at dopamine receptors belonging to the D2 receptor subfamily (D2, D3, D4 receptor subtypes) and with preferential affinity for the D3 receptor subtype. It is approved as monotherapy in early Parkinson’s disease and as adjunctive therapy to levodopa in patients with advanced disease experiencing motor effects because of diminished response to levodopa. The potential neuroprotective effects of pramipexole have been shown in animal and in vitro studies.
Data from relatively long term (10- or 31- week) studies suggest that pramipexole monotherapy (0.375 to 6.0 mg/day) can improve activities of daily living and motor symptoms in patients with early Parkinson’s disease. Pramipexole (0.375 to 4.5 mg/day for 31 or 36 weeks), as an adjunct to levodopa in advanced disease, improved activities of daily living and motor symptoms, reduced the duration and severity of ‘off’ periods and allowed a reduction in levodopa dosage. Mentation, behaviour and mood [Unified Parkinson’s Disease Rating Scale (UPDRS) part I], and timed walking test were not significantly improved. The extent of disability improved according to the UPDRS parts II and III but, when assessed by secondary efficacy parameters, it is unclear whether disability or the severity of disease improved. No significant differences were observed in patients randomised to pramipexole or bromocriptine according to a secondary hypothesis in a prospective study in which both drugs were better than placebo. Some quality- of- life measures improved with active treatment relative to placebo. Further studies comparing pramipexole with other dopamine agonists and levodopa in patients with early and advanced Parkinson’s disease would be useful.
In pramipexole recipients with early disease, the most commonly experienced adverse events were nausea, dizziness, somnolence, insomnia, constipation, asthenia and hallucinations. The most commonly reported adverse events in pramipexole recipients with advanced disease were orthostatic hypotension, dyskinesias, extrapyramidal syndrome (defined as a worsening of the Parkinson’s disease), dizziness, hallucinations, accidental injury, dream abnormalities, confusion, constipation, asthenia, somnolence, dystonia, gait abnormality, hypertonia, dry mouth, amnesia and urinary frequency. The incidence of some adverse events did not greatly differ between pramipexole and placebo recipients.
Conclusions. Pramipexole is effective as adjunctive therapy to levodopa in patients with advanced Parkinson’s disease. However, the potential beneficial effects of pramipexole on disease progression need to be confirmed in clinical studies. The efficacy of pramipexole monotherapy in patients with early disease has also been demonstrated, although the use of dopamine agonists in early Parkinson’s disease remains controversial.
Pharmacodynamic Properties
In vitro and in vivo studies have confirmed that pramipexole is a pre- and postsynaptic agonist at the dopamine D2 receptor subfamily (D2, D3, D4 receptor subtypes) with preferential affinity for the dopamine D3 receptor subtype.
The action of pramipexole at dopamine D2 receptors was confirmed by an increase in behavioural effects involving dopamine D2 receptor stimulation (yawning, stretching and penile erection), or a decrease in basal and stimulated prolactin secretion and a reduction in extracellular levels of dopamine and its metabolites in animals receiving the drug.
The dose-dependent reduction in neuronal firing rates observed after administration of pramipexole demonstrates that it is a full dopamine D2 agonist. Pramipexole acts at presynaptic dopamine D2 autoreceptors and postsynaptic dopamine D2 receptors: it produced an improvement in parkinson-like signs in monkeys with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced degeneration of presynaptic dopamine neurons; inhibition of locomotor activity at low doses and induction at high doses; induction of stereotypical behaviour; antagonism of induced akinesia and decreased body temperature in rats; and induction of circling behaviour in unilaterally 6-hydroxydopamine-lesioned rats. Pramipexole decreased extracellular dopamine but not acetylcholine levels in rats, which indicates that it has a stronger action on presynaptic than on postsynaptic dopamine D2 receptors. Pramipexole antagonised γ-butyrolactone-induced dopamine synthesis and D,L-α-methyltyrosine methylester-induced dopamine reduction further demonstrating its action at presynaptic autoreceptors. The effects of pramipexole were decreased by the dopamine D2 receptor antagonist haloperidol but not the dopamine D1 receptor antagonist SCH 23390.
Preferential affinity for dopamine D3 receptors has been shown in in vitro binding studies with a 6.6- to 7.8-fold higher affinity to dopamine D3 than to D2 receptor subtypes.
