Abstract
Synopsis
Ramipril is a second generation angiotensin converting enzyme (ACE) inhibitor. Like enalapril, it is a prodrug and is hydrolysed in vivo to release the active metabolite, ramiprilat, which has a long elimination half-life, permitting once-daily administration.
The antihypertensive efficacy of ramipril has been confirmed in large-scale noncomparative studies conducted in general practice as well as in more rigorously controlled clinical trials. In the former, approximately 85% of patients with mild to moderate essential hypertension have responded successfully to treatment with ramipril 2.5 or 5 mg/day, while comparative trials indicate that the antihypertensive efficacy of the drug is equivalent to that of other established ACE inhibitors and the β-adrenoceptor antagonist atenolol. As expected, the response rate to ramipril monotherapy is lower in patients with severe hypertension (around 40%), although the blood pressure lowering effect can be enhanced with the addition of a diuretic such as hydrochlorothiazide or piretanide. The antihypertensive efficacy of ramipril is maintained in patients with diabetes mellitus and preliminary data indicate that the drug has the beneficial effect of decreasing urinary albumin excretion in diabetic patients with nephropathy. Ramipril is superior to atenolol in causing regression of left ventricular hypertrophy, although the clinical significance of this effect per se remains to be established.
The large-scale Acute Infarction Ramipril Efficacy (AIRE) study demonstrated that ramipril 5 or 10 mg/day significantly decreased the risk of all-cause mortality by 27% in patients with clinical evidence of heart failure after acute myocardial infarction, even if transient. The beneficial effect of ramipril was apparent by 30 days of treatment and appeared to be greatest in patients with more severe ventricular damage after infarction.
Ramipril is well tolerated in general practice, with 5% or fewer patients discontinuing therapy because of drug intolerance. The data available suggest that ramipril shares a similar tolerability profile to that of other established ACE inhibitors.
Thus, clinical data confirm ramipril as a useful alternative ACE inhibitor for the treatment of patients with mild to moderate hypertension, and indicate a beneficial effect of the drug inpatients with clinical evidence of heart failure after acute myocardial infarction. It is also reasonable to assume that ramipril will be of value in the treatment of patients with more established heart failure or asymptomatic left ventricular dysfunction.
Pharmacodynamic Properties
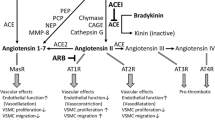
Ramipril is a prodrug designed to improve the systemic bioavailability of the active angiotensin converting enzyme (ACE) inhibitor, ramiprilat. Most data support the hypothesis that the beneficial haemodynamic effects of ramiprilat result from decreased angiotensin II formation, which, in turn, decreases vasopressor activity and peripheral vascular resistance. Moreover, evidence is accumulating that local inhibition of ACE and angiotensin II formation in specific target tissues such as the vascular wall may in some way be involved in the haemodynamic effects of ramipril. ACE inhibition potentiates endogenous bradykinin levels, which may contribute to 2 potentially beneficial cardiac effects observed with these agents, namely regression of left ventricular hypertrophy and a cardioprotective effect on the ischaemic myocardium.
When administered to patients with essential hypertension, a single oral dose of ramipril 2.5 to 20mg decreased systolic and diastolic blood pressure in a dose-dependent manner without affecting the normal circadian variation in blood pressure or heart rate. The antihypertensive response was maximal at 4 to 8 hours and was still apparent at 24 hours after dosing. In patients with moderate to severe congestive heart failure, a single oral dose of ramipril 5 or 10mg had the beneficial effect of decreasing preload and afterload with a reflex increase in cardiac output.
The effect of ramipril on renal blood flow in hypertensive patients with normal kidney function has been variable, but with no indication of a negative effect. Like other ACE inhibitors, ramipril has the beneficial action of reducing the urinary albumin excretion rate in diabetic patients with nephropathy. Short term, significant improvements in glucose tolerance and insulin sensitivity have been documented in elderly insulin-resistant patients with mild hypertension treated with ramipril.
Pharmacokinetic Properties
More than 55% of an oral dose of ramipril is absorbed and bioavailability is unaffected by the presence of food. Once absorbed, ramipril is rapidly de-esterified to form the active metabolite ramiprilat; peak plasma concentrations of the parent drug and ramiprilat are reached in about 1 and 3 hours, respectively. De-esterification takes place primarily in the liver. Ramiprilat has an extended terminal elimination phase lasting 110 hours which is due to slow dissociation from its binding site on ACE. However, significant accumulation of the parent drug or ramiprilat has not been observed after 2 weeks’ administration of therapeutic dosages of ramipril in healthy volunteers.
Renal excretion is the main route of elimination of the parent drug and ramiprilat and their respective metabolites. Approximately 60% of a single oral dose of ramipril is recovered in the urine, while the remaining 40% is recovered in the faeces and includes biliary excretion.
Plasma concentrations of ramiprilat are increased in the elderly and patients with renal or heart failure, while those of the parent drug are potentiated in patients with hepatic impairment. Accordingly, low initial dosages and/or dosage reductions of ramipril are likely to be necessary in these special patient populations.
