Summary
The use of ACE inhibitors in patients with myocardial infarction (MI) has been the subject of several studies conducted during recent years. These studies have demonstrated the capacity of these agents to improve both survival and morbidity of patients with MI.
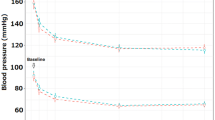
However, the use of ACE inhibitors in patients with MI has been shown to reduce blood pressure (BP) and so could jeopardise the ischaemic myocardium. A significant reduction in systemic BP has been demonstrated by all the studies of ACE inhibitors in patients with MI, but no relationship has been found between the occurrence of hypotension and a worse clinical outcome. An increased risk of death has been observed exclusively in association with severe and sudden hypotension, the occurrence of which can be largely prevented by the administration of the ACE inhibitor according to an increasing dose-titration scheme. Conversely, a certain degree of long term BP reduction could result in some beneficial effect in patients with MI and contribute to the lower incidence of re-infarction observed in patients with acute MI undergoing long term treatment with Captopril.
Since the renin-angiotensin system is strictly related to kidney function, its blockade by an ACE inhibitor could result in some degree of renal dysfunction, particularly in patients with MI and impaired ventricular function. The available results from large-scale studies suggest that abnormalities in kidney function (namely an increase in serum creatinine) are observed in 0.9 to 2.4% of patients with MI who, nevertheless, experience some benefit from treatment with ACE inhibitors. Interestingly, the administration of ACE inhibitors does not seem to further compromise severely impaired renal function, and may also represent a useful tool for the treatment of patients with renal dysfunction associated with MI.
The use of ACE inhibitors in patients with MI is associated with a satisfactory clinical and laboratory safety profile. The occurrence of significant adverse effects seems to be very low and mainly attributable to a rather modest prevalence of cough (2.4 to 6.8%). Discontinuation of treatment because of biochemical and haematological abnormalities has been observed in less than 1% of treated patients.
Thus, the beneficial effects of ACE inhibitor treatment seem to outweigh safety concerns, thereby reinforcing the role of ACE inhibition as a suitable therapeutic strategy in the treatment of patients with MI.
Similar content being viewed by others
References
Jeremy RW, Allman KC, Bautovitch G, et al. Patterns of ventricular dilatation during the six months after myocardial infarction. J Am Coll Cardiol 1989; 13: 304–10
Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction: experimental observations and clinical implications. Circulation 1990; 81: 1161–72
Lamas GA. Left ventricular dilatation following myocardial infarction: clinical course and potential for therapy. Cardiology 1989; 76: 112–21
White HD, Norris RM, Brown MA, et al. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation 1987; 76: 44–51
Yusuf S, Sleight P, Held P, et al. Routine medical management of acute myocardial infarction: lessons from overviews of recent randomized controlled trials. Circulation 1990; 82 (3 Suppl.): II117–34
McAlpine HM, Morton JJ, Leckie B, et al. Neuroendocrine activation after acute myocardial infarction. Br Heart J 1988; 60: 117–24
Sigurdsson A, Held P, Swedberg K. Short- and long-term neurohumoral activation following acute myocardial infarction. Am Heart J 1993; 126: 1068–76
Sigurdsson A, Held P, Swedberg K, et al. Neurohumoral effects of early treatment with enalapril after acute myocardial infarction and the impact on left ventricular remodeling. Eur Heart J 1993; 14: 1110–7
Tan LB, Jalil JE, Pick R, et al. Cardiac myocyte necrosis induced by angiotensin II. Circ Res 1991; 69: 1185–95
Borghi C, Ambrosioni E. Clinical aspects of ACE-inhibition in patients with acute myocardial infarction. Prim Cardiol. In press
Tan LB, Ball SG. ACE-inhibition after myocardial infarction. London: Science Press, 1994
Clough DP, Collis MG, Conway J, et al. Interaction of angiotensin-converting enzyme inhibitors with the function of the sympathetic nervous system. Am J Cardiol 1982; 49: 1410–4
Westlin W, Mullane K. Does Captopril attenuate reperfusion-induced myocardial dysfunction by scavenging free radicals? Circulation 1988; 77 (6 Pt 2): 130–9
Wright R, Flapan AD, Simpson CC, et al. Effects of Captopril on endogenous fibrinolysis in patients with recent myocardial infarction. A double-blind randomised placebo controlled cross-over study [abstract]. J Am Coll Cardiol 1994; 484A
Someya N, Morotomi Y, Kodama K, et al. Suppressive effect of Captopril on platelet aggregation in essential hypertension. J Cardiovasc Pharmacol 1984; 6: 840–3