Potential neuroprotective effects of pramipexole were demonstrated in rats: the drug attenuated 3-acetylpyridine (3-AP)-induced decreases in cerebellar cGMP (cyclic guanosine monophosphate) and ATP (adenosine triphosphate) levels, reduced 3-AP-induced loss of motor coordination and prevented 3-AP-induced loss of inferior olivary neurons. Furthermore, methamphetamine-induced loss of nigrostriatal neurons was attenuated by pramipexole in mice. MPTP-induced decreases in striatal dopamine concentrations were also inhibited by pramipexole in mice. In addition, pramipexole reduced dopamine- and levodopa-induced cytotoxicity and stimulated dopamine neuronal growth factor in in vitro studies. The potential free radical scavenging properties of pramipexole were demonstrated by its low oxidation potential in a preliminary in vitro study.
Pramipexole demonstrated a moderate affinity for α2-adrenoceptors and very low affinity for α1-adrenergic, β-, muscarinic and serotonin 5-HT receptors.
Pharmacokinetic Properties
Pramipexole exhibits linear pharmacokinetics over the dose range 0.125 to 1.5mg administered every 8 hours in healthy volunteers. After administration of pramipexole 4.5 mg/day, the maximum plasma concentration (Cmax) was 5.44 μg/L in men and 7.17 μg/L in women; corresponding area under the plasma concentration-time curve (AUC) values were 34.7 and 47.5 μg/L · h. Pramipexole has a large volume of distribution (Vd; 520 and 460L in men and women, respectively). The elimination half-life (t½) of pramipexole is 11.6 and 14.1 hours and the main route of elimination is renal [renal clearance (CLR) accounts for 70 to 80% of the total clearance of an oral dose (CLPO)].
In volunteers with renal disease, the CLPO of pramipexole decreased and t½ increased with decreasing renal function; CLPO was 53 to 68% lower than in those with normal renal function and t½ increased from 11.3 to 15.3 or 38.4 hours depending on the severity of renal disease. No differences were observed in Cmax, time to reach Cmax(tmax) or Vdarea/oral bioavailability (F) [Vdarea is equivalent to Vdβ and is the Vd during the β elimination phase]. Less than 9% of the dose was cleared by haemodialysis.
Pramipexole is secreted by the renal organic cation transport system. Coadministration with cimetidine decreased the CLPO of pramipexole by 31.8 and 35.1% and CLR by 30.2 and 38.6% in male and female volunteers, respectively, and increased the t½ of pramipexole by 40.5%. Probenecid decreased the CLPO of pramipexole by 10.3% in both genders and CLR by 19.6% in female participants. Gender differences may result from differences in weight or creatinine clearance (CLCR).
Gender differences are observed in CLR and CLPO, AUC, Cmax and the minimum plasma concentration (Cmin). Pramipexole clearance was 23% lower in women than men after a single dose. AUC, Cmax and Cmin were, respectively, 27, 24 and 35% lower in men than women after multiple doses of pramipexole 4.5 mg/day, which was attributed to the high CLPO in men.
In elderly volunteers, the t½ of pramipexole was longer (12 vs 8.5 hours) and CLPO values 25 to 29% lower than in younger volunteers. AUC also showed age differences which correlated with the changes in CLPO. No differences were observed in Cmax, tmax Or Vdarea/F.
Therapeutic Efficacy
Early Disease. Pramipexole monotherapy (0.375 to 6 mg/day) administered for 10 or 31 weeks improved the symptoms of early Parkinson’s disease. Mean total Unified Parkinson’s Disease Rating Scale (UPDRS) scores improved by 20% in one study. In a second study, UPDRS part II scores (Activities of Daily Living) improved by 22% and part III scores (motor symptoms) by 25%. The efficacy of pramipexole was generally greater in patients with more severe disease at baseline.
Advanced Disease. In patients experiencing motor fluctuations during long term levodopa therapy, pramipexole 0.375 to 4.5 mg/day, as an adjunct to levodopa for 31 or 36 weeks, improved UPDRS part II scores by 22 or 26.7% and part III scores by 25 or 34.9%. Pramipexole reduced the extent of disability and severity of disease in 1 of 2 studies when assessed by secondary efficacy measures, but no improvement was observed in part I of the UPDRS (mentation, behaviour and mood) or timed walking test, relative to placebo, in either study.