Therapeutic Efficacy
In noncomparative studies conducted in general practice, approximately 85% of patients with mild to moderate essential hypertension responded successfully to 6 to 8 weeks’ treatment with ramipril 2.5 or 5 mg/day; that is, diastolic blood pressure was controlled at ≤90 to 95mm Hg or reduced by >10mm Hg from baseline. The response rate declined with increasing severity of hypertension, although it was similar in men and women, as well as in young and older (>65 years) patients. After 2 years, ramipril monotherapy continued to be effective in more than 90% of patients who responded successfully to short term treatment with the drug.
Large-scale double-blind multicentre studies have demonstrated that the antihypertensive efficacy of ramipril is comparable to that of enalapril, Captopril, lisinopril and atenolol, while combination therapy with ramipril plus hydrochlorothiazide or piretanide was generally superior to monotherapy with either agent alone at the same dose. In terms of providing blood pressure reduction, the optimum combinations evaluated have been ramipril 5mg/hydrochlorothiazide 25mg and ramipril 5mg/piretanide 6mg.
In placebo-controlled studies, once daily administration of ramipril 2.5 to 20mg for 3 months achieved target blood pressure in over 50% of diabetic patients with mild to moderate hypertension, without adversely affecting plasma glucose and lipid levels. Moreover, the drug significantly decreased the urinary albumin excretion rate in diabetic patients with nephropathy. Ramipril reduced left ventricular hypertrophy to a greater extent than atenolol, although the clinical significance of this effect per se remains to be determined. Available data suggest that ramipril effectively lowers blood pressure in patients with renal insufficiency, although drug dosage should be modified in accordance with the degree of renal impairment.
Ramipril increases exercise duration and improves the status of patients with established congestive heart failure. In the large-scale Acute Infarction Ramipril Efficacy (AIRE) study, patients with clinical evidence of heart failure after acute myocardial infarction (MI), even if transient, were randomised to receive ramipril 5 or 10 mg/day or placebo (n = 1986). Ramipril was initiated between day 3 and day 10 after MI and continued for ≥6 (mean 15) months. An intention-to-treat analysis revealed that ramipril significantly decreased the risk of all-cause mortality by 27% and the combined incidence of prespecified secondary outcomes (i.e. first validated event in an individual patient, namely death, progression to severe/resistant heart failure, reinfarction or stroke) by 19% compared with placebo. A near-significant 29% reduction in the risk of all-cause mortality was apparent within 30 days of initiating ramipril therapy. Most patients benefited from treatment with ramipril, although the effect was less pronounced in younger patients (>65 years) and those not receiving concomitant diuretic therapy.
Tolerability
Ramipril has been well tolerated by hypertensive patients during short term treatment and maintenance therapy for up to 2 years. Adverse events are usually mild and transient and only rarely severe enough to necessitate withdrawal of ramipril in general practice (≤5% of patients). In the AIRE study, the number of patients with heart failure after MI who withdrew because of drug intolerance was higher for ramipril than for placebo (12.5 vs 7%).
Adverse events, regardless of causality to ramipril, have been reported in 9% of patients with essential hypertension enrolled in a large-scale general practice study based in Austria (n = 5193). Dry cough occurred in fewer than 1% of patients, while the other most commonly reported adverse events included headache and dizziness/vertigo which are expected to occur in a small proportion of patients taking oral medication.
Ramipril appears to be equally well tolerated by young and elderly patients (>65 years) with mild to moderate essential hypertension. Moreover, the drug has little effect on standard laboratory test values and can be administered to diabetic patients without adversely affecting the cardiovascular risk profile. As for all ACE inhibitors, caution is advised if ramipril is to be used in combination with a potassium-sparing diuretic, since hyperkalaemia may result.
Available data suggest that the tolerability profile of ramipril is similar to that of other available ACE inhibitors, although the impact of the drug on quality of life in patients with hypertension remains to be established.
Dosage and Administration
In the treatment of mild to moderate essential hypertension, the initial recommended oral dose of ramipril is normally 2.5mg once daily. However, a lower dosage of 1.25 mg/day should be initiated in patients already receiving a diuretic, thereby reducing the risk of symptomatic hypotension. The dosage should be titrated according to the blood pressure response, and the usual maintenance dosage is 2.5 or 5 mg/day (maximum 10 mg/day). Twice daily administration is advised for patients in whom it is suspected that the antihypertensive effect of ramipril diminishes towards the end of a once daily dosage interval.
The recommended starting dose in patients with renal impairment (creatinine clearance >3 L/h/1.73m ) is 1.25mg, titrated up to a maximum of 5 mg/day. Dosages at the lower end of the therapeutic spectrum are also likely to be required in elderly patients and those with hepatic impairment. Patients with clinical evidence of heart failure following acute MI should receive an initial dosage of ramipril 2.5 mg/day titrated upwards to 5 or 10 mg/day, regardless of whether they are already receiving diuretics. In the event of poor tolerability, a lower dosage of 2.5 mg/day can be given for 2 days, followed by re-titration upwards if appropriate.