de Graeff PA, de Langen CDJ, Bel K, et al. Protective effects of Captopril against ischemia/reperfusion-induced ventricular arrhythmias in vitro and in vivo. Am J Med 1988; 84Suppl. 3A: 67
Francis GS. Neuroendocrine activity in congestive heart failure. Am J Cardiol 1990; 66: 33D–39D
Scharper W, Pasyk S. Influence of collateral flow on the ischemic tolerance of the heart following acute and subacute occlusion. Circulation 1976; 66: 1143–9
Pfeffer MA, Braunwald E, Moyè LA, et al. Effect of Captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 1992; 327: 669–77
The AIRE Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 1993; 342: 821–8
Swedberg K, Held P, Kjekshus J, et al. Effect of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med 1992; 327: 678–84
The GISSI-3 Investigators. Effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet 1994; 343: 1115–22
ISIS-4 Collaborative group. ISIS-4: a randomised factorial trial assessing early oral Captopril, oral mononitrate, and intravenous magnesium sulphate in 58050 patients with suspected acute myocardial. Lancet 1995; 345: 669–85
Ambrosioni E, Borghi C, Magnani B, on behalf of the SMILE Study Investigators. The effect of the angiotensin-convertingenzyme inhibitor zofenopril on mortality and morbidity after anterior myocardial infarction. N Engl J Med 1995: 332; 80–5
Chinese Cardiac Study Collaberative Group. Oral Captopril versus placebo among 13634 patients with suspected acute myocardial infarction: interim report from the Chinese Cardiac Study (CCS-1). Lancet 1995; 345: 686–7
Oldroyd KG, Pye MP, Ray SG, et al. Effects of early Captopril administration on infarct expansion, left ventricular remodeling, and exercise capacity after acute myocardial infarction. Am J Cardiol 1991; 68: 713–8
Fiather M, Pipilis A, Collins R, et al. Randomised controlled trial of oral Captopril, of oral isosorbide mononitrate and of intravenous magnesium sulphate started early in acute myocardial infarction: safety and hemodynamic effects. Eur Heart J 1994; 15: 608–19
Latini R, Avanzini F, De Nicolao A, et al. Effects of lisinopril and nitroglicerin on blood pressure early after myocardial infarction: the GISSI 3 pilot study. Clin Pharmacol Ther 1995; 56 (6 Pt 1): 680–92
Kingma JH, van Gilst WH, Peels CH, et al. Acute intervention with Captopril during thrombolysis in patients with first anterior myocardial infarction. Results from the CATS Study. Eur Heart J 1994; 15: 898–907
Ambrosioni E, Borghi C, Magnani B. Early treatment of acute myocardial infarction with angiotensin-converting enzyme inhibition: safety considerations. SMILE Pilot Study Working Party. Am J Cardiol 1991; 68: 101D–110D
Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991; 325: 303–10
The SOLVD Investigators. Effect of enalapril on mortality and development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992; 327: 685–91
The CONSENSUS Trial Study Group. Effect of enalapril on mortality in severe congestive heart failure: results of the Cooperative North Scandinavian Enalapril Survival Study. N Engl J Med 1987; 316: 1429–35
Kober L, Torp-Pederson C, Carlsen JE, et al. A clinical trial of the angiotensin-converting enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 1995; 333: 1670–6.
Wollert KC, Studer R, Just H, et al. Influence of lisinopril on long-term mortality in rats with chronic MI. Role of blood pressure reduction and tissue ACE-inhibition [abstract]. J Am Coll Cardiol 1994; 1A: 484A
MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke and coronary heart disease. Part 1. Lancet 1990: 335; 765–74
Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke and coronary heart disease. Part 2. Lancet 1990: 335; 827–38
Tranchesi B, Santos RD, Caramelli B, et al. Early administration of Captopril and nitroglycerin in combination after acute myocardial infarction: an invasive hemodynamic study. Eur Heart J 1993; 14: 90–5
Seidin DW, Giebish D, editors. The kidney: physiology and pathophysiology. New York: Raven Press, 1992: 1455–504
Schunkert H. Evidence for tissue-specific activation of renal angiotensinogen m-RNA expression in chronic stable experimental heart failure. J Clin Invest 1992; 90: 1523–9
Latini R. Renal effects of lisinopril after myocardial infarction. Results from GISSI-3 trial[abstract]. Eur Heart J 1994; 15: 429: 2258
Sica DA, Cutler RE, Parmer RJ, et al. Comparison of the steady state pharmacokinetics of fosinopril, lisinopril and enalapril in patients with chronic renal insufficiency. Clin Pharmacokinet 1991; 20: 420–7
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Borghi, C., Ambrosioni, E. A Risk-Benefit Assessment of ACE Inhibitor Therapy Post-Myocardial Infarction. Drug-Safety 14, 277–287 (1996). https://doi.org/10.2165/00002018-199614050-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-199614050-00002