The relative improvement in ‘off’ periods in patients receiving pramipexole was 31 or 45.6% and the ‘off’ period severity was reduced by 17%. The levodopa dosage was reduced by 27% in pramipexole recipients. Dyskinesias were significantly reduced during pramipexole therapy when evaluated by UPDRS part IV (complications of therapy) in 1 of 2 studies but not when assessed in both studies using the Parkinson Dyskinesia Scale.
In the 36-week prospective study, no significant differences were observed between patients randomised to pramipexole (mean dose 3.36 mg/day) or bromocriptine (mean dose 22.64 mg/day) according to secondary hypothesis testing in which both drugs were better than placebo. However, pramipexole, but not bromocriptine, significantly reduced the percentage of the day patients spent in ‘off’ periods relative to placebo. This study did not have adequate power to detect differences between pramipexole and bromocriptine.
Some Functional Status Questionnaire quality-of-life measures significantly improved after pramipexole compared with placebo. No significant differences were observed in quality- of-life measures between pramipexole and bromocriptine, although pramipexole, but not bromocriptine, recipients tended to have better European Quality of Life (EuroQoL) scores than patients receiving placebo.
Tolerability
In patients with early disease, the most commonly reported adverse events that occurred more frequently in pramipexole than in placebo recipients were nausea, dizziness, somnolence, insomnia, constipation, asthenia and hallucinations.
Most commonly reported adverse events occurring more frequently in pramipexole than in placebo recipients with advanced disease were orthostatic hypotension, dyskinesias, extrapyramidal syndrome (defined as a worsening of the Parkinson’s disease), insomnia, dizziness, hallucinations, accidental injury, dream abnormalities, confusion, constipation, asthenia, somnolence, dystonia, gait abnormality, hypertonia, dry mouth, amnesia and urinary frequency.
In both groups of patients, the incidence of some adverse events did not greatly differ between pramipexole and placebo recipients.
The most common causes of treatment discontinuation were nervous system and gastrointestinal events in patients with early disease, and nervous system and cardiovascular events in patients with advanced disease.
In one study, 99% of pramipexole recipients and 93% of patients receiving bromocriptine reported adverse events; these events led to discontinuation by 20% of patients in each group. However, relative tolerability between the 2 active treatments could not be evaluated because both drugs were titrated mainly according to tolerability.
Dosage and Administration
Pramipexole dihydrochloride 4.5mg is equivalent to 3.3mg of pramipexole base. Doses in this section refer to the salt of pramipexole and have been obtained from the prescribing information available in the US and in Europe.
As with other dopamine agonists, pramipexole should be initiated at a low dosage (0.375 mg/day) that should be increased gradually, until symptoms are relieved (maximum dosage is 4.5 mg/day given in 3 divided doses), to minimise the occurrence of adverse events including orthostatic hypotension. The maintenance dosage ranges from 0.375 to 4.5 mg/day (generally 1.5 mg/day). These recommendations are for patients with early disease requiring monotherapy and for those with advanced disease receiving concomitant levodopa.
A lower starting and maintenance dosage is recommended in patients with renal impairment but there is inadequate information on the use of pramipexole in those with very severe renal disease (CLCR < 0.9 L/h) and haemodialysis patients. Although not studied, hepatic impairment is unlikely to influence the pharmacokinetics of pramipexole, since the drug is mainly eliminated via the renal route.
A 20% decrease in the CLPO of pramipexole may result from the coadministration of other drugs eliminated via the cationic transport system, and pramipexole may inhibit the clearance of these drugs. Cimetidine can increase the AUC of pramipexole by 50% and increase the t½ by 40%. The efficacy of pramipexole can be reduced by the addition of dopamine antagonists. Pramipexole may increase the Cmax of levodopa by 40% and decrease the tmax from 2.5 to 0.5 hours. Selegiline, amantadine, levodopa/carbidopa, drugs eliminated via the anionic transport system and cytochrome P450 inhibitors are unlikely to affect pramipexole.