Similar content being viewed by others
References
Todd PA, Benfield P. Ramipril: a review of its pharmacological properties and therapeutic efficacy in cardiovascular disorders. Drugs 1990; 39: 110–35
Todd PA, Goa KL. Enalapril: a reappraisal of its pharmacology and therapeutic use in hypertension. Drugs 1992; 43: 346–81
Rosenthal J, Buehler G, Koenig W, et al. Effect of angiotensin-converting enzyme inhibition on human tissue renin. J Car-diovasc Pharmacol 1991; 18 Suppl. 2: 122–4
Erman A, Winkler J, Chen-Gal B, et al. Inhibition of angiotensin converting enzyme by ramipril in serum and tissue of man. J Hypertens 1991; 9: 1057–62
Vago T, Bevilacqua M, Conci F, et al. Angiotensin converting enzyme binding sites in human heart and lung: comparison with rat tissues. Br J Pharmacol 1992; 107: 821–5
Bönner G, Preis S, Schunk U, et al. Effect of bradykinin on arteries and veins in systemic and pulmonary circulation. J Cardiovasc Pharmacol 1992; 20 Suppl 9: S21–7
Linz W, Wiemer G, Schölkens BA. Contribution of bradykinin to the cardiovascular effects of ramipril. J Cardiovasc Pharmacol 1993; 22 Suppl. 9: S1–8
de Leeuw PW, Lugtenberg PL, van Houten H, et al. Preliminary experiences with HOE 498, a novel long-acting converting enzyme inhibitor, in hypertensive patients. J Cardiovasc Pharmacol 1985; 7: 1161–5
Kostis JB. Double-blind study of ascending doses of ramipril in patients with mild to moderate hypertension. Adv Ther 1991; 8: 6–17
McCarron D, Ramipril MSG. 24-Hour blood pressure profiles in hypertensive patients administered ramipril or placebo once daily: magnitude and duration of antihypertensive effects. Clin Cardiol 1991; 14: 737–42
Spieker C, Zidek W, Vetter H, et al. Ambulatory 24-h blood pressure monitoring in essential hypertensives treated with the angiotensin-converting enzyme inhibitor ramipril. J Int Med Res 1991; 19: 39–43
Burris JF. Lessons learned with ambulatory blood pressure monitoring: a focus on ramipril. Clin Ther 1993; 15: 476–85
Karlberg BE, Lindström T, Rosenqvist U, et al. Efficacy, tolerance and hormonal effects of a new oral angiotensin converting enzyme inhibitor, ramipril (HOE 498), in mild to moderateessentialhypertension. AmJCardiol 1987; 59: 104–9D
Wenting GJ, Blankestijn PJ, Poldermans D, et al. Blood pressure response of nephrectomised subjects and patients with essential hypertension to ramipril: indirect evidence that inhibition of tissue angiotensin converting enzyme is important. Am J Cardiol 1987; 59: 92–7D
de Graeff PA, Kingma JH, Dunselman PHJM, et al. Acute hemodynamic and hormonal effects of ramipril in chronic congestive heart failure and comparison with Captopril. Am J Cardiol 1987; 59: 164–70D
Beerman B, Nyquist O, Höglund C, et al. Haemodynamic effects, ACE inhibition and pharmacokinetics in patients with heart failure. Eur J Clin Pharmacol 1993; 45: 241–6
Lonn EM, Yusuf S, Jha P, et al. Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation 1994; 90: 2056–69
Przyklenk K, Kloner RA. “Cardioprotection” by ACE-inhibitors in acute myocardial ischemia and infarction. Basic Res Cardiol 1993; 88 Suppl. 1: 139–54
Zughaib ME, Sun JZ, Bolli R. Effect of angiotensin-converting enzyme inhibitors on myocardial ischemia/reperfusion injury: an overview. Basic Res Cardiol 1993; 88 Suppl. 1: 155–67
Juggi JS, Koenig-Berard E, Van-Gilst WH. Cardioprotection by angiotensin-converting enzyme (ACE) inhibitors. Can J Cardiol 1993; 9: 336–52
Gavras H, Gavras I. Cardioprotective potential of angiotensin converting enzyme inhibitors. J Hypertens 1991; 9: 385–92
Dominiak P. Modulation of sympathetic control by ACE inhibitors. Eur Heart J 1993 Nov; 14 Suppl. 1: 169–72
Finta KM, Fischer MJ, Lee L, et al. Ramipril prevents impaired endothelium-dependent relaxation in arteries from rabbits fed an atherogenic diet. Atherosclerosis 1993; 100: 149–56
