Abstract
Objectives
Antibiotic prescribing in paediatric care is highly prevalent, and quite often, children are prescribed for conditions, like upper respiratory tract infections, which are self-limiting and viral in aetiology. The purpose of this study was to identify potential new targets for provincial antimicrobial stewardship efforts.
Methods
Antibiotic prescription data for children were extracted from a provincial prescription database, linked to physician billing data in order to obtain diagnostic information, and then combined with demographic data in order to obtain patient age, sex and geographic location. Prescription rates were calculated, and trends were examined by major anatomical therapeutic chemical (ATC) classification.
Results
Our cohort included an average of 271,134 children per year and 1,767,652 antibiotic prescriptions. Antibiotic utilization increased 4.5% (from 453 to 474 prescriptions per 1000 population). The greatest increases in prescribing were seen in children aged 0–2 years. Increased indication-specific rates of prescribing were observed in children aged 0–2 years, across every category. Although antibiotic use for upper respiratory tract infections decreased, prescribing rates remain as high as 5 times more than other indications.
Conclusion
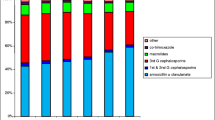
Past studies have widely illustrated decreasing or static rates of prescribing in British Columbia. However, these results signal a potential problem in the sphere of paediatric antibiotic prescribing, wherein rates have been increasing since 2013. Despite the success of provincial efforts in reducing the use of broad-spectrum penicillins, marked surges in the use of classes like tetracyclines, quinolones and other antibacterials identify a new potential target for provincial stewardship.
Résumé
Objectifs
La prescription d’antibiotiques en pédiatrie est hautement prévalente, et très souvent, les enfants se les font prescrire pour des affections spontanément résolutives et à étiologie virale, comme les infections des voies respiratoires supérieures. Notre objectif était de trouver de nouvelles cibles possibles pour les démarches provinciales d’intendance des antimicrobiens.
Méthode
Les données sur la prescription d’antibiotiques aux enfants ont été extraites d’une base de données provinciale sur les ordonnances, que nous avons jumelées aux données de facturation des médecins pour obtenir des informations sur le diagnostic, puis combinées avec les données démographiques pour obtenir l’âge, le sexe et le lieu géographique des patients. Les taux de prescription ont été calculés, et les tendances ont été examinées par grande catégorie du Système de classification anatomique thérapeutique et chimique (ATC).
Résultats
Notre cohorte comptait en moyenne 271 134 enfants par année et 1 767 652 ordonnances d’antibiotiques. Le recours aux antibiotiques a augmenté de 4,5 % (de 453 à 474 ordonnances p. 1000 habitants). La plus forte hausse a été observée chez les enfants de 0 à 2 ans. Des taux accrus de prescription pour indication précise ont été observés chez les enfants de 0 à 2 ans, dans toutes les catégories. Bien que le recours aux antibiotiques pour les infections des voies respiratoires supérieures ait diminué, les taux de prescription sont encore 5 fois supérieurs aux taux de prescription pour les autres indications.
Conclusion
Les études passées font généralement état de taux de prescription stables ou décroissants en Colombie-Britannique. Il semble par contre y avoir un problème possible dans la prescription d’antibiotiques en pédiatrie, où les taux augmentent depuis 2013. Malgré l’efficacité des démarches provinciales pour réduire l’utilisation des pénicillines à spectre étendu, les augmentations marquées de l’utilisation des catégories comme les tétracyclines, les quinolones et autres antibactériens représentent une nouvelle cible possible pour l’intendance provinciale.



Similar content being viewed by others
References
BC Ministry of Health. (2009). Macroscopic and microscopic urinalysis and the investigation of urinary tract Infections. Available at: http://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/urinary-tract-infections [accessed on: June 18, 2019].
BC Ministry of Health. (2010). Otitis media: acute otitis media (AOM) and otitis media with effusion (OME). Available at: http://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/otitis-media [accessed on: June 5, 2019].
BC Ministry of Health. (2015). Asthma in children – diagnosis and management. Available at: http://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/asthma-children [accessed on: July 5, 2019].
Bie, S. D., Kaguelidou, F., Verhamme, K. M. C., Ridder, M. D., Picelli, G., Straus, S. M. J. M., et al. (2016). Using prescription patterns in primary care to derive new quality indicators for childhood community antibiotic prescribing. The Pediatric Infectious Disease Journal, 35(12), 1317–1323.
Bradley, J. S., Byington, C. L., Shah, S. S., Alverson, B., Carter, E. R., Harrison, C., et al. (2011). The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clinical Infectious Diseases, 53(7), e25–e76.
Centers for Disease Control and Prevention (CDC). (n.d.). Get smart: know when antibiotics work in doctor’s offices. Available at: https://www.cdc.gov/getsmart/community/materials-references/index.html. Accessed on: June 3, 2019.
Chow, A. W., Benninger, M. S., Brook, I., Brozek, J. L., Goldstein, E. J., Hicks, L. A., et al. (2012). IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clinical Infectious Diseases, 54(8), e72–e112.
Chung, A., Perera, R., Brueggemann, A. B., Elamin, A. E., Harnden, A., Mayon-White, R., et al. (2007). Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: prospective cohort study. BMJ, 335, 429.