Similar content being viewed by others
References
Gottwald MD, Bainbridge JL, Dowling GA, et al. New pharmacotherapy for Parkinson’s disease. Ann Pharmacother 1997 Oct; 31: 1205–17
Carter AJ, Müller RE. Pramipexole, a dopamine D2 autoreceptor agonist, decreases the extracellular concentration of dopamine in vivo. Eur J Pharmacol 1991 Jul 23; 200: 65–72
Piercey MF, Hoffmann WE, Smith MW, et al. Inhibition of dopamine neuron firing by pramipexole, a dopamine D3 receptor-preferring agonist: comparison ot other dopamine receptor agonists. Eur J Pharmacol 1996 Sep 19; 312: 35–44
Camacho-Ochoa M, Evans DL, Walker EL, et al. Receptor binding autoradiography with pramipexole, a clinically useful D3-preferring dopamine agonist [abstract]. Neuropsychopharmacology 1994 May; 10 Suppl. Pt 3: 30
Carvey PM, Pieri S, Ling ZD. Attenuation of levodopa-induced toxicity in mesencephalic cultures by pramipexole. J Neural Transm Gen Sect 1997; 104(2–3): 209–28
Carlsson A, Piercey MF. Dopamine-receptor subtypes in neurological and psychiatric disease. Clinical Neuropharmacology 1995; 18Suppl. 1: S1–5
Piercey MF, Camacho-Ochoa M, Smith MW. Functional roles for dopamine-receptor subtypes. Clin Neuropharmacol 1995; 18Suppl. 1: S34–42
Piercey MF, Walker EL, Feldpausch DL, et al. High affinity binding for pramipexole, a dopamine D3 receptor ligand, in rat striatum. Neurosci Lett 1996; 219(2): 138–40
Mierau J, Schneider FJ, Ensinger HA, et al. Pramipexole binding and activation of cloned and expressed dopamine D2, D3 and D4 receptors. Eur J Pharmacol Mol Pharmacol 1995 Jun 23; 290: 29–36
Matsumoto S-i, Yamada K, Nagashima M, et al. Occurrence of yawning and decrease of prolactin levels via stimulation of dopamine D2-receptors after administration of SND 919 in rats. Naunyn Schmiedebergs Arch Pharmacol 1989 Jul; 340: 21–5
Ferrari F, Pelloni F, Giuliani D. Behavioural evidence that different neurochemical mechanisms underly stretching-yawning and penile erection induced in male rats by SND 919, a new selective D2 dopamine receptor agonist. Psychopharmacology 1993 Dec; 113: 172–6
Maj J, Rogóz Z, Skuza G, et al. The behavioural effects of pramipexole, a novel dopamine receptor agonist. Eur J Pharmacol 1997 Apr 11; 324: 31–7
Mierau J, Schingnitz G. Biochemical and pharmacological studies on pramipexole, a potent and selective dopamine D2 receptor agonist. Eur J Pharmacol 1992 May 14; 215: 161–70
Robertson GS, Tham C-S, Wilson C, et al. In vivo comparisons of the effects of quinpirole and the putative presynaptic dopaminergic agonists B-HT 920 and SND 919 on striatal dopamine and acetylcholine release. J Pharmacol Exp Ther 1993 Mar; 264: 1344–51
Sethy VH, Wu HY, Oostveen JA, et al. Neuroprotective effects of the dopamine agonists pramipexole and bromocriptine in 3-acetylpyridine-treated rats. Brain Res 1997 Apr 18; 754: 181–6
Kitamura Y, Kohno Y, Nakazawa M, et al. Inhibitory effects of talipexole and pramipexole on MPTP-induced dopamine reduction in the striatum of C57BL/6N mice. Jpn J Pharmacol 1997 May; 74: 51–7
Hall ED, Andrus PK, Oostveen JA, et al. Neuroprotective effects of the D2/D3 agonist pramipexole against postischemic or methamphetamine-induced degeneration of nigrostriatal neurons. Brain Res 1996; 742: 80–8
Le WD, Zou LL, Rowe DB, et al. Neuroprotection of pramipexole against dopamine- and levodopa-induced cytotoxicity [abstract]. Mov Disord 1997 Sep; 12: 840
Domino EF, Ni L, Zhang H, et al. Talipexole or pramipexole combinations with chloro-APB (SKF 82958) in MPTP-induced hemiparkinsonian monkeys. Eur J Pharmacol 1997 May 1; 325: 137–44