Riezebos J, Vleeming W, Beems RB, et al. Comparison of the antiatherogenic effects of isradipine and ramipril in cholesterol-fed rabbits: I. Effect on progression of atherosclerosis and endothelial dysfunction. J Cardiovasc Pharmacol 1994; 23: 415–23
Riezebos J, Vleeming W, Beems RB, et al. Comparison of the antiatherogenic effects of isradipine and ramipril in cholesterol-fed rabbits: II. Effect on regression of atherosclerosis and restoration of endothelial function. J Cardiovasc Pharmacol 1994; 23: 424–31
Sharpe N. The effects of ACE inhibition on progression of atherosclerosis. J Cardiovasc Pharmacol 1993; 22 Suppl. 9: S9–12
Ram CVS, Lugo CE, Tinsley RL, et al. Systemic and renal hemodynamic effects of ACE inhibition with ramipril in patients with essential hypertension [abstract]. J Hypertens 1994 Mar; 12 Suppl. 3: 44
Moiseyev VS, Ivleva AJ, Antija ID, et al. Cardiovascular and renal effects of ramipril [Letter]. Lancet 1989; 1: 846
Crozier IG, Ikram H, Nicholls MG, et al. Global and regional hemodynamic effects of ramipril in congestive heart failure. J Cardiovasc Pharmacol 1989; 14: 688–93
Marre M, Hallab M, Billiard A, et al. Small doses of ramipril to reduce microalbuminuria in diabetic patients with incipient nephrophathy independently of blood pressure changes. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S165–168
Chonko A, Donaldson D, Moore W, et al. Ramipril has an anti-proteinuric effect and maintains renal function in patients with type I diabetes mellitus: a prospective double-blind dose finding trial [abstract no 656A]. Clin Res 1993; 41 Suppl
Orrasch. Effect of low-dose ACE-inhibitor (ramipril) on microalbuminuria in the non-insulin dependent diabetic patient [abstract; In Italian]. G Diabetol 1994; 14: 79
Kasiske BL, Kalil RSN, Ma JZ, et al. Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Ann Intern Med 1993; 118: 129–38
Jungmann E, Krüger K, Semler B, et al. Nephroprotective effect of ramipril. Impact of blood pressure and metabolic control in patients with insulin-dependent diabetes [in German]. Fortschr Med 1994; 112: 39–42
Erley CM, Haefele U, Heyne N, et al. Microalbuminuria in essential hypertension: reduction by different antihypertensive drugs. Hypertension 1993; 21: 810–5
Keilani T, Schlueter WA, Kaplan B, et al. Therapeutic advantage of low dose angiotensin converting enzyme (ACE) inhibition for patients with proteinuria and renal impairment [abstract]. Clin Res 1994; 42: 222A
Heintz B, Verho M, Brockmeier D, et al. Influence of ramipril on renal function in patients with chronic congestive heart failure. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S174–179
Bönner G, Döring R, Baumanns J, et al. Endogenous kinins mediate the acute effects of ACE inhibitors on glucose metabolism [abstract no. 1046]. J Hypertens 1994; 13 Suppl. 3: S190
Paolisso G, Gambardella A, Verza M, et al. ACE inhibition improves insulin-sensitivity in aged insulin-resistant hypertensive patients. J Hum Hypertens 1992; 6: 175–9
Ludvik B, Kueenburg E, Brunnbauer M, et al. The effects of ramipril on glucose tolerance, insulin secretion, and insulin sensitivity in patients with hypertension. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S157–159
Heintz B, Verho M, Brockmeier D, et al. Multiple-dose pharmacokinetics of ramipril in patients with chronic congestive heart failure. J Cardiovasc Pharmacol 1993; 22 Suppl. 9: S36–42
Hosie J, Meredith P. The pharmacokinetics of ramipril in a group of ten elderly patients with essential hypertension. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: 125–7
Eckert HG, Badian MJ, Gantz D, et al. Pharmacokinetics and biotransformation of 2-[N-[(S)-1-ethoxycarbonyl-3-phenyl-propyl]-L-alanyl]-(lS,3S,5S)-2-azabicyclo [3.3.0] octane-3-carboxylic acid (Hoe 498) in rat, dog and man. Arzneimittel Forschung 1984; 34: 1435–47
Ball SG, Robertson JIS. Clinical pharmacology of ramipril. Am J Cardiol 1987; 59: 23–7D
Hoechst-Roussel Pharmaceuticals Inc. Drug reference/prescribing information. New Jersey, US, 1992.
