Abstract
OBJECTIVES: We aimed to calculate trends in incidence and prevalence rates of long-term opioid use for non-cancer pain, as well as to describe the characteristics of long-term opioid users and their patterns of opioid use.
METHODS: We used population-based linked health care and socio-demographic administrative data for British Columbia (BC) between 2005 and 2012. We included individuals who had at least one episode of long-term opioid use during the study period and who were not cancer or palliative care patients.
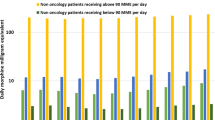
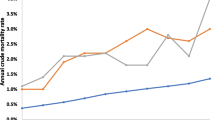
RESULTS: Long-term users comprised only 10% of all individuals prescribed opioids for non-cancer pain, but accounted for 64% of all opioid prescriptions and 87% of all morphine equivalents dispensed in BC during this period. While the incidence rate did not significantly change, the prevalence rate increased by 27% for men and 22% for women. In 2012, there were 3.80 (3.72–3.88) new long-term opioid users per 1,000 men and 4.42 (4.34–1.51) new users per 1,000 women. At the same time, there were 18.3 (95% CI 18.1–18.5) existing long-term users per 1,000 men and 21.7 users (95% CI 21.5–21.9) per 1,000 women. Overall, 2.4% of BC residents were long-term users of prescription opioids in 2012. Most long-term users had one continuous episode of use spanning multiple years. Almost two thirds took opioids every other day or more frequently.
CONCLUSION: There is a growing population of long-term opioid users for non-cancer pain in BC, with higher incidence and prevalence rates observed among women than among men.
Résumé
OBJECTIFS: Nous avons cherché à calculer les tendances dans les taux d’incidence et de prévalence de l’usage à long terme d’opioïdes contre la douleur non cancéreuse, ainsi qu’à décrire les caractéristiques des consommateurs à long terme d’opioïdes et leurs types d’usage d’opioïdes.
MÉTHODE: Nous avons utilisé les données administratives sociodémographiques et de soins de santé liées à la population de la Colombie-Britannique (C.-B.) de 2005 à 2012. Nous avons inclus les personnes ayant eu au moins un épisode d’usage à long terme d’opioïdes durant la période de l’étude et qui n’étaient pas des patients cancéreux ni aux soins palliatifs.
RÉSULTATS: Les consommateurs à long terme ne représentaient que 10% des personnes à qui l’on avait prescrit des opioïdes contre la douleur non cancéreuse, mais ils avaient reçu 64% des prescriptions d’opioïdes et 87% de tous les équivalents de morphine distribués en C.-B. durant la période de l’étude. Le taux d’incidence n’a pas changé de manière significative, mais le taux de prévalence a augmenté de 27% chez les hommes et de 22% chez les femmes. En 2012, il y avait 3,80 (3,72–3,88) nouveaux consommateurs à long terme d’opioïdes pour 1 000 hommes et 4,42 (4,34–1,51) nouvelles consommatrices pour 1 000 femmes. Simultanément, il y avait 18,3 (IC de 95% 18,1–18,5) consommateurs à long terme existants pour 1 000 hommes et 21,7 consommatrices à long terme existantes (IC de 95% 21,5–21,9) pour 1 000 femmes. Dans l’ensemble, 2,4% des résidents de la C.-B. étaient des consommateurs à long terme d’opioïdes d’ordonnance en 2012. La plupart des consommateurs à long terme avaient eu un épisode continu de consommation sur plusieurs années. Près des deux tiers prenaient des opioïdes tous les deux jours ou plus souvent.
CONCLUSION: Il existe une population croissante de consommateurs à long terme d’opioïdes contre la douleur non cancéreuse en C.-B., et l’on observe des taux d’incidence et de prévalence plus élevés chez les femmes que chez les hommes.
Similar content being viewed by others
References
Pain and Policy Studies Group (University of Wisconsin-Madison). Global Opioid Consumption, 2011. Available at: http://www.painpolicy.wisc.edu/country/profile/canada (Accessed December 4, 2015).
Reitsma M, Tranmer J, Buchanan D, Vandenkerkhof E. The prevalence of chronic pain and pain-related interference in the Canadian population from 1994 to 2008. Chronic Dis Inj Can 2011;31(4):157–64. PMID: 21978639.
Gomes T, Paterson JM, Caetano P, Sketris I, Henry D. Canadian Network for Observational Drug Effect Studies. Part 1: Changes in the dispensing of oral opioid drugs in Canadian provinces between 2008 and the end of 2013. Unpublished report. Montreal, QC: Canadian Network for Observational Drug Effect Studies, 2015.
Chou R, Turner JA, Devine EB, Hansen RN, Sullivan SD, Blazina I, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health pathways to prevention workshop. Ann Intern Med 2015;162(4):276–86. PMID: 25581257. doi: 10.7326/M14-2559.
Braden J, Russo J, Fan M, Edlund MJ, Martin BC, DeVries A, et al. Emergency department visits among recipients of chronic opioid therapy. Arch Intern Med 2010;170(16):1425–32. PMID: 20837827. doi: 10.1001/archinternmed.2010.273.
Wisniewski AM, Purdy CH, Blondell RD. The epidemiologic association between opioid prescribing, non-medical use, and emergency department visits. J Addict Dis 2008;27(1):1–11. PMID: 18551883. doi: 10.1300/J069v27n01_01.
Gomes T, Redelmeier DA, Juurlink DN, Dhalla IA, Camacho X, Mamdani MM. Opioid dose and risk of road trauma in Canada: A population-based study. JAMA Intern Med 2013;173(3):196–201. PMID: 23318919. doi: 10.1001/2013.jamainternmed.733.
Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305(13):1315–21. PMID: 21467284. doi: 10.1001/jama.2011.370.
Fischer B, Jones W, Rehm J. Trends and changes in prescription opioid analgesic dispensing in Canada 2005–2012: An update with a focus on recent interventions. BMC Health Serv Res 2014;14(1):90. PMID: 24572005. doi: 10.1186/1472-6963-14-90.
Gomes T, Mamdani MM, Paterson JM, Dhalla IA, Juurlink DN. Trends in high-dose opioid prescribing in Canada. Can Fam Physician 2014;60(9):826–32. PMID: 25217680.
Patented Medicine Prices Review Board. Utilization of Prescription Opioids in Canada’s Public Drug Plans, 2006/07 to 2012/13. Ottawa, ON: Patented Medicine Prices Review Board, 2014.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: A retrospective cohort study. Arch Intern Med 2012;172(5):425–30. PMID: 22412106. doi: 10.1001/archinternmed.2011.1827.
Kaplovitch E, Gomes T, Camacho X, Dhalla IA, Mamdani MM, Juurlink DN. Sex differences in dose escalation and overdose death during chronic opioid therapy: A population-based cohort study. PLoS ONE 2015;10(8):e0134550. PMID: 26291716. doi: 10.1371/journal.pone.0134550.
Canadian Institute for Health Information. Discharge Abstract Database (Hospital Separations). Population Data BC. Data Extract. MOH, 2015. Available at: http://www.popdata.bc.ca/data (Accessed December 4, 2015).
BC Ministry of Health. Medical Services Plan (MSP) Payment Information File. Population Data BC. Data Extract. MOH, 2015. Available at: http://www.popdata.bc.ca/data (Accessed December 4, 2015).
BC Ministry of Health. PharmaNet. BC Ministry of Health. Data Extract. Data Stewardship Committee, 2015. Available at: http://www.popdata.bc.ca/data (Accessed December 4, 2015).
Hanley G, Morgan S. On the validity of area-based income measures to proxy household income. BMC Health Serv Res 2008;8(1):79. PMID: 18402681. doi: 10.1186/1472-6963-8-79.
Boudreau D, Von Korff M, Rutter CM, Saunders K, Ray GT, Sullivan MD, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf 2009;18(12):1166–75. PMID: 19718704. doi: 10.1002/pds.vl8:12.
Campbell CI, Weisner C, Leresche L, Ray GT, Saunders K, Sullivan MD, et al. Age and gender trends in long-term opioid analgesic use for noncancer pain. Am J Public Health 2010;100(12):2541–47. PMID: 20724688. doi: 10.2105/AJPH.2009.180646.
Weiner J, Abrams C. The Johns Hopkins ACG System Technical Reference Guide, Version 10.0. Baltimore, MD: The Johns Hopkins University, 2011.
Shah BR, Chiu M, Amin S, Ramani M, Sadry S, Tu JV. Surname lists to identify South Asian and Chinese ethnicity from secondary data in Ontario, Canada: A validation study. BMC Med Res Methodol 2010;10(1):42. PMID: 20470433. doi: 10.1186/1471-2288-10-42.
British Columbia. The Diversity of Visible Minorities and Ethnic Origins in BC. Victoria, BC: Ministry of Attorney General and Minister Responsible for Multiculturalism, 2008.
Morgan SG, Hanley G, Cunningham C, Quan H. Ethnic differences in the use of prescription drugs: A cross-sectional analysis of linked survey and administrative data. Open Med 2011;5(2):e87–93. PMID: 21915239.
Puyat JH, Hanley GE, Cunningham CM, Law MR, Wong ST, Sutherland JM, et al. Ethnic disparities in antipsychotic drug use in British Columbia: A cross-sectional retrospective study. Psychiatr Serv 2011;62(9):1026–31. PMID: 21885580. doi: 10.1176/ps.62.9.pss6209_1026.
Martin BC, Fan M-Y, Edlund MJ, DeVries A, Braden JB, Sullivan MD. Long-term chronic opioid therapy discontinuation rates from the TROUP study. J Gen Intern Med 2011;26(12):1450–57. PMID: 21751058. doi: 10.1007/S11606-011-1771-0.
Vanderlip ER, Sullivan MD, Edlund MJ, Martin BC, Fortney J, Austen M, et al. National study of discontinuation of long-term opioid therapy among veterans. Pain 2014;155(12):2673–79. PMID: 25277462. doi: 10.1016/j.pain.2014.09.034.
Gilson AM, Maurer MA, Ryan KM, Rathouz PJ, Cleary JF. Using a morphine equivalence metric to quantify opioid consumption: Examining the capacity to provide effective treatment of debilitating pain at the global, regional, and country levels. J Pain Symptom Manage 2013;45(4):681–700. PMID: 23017614. doi: 10.1016/j.jpainsymman.2012.03.011.
BC Cancer Agency. Age-Standardized Cancer Incidence (per 100,000) for British Columbia, 2008–2012, 2014. Available at: http://www.bccancer.bc.ca/statistics-and-reports-site/Documents/Incidence_agestd_rates_2012.pdf (Accessed December 4, 2015).
Juurlink DN, Dhalla IA. Dependence and addiction during chronic opioid therapy. J Med Toxicol 2012;8(4):393–99. PMID: 23073725. doi: 10.1007/S13181-012-0269-4.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest: None to declare.
Rights and permissions
About this article
Cite this article
Smolina, K., Gladstone, E.J., Rutherford, K. et al. Patterns and trends in long-term opioid use for non-cancer pain in British Columbia, 2005–2012. Can J Public Health 107, e404–e409 (2016). https://doi.org/10.17269/CJPH.107.5413
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/CJPH.107.5413