Clavenna, A., & Bonati, M. (2009). Drug prescriptions to outpatient children: a review of the literature. European Journal of Clinical Pharmacology, 65, 749–755.
de Bont, E. G., van Loo, I. H., Dukers-Muijrers, N. H., Hoebe, C. J., Bruggeman, C. A., Dinant, G. J., et al. (2013). Oral and topical antibiotic prescriptions for children in general practice. Archives of Disease in Childhood, 98, 228–231.
Downing, H., Thomas-Jones, E., Gal, M., et al. (2012). The diagnosis of urinary tract infections in young children (DUTY): protocol for a diagnostic and prospective observational study to derive and validate a clinical algorithm for the diagnosis of UTI in children presenting to primary care with an acute illness. BMC Infectious Diseases, 12(1), 158.
Ferris, T. G., Saglam, D., Stafford, R. S., Causino, N., Starfield, B., Culpepper, L., et al. (1998). Changes in the daily practice of primary care for children. Archives of Pediatrics & Adolescent Medicine, 152(3), 227–233.
Fleming-Dutra, K. E., Hersh, A. L., Shapiro, D. J., et al. (2016). Prevalence of inappropriate antibiotic prescriptions among us ambulatory care visits, 2010–2011. JAMA, 315, 1864–1873.
Fleming-Dutra, K. E., Demirjian, A., Bartoces, M., Roberts, R. M., Taylor, T. H., & Hicks, L. A. (2018). Variations in antibiotic and azithromycin prescribing for children by geography and specialty — United States, 2013. The Pediatric Infectious Disease Journal, 37(1), 52–58.
Gonzales, R., Malone, D. C., Maselli, J. H., & Sande, M. A. (2001). Excessive antibiotic use for acute respiratory infections in the United States. Clinical Infectious Diseases, 33(6), 757–762.
Goossens, H., Ferech, M., Vander Stichele, R., Elseviers, M., & ESAC Project Group. (2005). Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet, 365, 579–587.
Grijalva, C. G., Nuorti, J. P., & Griffin, M. R. (2009). Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA, 302(7), 758–766.
Hersh, A. L., Shapiro, D. J., Pavia, A. T., & Shah, S. S. (2011). Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics, 128(6), 1053–1061.
Holstiege, J., & Garbe, E. (2013). Systemic antibiotic use among children and adolescents in Germany: a population-based study. European Journal of Pediatrics, 172, 787–795.
Le Saux, N. (2014). Antimicrobial stewardship in daily practice: managing an important resource. Paediatrics & Child Health, 19(4), 261–265.
Levine, M. (2017). Are we choosing wisely in Canada? Canadian Journal of General Internal Medicine, 12(3).
McCaig, L. F., Besser, R. E., & Hughes, J. M. (2003). Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerging Infectious Diseases, 9(4), 432–437.
No author. (n.d.). Do bugs need drugs? A community program for wise use of antibiotics. Available at: http://www.dobugsneeddrugs.org [accessed on: June 22, 2019].
Province of British Columbia. (n.d.). Population estimates 1886–2017. Available at: https://www2.gov.bc.ca/gov/content/data/statistics/people-population-community/population/population-estimates. [accessed on: April 14, 2019].
Public Health Agency of Canada. Canadian antimicrobial resistance surveillance system 2017. Available at: https://www.canada.ca/en/public-health/services/publications/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2017-report-executive-summary.html [accessed on: June 4, 2019].
Public Health England. (2015). English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) 2010 to 2014. Available at: https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobialutilisation-and-resistance-espaur-report. [accessed on: June 29, 2019].
Shulman, S. T., Bisno, A. L., Clegg, H. W., Gerber, M. A., Kaplan, E. L., Lee, G., et al. (2012). Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clinical Infectious Diseases, 55(10), e86–e102.
Stevens, D. L., Bisno, A. L., Chambers, H. F., Dellinger, E. P., Goldstein, E. J., Gorbach, S. L., et al. (2014). Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clinical Infectious Diseases, 59(2), 147–159.
Sturkenboom, M. C. J. M., Verhamme, K. M. C., Nicolosi, A., Murray, M. L., Neubert, A., Caudri, D., et al. (2008). Drug use in children: cohort study in three European countries. BMJ, 337, a2245.
van den Broek d’Obrenan, J., Verheij, T. J., Numans, M. E., & van der Velden, A. W. (2014). Antibiotic use in Dutch primary care: Relation between diagnosis, consultation and treatment. The Journal of Antimicrobial Chemotherapy, 69, 1701–1707.
Williams, M. R., Greene, G., Naik, G., Hughes, K., Butler, C. C., & Hay, A. D. (2018). Antibiotic prescribing quality for children in primary care: an observational study. British Journal of General Practice, 68(667), e90–e96.
World Health Organization. (1996). Guidelines for ATC classification and DDD assignment, in Guidelines for ATC classification and DDD assignment.
Zetts, R. M., Stoesz, A., Smith, B. A., & Hyun, D. Y. (2018). Outpatient antibiotic use and the need for increased antibiotic stewardship efforts. Pediatrics, 141(6), e20174124.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 49 kb)
Rights and permissions
About this article
Cite this article
Saatchi, A., Marra, F. Increasing paediatric prescribing rates in British Columbian children: cause for concern?. Can J Public Health 111, 523–530 (2020). https://doi.org/10.17269/s41997-020-00298-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-020-00298-2