Manhem PJO, Ball SG, Morton JJ, et al. A dose-response study of HOE 498, a new non-sulphydryl converting enzyme inhibitor, on blood pressure, pulse rate and the renin-angiotensin-aldosterone system in normal man. Br J Clin Pharmacol 1985; 20: 27–35
Luck C, Verho M, Umscheid T, et al. Preliminary results of biliary excretion of ramipril after T-drainage in cholecystectomy patients. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S116–121
Schunkert H, Kindler J, Gassmann M, et al. Pharmacokinetics of ramipril in hypertensive patients with renal insufficiency. Eur J Clin Pharmacol 1989; 37: 249–56
Kelly JG, O’Malley K. Clinical pharmacokinetics of the newer ACE inhibitors. A review. Clin Pharmacokinet 1990; 19: 177–96
Begg EJ, Bailey RR, Lynn KL, et al. The pharmacokinetics of angiotensin converting enzyme inhibitors in patients with renal impairment. J Hypertens 1989; 7 Suppl. 5: S29–32
Gerckens U, Grube E, Mengden T, et al. Pharmacokinetic and pharmacodynamic properties of ramipril in patients with congestive heart failure (NYHA III–IV). J Cardiovasc Pharmacol 1989; 13 Suppl 3: S49–51
Meyer BH, Muller O, Badian M, et al. Pharmacokinetics of ramipril in the elderly. Am J Cardiol 1987; 59: 33–7D
Gilchrist WJ, Beard K, Manhem P, et al. Pharmacokinetics and effects on the renin-angiotensin system of ramipril in elderly patients. Am J Cardiol 1987; 59: 28–32D
Reinisch W, Hoffmann H, Hoffmann W. Hypertension treatment with ramipril: results of a prospective clinical study [in German]. Ther Schweiz 1993; 9: 655–9
Brandt D. Therapie der arteriellen hypertonic mit dem ACE-hemmer ramipril: ergebnisse der Ostereichischen multicen-ter-ramipril-studie (ART1). Therapiewoche Osterreich 1992; 7: 394–400
Carré A, Zannad F, Vasmant D. The French multicentre study of ramipril in ambulatory patients with mild-to-moderate hypertension. Clin Physiol Biochem 1992; 9: 105–12
Kaplan NM, Sproul LE, Mulcahy WS. Large prospective study of ramipril in patients with hypertension. Clin Ther 1993; 15: 810–8
Lederle RM, Klaus D, Verho M, et al. Ramipril. A novel angiotensin-converting enzyme inhibitor in the treatment of severe, refractory hypertension [in German]. Munch Med Wochenschr 1991; 133: 394–6
Predel H-G, Düsing R, Bäcker A, et al. Combined treatment of severe essential hypertension with the new angiotensin converting enzyme inhibitor ramipril. Am J Cardiol 1987; 59: 143–8D
Delix® bei Hypertonic Data on file, Hoechst AG, Germany.
Saalbach R, Wochnik G, Mauersberger H, et al. Antihypertensive efficacy, tolerance, and safety of ramipril in young vs. old patients: a retrospective study. J Cardiovasc Pharmacol 1991; 18 Suppl 2: S134–6
Lonati L, Sampieri L, Cuspidi C. Efficacy and safety of ramipril in elderly hypertensive patients: a multicenter trial, [abstract] Presented at: IFECC III International Forum for the Evaluation of Cardiovascular Care, Monte Carlo, January 19–22, 1994.
Schreiner M, Berendes B, Verho M, et al. Antihypertensive efficacy, tolerance, and safety of long-term treatment with ramipril in patients with mild-to-moderate essential hypertension. J Cardiovasc Pharmacol 1991; 18 Suppl 2: S137–40
Koenig W, Feldmann M, Krohn J, et al. Ramipril vs lisinopril in the treatment of mild to moderate primary hypertension — a randomised double-blind multicentre trial. Drug Invest 1992; 4(5): 450–7
Nami R, Pavese G, Panza F, et al. Comparative evaluation of the antihypertensive effect and the tolerability of different ACE inhibitors in the medium term treatment of essential hypertension [in Italian]. G Ital Ric Clin Ter 1992; 13: 107–16
Ruddy MC, Mroczek WJ. Comparison of ramipril and enalapril in patients with essential hypertension. Pharmacotherapy 1993; 13: 224–8
Witte PU, Walter U. Comparative double-blind study of ramipril and Captopril in mild to moderate essential hypertension. Am J Cardiol 1987; 59: 115–20D
Yajnik VH, Vatsraj DJ, Acharya HK, et al. Ramipril vs Captopril in mild to moderate hypertension. Journal of the Association of Physicians in India 1994; 42: 120–3
Zabludowski J, Rosenfeld J, Akbary MA, et al. A multi-centre comparative study between ramipril and enalapril in patients with mild to moderate essential hypertension. Curr Med Res Opin 1988; 11: 93–106
Modesti PA, Said AM, Cecioni I, et al. Twenty-four-hour antihypertensive efficacy of ramipril and enalapril. Curr Ther Res 1993; 53: 137–43
Grandinetti O, Cosentino G, Feraco E. Lisinopril versus ramipril: efficacy and safety in elderly hypertensives with non-insulin dependent diabetes mellitus [abstract]. J Hypertens 1992 Jun; 10 Suppl. 4: 222
