Abstract
Background: It has been shown that the abrupt cessation of treatment with β-adrenoceptor antagonists (β-blockers) increases the risk of myocardial infarction in patients with hypertension. As β-blockers differ in their pharmacokinetic and pharmacodynamic properties, this risk of discontinuation might also differ between subgroups of β-blockers.
Objective: To determine whether discontinuation of β-blockers is associated with an increased risk of myocardial infarction in elderly patients and whether the effects of recent cessation differs between subgroups of β-blockers, categorised according to their selectivity, lipophilic profile and intrinsic sympathomimetic activity (ISA).
Design: A cohort study in users of β-blockers within the Rotterdam Study, which was a prospective population-based follow-up study of 7983 individuals aged ≥55 years.
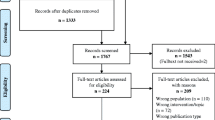
Patients: We identified 2588 individuals who had been treated with a β-blocker for at least 30 days at any time during the study period of 1 January 1991 to 1 January 2002. In this group, 148 subjects developed incident myocardial infarction.
Methods: Detailed information on the medication use and clinical characteristics of all patients were collected from the files of pharmacies, general practices and hospitals. Myocardial infarction was diagnosed on the basis of internationally accepted criteria and verified by a cardiologist. The duration of β-blocker use was calculated from computerised pharmacy records on the basis of the number of dispensed tablets or capsules and the prescribed daily number.
For every individual, on the index date (date of myocardial infarction in cases, the same date in controls [defined as any patient who had not experienced a myocardial infarction up to that timepoint]) the usage of β-blockers was determined and classified as either current or as past use. Past use was classified into three different periods: cessation of β-blockers less than 30 days; between 30 and 180 days; and more than 180 days before the index date. The risk of myocardial infarction in the three periods of cessation of exposure were analysed using a Cox proportional hazards model that included potential confounders and cardiac comedication. These analyses were performed for the whole group and for subgroups of β-blockers.
Results: Discontinuation of any β-blocker was not associated with an increased risk of myocardial infarction compared with current use of a β-blocker. Analyses within subgroups showed that discontinuation of selective β-blockers was associated with an increased risk of myocardial infarction compared with current use of any β-blocker within the first 30 days (relative risk [RR] 2.70; 95% CI 1.06, 6.89) and also between 30 and 180 days after discontinuation (RR 2.44; 95% CI 1.07, 5.59). No increased risk was demonstrated in the other β-blocker subgroups.
Conclusion: Overall, discontinuation of β-blockers was not associated with an increased risk of myocardial infarction. However, when analysed by β-blocker subgroup, cessation of selective β-blockers was associated with an increased risk of myocardial infarction during the first 180 days after discontinuation.



Similar content being viewed by others
References
Prichard BNC, Waiden RJ. The syndrome associated with the withdrawal of β-adrenergic receptor blocking drugs. Br J Clin Pharmacol 1982; 13: 337–43
Rangno RE, Langlois S. Comparison of withdrawal phenomena after propranolol, metoprolol and pindolol. Br J Clin Pharmacol 1982; 13: 345–51
Frishman WH. β-Adrenergic blocker withdrawal. Am J Cardiol 1987; 59(13): 26F-32F
Hart GR, Anderson RJ. Withdrawal syndromes and the cessation of antihypertensive therapy. Arch Intern Med. 1981; 141: 1125–7
Psaty BM, Koepsell TD, Wagner EH, et al. The relative risk of incident coronary heart disease associated with recently stopping the use of β-blockers. JAMA 1990; 263: 1653–7
Psaty BM, Heckbert SR, Koepsell TD, et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA 1995; 247: 620–5
Hofman A, Grobbee DE, de Jong PT, et al. Determinants of disease and disability in the elderly: the Rotterdam Elderly Study. Eur J Epidemiol 1991; 7: 403–22
Bots ML, Hoes AW, Koudstaal PJ, et al. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation 1997; 96: 1432–7
Sjahid SI, Van der Linden PD, Stricker BHCh. The agreement between the pharmacy medication history and patient interview for cardiovascular drugs: the Rotterdam elderly study. Br J Clin Pharmacol 1998; 45: 591–5
Hardman JG, Limbird LE, editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 10th ed. San Diego (CA): McGraw-Hill, 2005
Sweetman SC, editor. Martindale: the complete drug reference. 34th ed. London (UK): Pharmaceutical Press, 2005
Bleumink GS, Knetsch AM, Sturkenboom MCJM, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk, sand prognosis of heart failure — the Rotterdam study. Eur Heart J 2004; 25: 1614–9
Shammash JB, Trost JC, Gold JM, et al. Perioperative β-blocker withdrawal and mortality in vascular surgical patients. Am Heart J 2001; 141: 148–52
Hoeks SE, Scholte op Reimer WJM, van Urk H, et al. Increase of 1 -year mortality after perioperative beta-blocker withdrawal in endovascular and vascular surgery patients [online]. Eur J Vasc Endovasc Surg 2007 Jan; 33(1): 13–9
Bolli P, Buhler FR, Raeder EA. Lack of beta-adrenoreceptor hypersensitivity after abrupt withdrawal of long-term therapy with oxprenolol. Circulation 1981; 64: 1130–4
NHG Standaard Hypertensie until december 2005 [online]. Available from URL: http://nhg.artsennet.nl/content/resources/AMGATE_6059_l04_TICH_L230443008 [Accessed 2007 May 9]
Carlberg B, Samjuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet 2004; 364: 1684–9
Farmacotherapeutisch Kompas. College voor zorgverzekeringen: Amstelveen, 2005
Informatorium Medicamentorum. Wetenschappelijk Instituut Nederlandse Apothekers, Den Haag, 2005
Acknowledgements
No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the contents of this study. We gratefully acknowledge the valuable comments of Professor Bruce Psaty while preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teichert, M., de Smet, P.A.G.M., Hofman, A. et al. Discontinuation of β-Blockers and the Risk of Myocardial Infarction in the Elderly. Drug-Safety 30, 541–549 (2007). https://doi.org/10.2165/00002018-200730060-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200730060-00008