Wright CE, Lasher Sisson T, Ichhpurani AK, et al. Influence of renal impairment and hemodialysis on pramipexole pharmacokinetics [abstract]. Mov Disord 1997; 12Suppl. 1: 66
Wright CE, Lasher Sisson T, Ichhpurani AK, et al. Influence of probenecid and cimetidine on pramipexole pharmacokinetics [abstract]. Clin Pharmacol Ther 1996 Feb; 59: 183
Wright CE, Lasher Sisson T, Ichhpurani AK, et al. Influence of age and gender on pramipexole pharmacokinetics [abstract]. Clin Pharmacol Ther 1996 Feb; 59: 184
Wright CE, Lasher Sisson T, Ichhpurani AK, et al. Steady-state pharmacokinetic properties of pramipexole in healthy volunteers. J Clin Pharmacol 1997 Jun; 37: 520–5
Hubble JP, Koller WC, Cutler NR, et al. Pramipexole in patients with early Parkinson’s disease. Clin Neuropharmacol 1995 Aug; 18: 338–47
Molho ES, Factor SA, Weiner WJ, et al. The use of pramipexole, a novel dopamine (DA) agonist, in advanced Parkinson’s disease. J Neural Transm 1995; 10Suppl. 45: 225–30
Parkinson Study Group. Safety and efficacy of pramipexole in early Parkinson disease: a randomized dose-ranging study. JAMA 1997 Jul 9; 278: 125–30
Shannon KM, Bennett Jr JP, Friedman JH. Efficacy of pramipexole, a novel dopamine agonist, as monotherapy in mild to moderate Parkinson’s disease. Neurology 1997 Sep; 49: 724–8
Lieberman A, Ranhosky A, Korts D. Clinical evaluation of pramipexole in advanced Parkinson’s disease: results of a double-blind, placebo-controlled, parallel-group study. Neurology 1997 Jul; 49: 162–8
Guttman M, International Pramipexole-Bromocriptine Study Group. Double-blind comparison of pramipexole and bromocriptine treatment with placebo in advanced Parkinson’s disease. Neurology 1997 Oct; 49: 1060–5
Hagan JJ, Middlemiss DN, Sharpe PC, et al. Parkinson’s disease: prospects for improved drug therapy. Trends Pharmacol Sci 1997 May; 18: 156–63
Pharmacia and Upjohn Company. Pramipexole prescribing information. Kalamazoo, Michigan, USA, 1997
Boehringer Ingelheim International GmbH. Sifrol summary of product characteristics. Ingelheim am Rhein, Germany, 1998
Ahlskog JE, Cornelia CL, Hubble JP, et al. An algorithm for the management of Parkinson’s disease. Neurology 1994 Dec; 44Suppl. 10: S9–52
The treatment of Parkinson’s disease. MeReC Bull 1996 Nov; 7: 41–4
Poewe WH, Wenning GK. The natural history of Parkinson’s disease. Neurology 1996 Dec; 47Suppl. 3: S146–152
Watts RL. The role of dopamine agonists in early Parkinson’s disease. Neurology 1997 Jul; 49Suppl. 1: S34–48
Mizuno Y, Mori H, Kondo T. Practical guidelines for the drug treatment of Parkinson’s disease. CNS Drugs 1994 Jun; 1: 410–26
Bodagh IYO, Robertson DRC. A risk-benefit assessment of drugs used in the management of Parkinson’s disease. Drug Saf 1994 Aug; 11: 94–103
Hughes AJ. Drug treatment of Parkinson’s disease in the 1990s: achievements and future possibilities. Drugs 1997 Feb; 53: 195–205
Pfeiffer R. Optimization of levodopa therapy. Neurology 1992 Jan; 42Suppl. 1: 39–43
Plosker GL, Benfield P. Talipexole. Drugs 1997 May; 7: 410–6
Quinn N. Drug treatment of Parkinson’s disease. BMJ 1995 Mar 4; 310: 575–9
Caspi A. Pramipexole, a dopamine agonist for the treatment of Parkinson’s disease. PT 1997 Mar; 22: 155–7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dooley, M., Markham, A. Pramipexole. Drugs & Aging 12, 495–514 (1998). https://doi.org/10.2165/00002512-199812060-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-199812060-00007