Mohiuddin SM, Gannon JM, Hilleman DE. Sustained effects of ACE inhibitors on ambulatory blood pressure in mild to moderate hypertension: ramipril versus enalapril. South Med J 1993; 86: S136
Zannad F. Trandolapril: how does it differ from other angiotensin converting enzyme inhibitors? Drugs 1993; 46 Suppl. 2: 172–82
Meredith PA. Trough/peak ratios for antihypertensive agents: the issues in perspective. Drugs 1994; 48: 661–6
Meredith PA, Elliot HL. FDA guidelines on trough: peak ratios in the evaluation of antihypertensive agents. J Cardiovasc Pharmacol 1994; 24 Suppl. 5: S26–30
Vasmant D, Lendresse P, Lemarie J-C, et al. Comparison of response rates to the angiotensin-converting enzyme inhibitor ramipril in mild-to-moderate hypertension in a double-blind, parallel-group study and an open single-blind study. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S144–146
Genthon R, and the ATHES study group. Study of the efficacy and safety of the combination ramipril 2.5 mg plus hydrochlorothiazide 12.5 mg in patients with mild-to-moderate hypertension. Int J Clin Pharmacol Res 1994; 14: 1–9
Heidbreder D, Froer K-L, Breitstadt A, et al. Combination of ramipril and hydrochlorothiazide in the treatment of mild to moderate hypertension: Part 1 — a double-blind, comparative, multicenter study in nonresponders to ramipril monotherapy. Clin Cardiol 1992; 15: 904–10
Scholze J, Breitstadt A, Cairns V, et al. Short report: ramipril and hydrochlorothiazide combination therapy in hypertension: a clinical trial of factorial design. J Hypertens 1993; 11: 217–21
Amery A, Kiowski W, Löffler K, et al. Double-blind comparison of ramipril, piretanide and the combined therapy in hypertensive patients [abstract]. J Hypertens 1994 Mar; 12 Suppl. 3: 131
Lenox-Smith AJ, Street RB, Kendall FD. Comparison of ramipril against atenolol in controlling mild-to-moderate hypertension. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S150–152
Weidmann P, Frank J, Graf W, et al. Monotherapy with the ACE inhibitor ramipril or the calcium antagonist nitrendipine in essential hypertension [in German]. Schweiz Med Wochenschr 1992; 122: 1497–503
Perticone F, Pugliese F, Ceravolo R, et al. Amlodipine versus ramipril in the treatment of hypertension of mild to moderate hypertension: evaluation by 24-hour ambulatory blood pressure monitoring. Cardiology 1994; 85: 36–46
Kundu SC, Bhattacharya A, Vakil HB. Ramipril and methyl-dopa compared in patients with mild to moderate hypertension. Clin Ther 1990; 12: 393–7
Townsend RR, Holland OB. Combination of converting enzyme inhibitor with diuretic for the treatment of hypertension. Arch Intern Med 1990; 150: 1173–83
Homuth V, Faulhaber H-D, Loose U. Usefulness of piretanide plus ramipril for systemic hypertension: a multicenter trial. Am J Cardiol 1993; 72: 666–71
Bainbridge AD, MacFadyen RJ, Stark S, et al. The antihypertensive efficacy and tolerability of a low dose combination of ramipril and felodipine ER in mild to moderate essential hypertension. Br J Clin Pharmacol 1993; 36: 323–30
Lüders S, Schrader J, Scheler F. Combined treatment of primary hypertension with ACE-inhibitors and β-blockers [in German]. Nieren Hoch 1992; 21: 677–9
Baba T, Ishizaki T. Recent advances in pharmacological management of hypertension in diabetic patients with nephropathy: effects of antihypertensive drugs on kidney function and insulin sensitivity. Drugs 1992; 43: 464–89
Schwartz SL, Hanson C, Lucas C, et al. Double-blind, placebocontrolled study of ramipril in diabetics with mild to moderate hypertension. Clin Ther 1993; 15: 79–87
Erhard W, Lindner U, Krall H, et al. Assessment of the efficacy, tolerance, and safety of ramipril in diabetic patients with mild-to-moderate hypertension: a retrospective analysis. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S160–164
Pedersen MM, Hansen KW, Schmitz A, et al. Effects of ACE inhibition supplementary to beta-blockers and diuretics in early diabetic nephropathy. Kidney Int 1992; 41: 883–90
Tettamanti F, Zoppi A, Malamani GD, et al. Effects of ramipril and nitrendipine on proteinuria in hypertensive patients with albuminuric NIDDM [abstract]. J Hypertens 1992 Jun; 10 Suppl. 4: 102
Schernthaner G, Schnack C, Hopmeier P. Effect of ramipril or atenolol on microalbuminuria and metabolic control parameters in type-2 diabetes mellitus, [abstract no. 752] Presented at 30th Annual Meeting of the European Association for the study of Diabetes, Düsseldorf, 1994: A195.
Kindler J, Schunkert H, Gassmann M, et al. Therapeutic efficacy and tolerance of ramipril in hypertensive patients with renal failure. J Cardiovasc Pharmacol 1989; 13 Suppl 3: S55–8
Lavie CJ, Ventura HO, Messerli FH. Regression of increased left ventricular mass by antihypertensives. Drugs 1991; 42: 945–61
Eichstädt HW, Felix R, Langer M, et al. Use of nuclear magnetic resonance imaging to show regression of hypertrophy with ramipril treatment. Am J Cardiol 1987; 59: 98–103D
Lievre M, Gueret P, Delair S, et al. ACE-inhibitor-induced reduction in left ventricular mass independent of changes in blood pressure in hypertensive patients with left ventricular hypertrophy [abstract]. Hypertension 1993; 22: 419
Agabiti-Rosei E, Ambrosioni E, Dal Palu C, et al. Is ACE inhibition more effective than β-blockade in reducing hypertensive cardiac hypertrophy [abstract no. 1785]. Eur Heart J 1994; 15: 338
Boissel J-P, Lievre M, Guéret P, et al. The trial of low and regular dose of ramipril on regression of left ventricular hypertrophy in hypertensive patients: the HYCAR Study. In: Unger T, Albrechts C, Ball SG, editors. ACE inhibitors and high risk patients. Haslemere: Euromed Communications Ltd, 1994: 37-49
Yusuf S, Garg R, McConachie D. Effect of angiotensin-converting enzyme inhibitors in left ventricular dysfunction: results of studies of left ventricular dysfunction in the context of other similar trials. J Cardiovasc Pharmacol 1993; 22 Suppl. 9: S28–35
Cohn JN, Johnson G, Ziesche S, et al. Acomparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med 1991; 325: 303–10
de Graeff PA, Kingma JH, Viersma JW, et al. Acute and chronic effects of ramipril and Captopril in congestive heart failure. Int J Cardiol 1989; 23: 59–67
Manthey J, Osterziel KJ, Röhrig N, et al. Ramipril and Captopril in patients with heart failure: effects on haemodynamics and vasoconstrictor systems. Am J Cardiol 1987; 59: 171–5D
Kholeif MA, Pringle S, Kesson E, et al. A comparison of the efficacy and safety of ramipril and digoxin added to maintenance diuretic treatment in patients with chronic heart failure. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S180–183
Sigurdsson A, Swedberg K, Ullman B. Effects of ramipril on the neurohormonal response to exercise in patients with mild or moderate congestive heart failure. Eur Heart J 1994; 15: 247–54
Sigurdsson A, Amtorp O, Gundersen T, et al. Neurohormonal activation in patients with mild or moderately severe congestive heart failure and effects of ramipril. Br Heart J 1994; 72: 422–7
Cohn JN, Levine TB, Olivari MT, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984; 311: 819–23
Packer M. The neurohormonal hypothesis: a theory to explain the mechanism of disease progression in heart failure. J Am Coll Cardiol 1992; 20: 248–54
Stevenson R, Ranjadayalan K, Wilkinson P, et al. Short and long term prognosis of acute myocardial infarction since introduction of thrombolysis. BMJ 1993; 307: 349–53
Ertl G. Angiotensin converting enzyme inhibitors in angina and myocardial infarction: what role will they play in the 1990s? Drugs 1993; 46(2): 209–18
Ball SG, Cowan JC, Winter C. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 1993; 342: 821–8
Ball SG, Hall AS, Murray GD. ACE inhibition, atherosclerosis and myocardial infarction — the AIRE Study in practice. Eur Heart J 1994 May; 15 Suppl. B: 20–5
Williams GH. Converting-enzyme inhibitors in the treatment of hypertension. N Engl J Med 1988; 319: 1517–25
Lunde H, Hedner T, Samuelsson O, et al. Dyspnoea, asthma, and bronchospasm in relation to treatment with angiotensin converting enzyme inhibitors. BMJ 1994; 308: 18–21
Simon SR, Black HR, Moser M, et al. Cough and ACE inhibitors. Arch Intern Med 1992; 152: 1698–700
Bauer B, Lorenz H, Zahlten R. An open multicenter study to assess the long-term efficacy, tolerance, and safety of the oral angiotensin converting enzyme inhibitor ramipril in patients with mild to moderate essential hypertension. J Cardiovasc Pharmacol 1989; 13 Suppl 3: S70–4
Carré A, Vasmant D, Elmalem J. Tolerability of ramipril in a multicenter study of mild-to-moderate hypertension in general practice. J Cardiovasc Pharmacol 1991; 18 Suppl. 2: S141–143
Gums JG. Use of ACE inhibitors in the treatment of cardiovascular disease. Am Pharm 1992; NS32: 62–71
Moore N, Noblet C, Joannidés R, et al. Cough and ACE-inhibitors [letter]. Lancet 1993; 341 Suppl. 9: 61
Fletcher AE, Palmer AJ, Bulpitt CJ. Cough with angiotensin converting enzyme inhibitors: how much of a problem? J Hypertens 1994; 12 Suppl. 2: S43–47
Shotan A, Widerhorn J, Hurst A, et al. Risks of angiotensin-converting enzyme inhibition during pregnancy: experimental and clinical evidence, potential mechanisms, and recommendations for use. Am J Med 1994; 96: 451–6
McKenney J. Angiotensin-Converting enzyme inhibitor therapy: practical implications for the pharmacist. Adv Ther 1993; 10: 41–51
van Griensven JM, Seibert-Grafe M, Schoemaker HC, et al. The pharmacokinetic and pharmacodynamic interactions of ramipril with propranolol. Eur J Clin Pharmacol 1993; 45: 255–60
Brogden RN, Todd PA, Sorkin EM. Captopril: an update of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in hypertension and congestive heart failure. Drugs 1988; 36: 540–600
Lancaster SG, Todd PA. Lisinopril: a preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in hypertension and congestive heart failure. Drugs 1988; 35: 646–69
Wadworth AN, Brogden RN. Quinapril: a review of its pharmacological properties, and therapeutic efficacy in cardiovascular disorders. Drugs 1991; 41: 378–99
Todd PA, Fitton A. Perindopril: a review of its pharmacological properties and therapeutic use in cardiovascular disorders. Drugs 1991; 42: 90–114
Murdoch D, McTavish D. Fosinopril: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in essential hypertension. Drugs 1992; 43: 123–40
Balfour JA, Goa KL. Benazapril: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in hypertension and congestive heart failure. Drugs 1991; 42: 511–39
Herman AG. Differences in structure of angiotensin-converting enzyme inhibitors might predict differences in action. Am J Cardiol 1992; 70: 102–8C
Unger T, Gohlke P. Converting enzyme inhibitors in cardiovascular therapy: current status and future potential. Cardiovasc Res 1994; 28: 146–58
Rosenthal T. Drug therapy of renovascular hypertension. Drugs 1993; 45: 895–909
Swales JD. Pharmacological treatment of hypertension. Lancet 1994; 344: 380–5
Dahlöf B, Pennert K, Hansson L. Reversal of left ventricular hypertrophy in hypertensive patients: a metaanalysis of 109 treatment studies. Am J Hypertens 1992; 5: 95–110
Wilson MD, Weart W. Hypertension: are beta-blockers and diuretics appropriate first-line therapies? Ann Pharmacother 1994; 28: 617–25
Lewis EJ, Hunsicker LG, Bain RP, et al. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med 1993; 329: 1456–62
CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med 1987; 316: 1429–35
The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1990; 325: 293–302
The SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992; 327: 685–91
Hall AS, Tan L-P, Ball SG. Inhibition of ACE/kininase-II, acute myocardial infarction, and survival. Cardiovasc Res 1994; 28: 190–8
Ertl G, Gaudron P, Neubauer S, et al. Indication for ACE-inhibitors post-myocardial infarction [in German]. Z Kardiol 1994; 83 Suppl. 4: 65–74
Ray S, Dargie H. Infarct-related heart failure: the choice of ACE-inhibitor does not matter. Cardiovasc Drugs Ther 1994; 8: 433–6
Opie LH. The new trials: AIRE, ISIS-4, and GISSI-3. Is the dossier on ACE inhibitors and myocardial infarction now complete? Cardiovasc Drugs Ther 1994; 8: 469–72
Jha P, Lonn E, Flather M, et al. Rationale for the HOPE (Heart Outcomes Prevention Evaluation) study. In: Unger T, Albrechts C, Ball SG, editors. ACE inhibitors and high risk patients. Haslemere: Euromed Communications Ltd, 1994: 89–103
Frishman WH. Comparative pharmacokinetic and clinical profiles of angiotensin-converting enzyme inhibitors and calcium antagonists in systemic hypertension. Am J Cardiol 1992; 69: 17–25C
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: S.G. Ball, Institute for Cardiovascular Research, University of Leeds, Leeds, England; G. Bönner, Department of Internal Medicine II, University of Cologne, Cologne, Germany; M.J. Cziraky, Department of Pharmacy Practice and Administration, Philadelphia College of Pharmacy & Science, Philadelphia, Pennsylvania, USA; W.H. Irishman, Department of Medicine, Albert Einstein College of Medicine, Bronx, New York, USA; B. Jackson; Department of Medicine, Preston and Northcote Community Hospital, Preston, Victoria, Australia; J. Kostis, Robert Wood Johnson School of Medicine, New Brunswick, New Jersey, USA; H.J. Kramer, Department of Medicine, University of Bonn, Bonn, Germany; G. Paolisso, Department of Geriatric Medicine and Metabolic Diseases, University of Naples, Naples, Italy; D.N. Sharpe, Department of Medicine, University of Auckland, Auckland, New Zealand; H. Thurston, Department of Medicine, Leicester Royal Infirmary, Leicester, England; R.R. Townsend, Renal Electrolyte and Hypertension Division, University of Pennsylvania Medical Center, Philadelphia, Pennsylvania, USA; M.D. Wilson, Department of Pharmacy Practice and Administration, Philadelphia College of Pharmacy and Science, Philadelphia, Pennsylvania, USA.
Rights and permissions
About this article
Cite this article
Frampton, J.E., Peters, D.H. Ramipril. Drugs 49, 440–466 (1995). https://doi.org/10.2165/00003495-199549030-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199549030-00008