Abstract
Background
The advent of tissue engineering and the clinical applications with cultured epidermal autograft (CEA) have improved the prognosis of severely burned patients. Marjolin ulcers (MUs) are a well-known complication of burns. These malignant neoplasm transformations of burn scars are usually squamous cell carcinomas with a higher incidence of regional metastases. Radical surgery remains the treatment of choice.
Objectives
To identify cases of malignant transformation occurring at sites of CEA in a cohort of 68 massively burned patients.
Materials & Methods
A retrospective single-centre study was performed from April 2017 to June 2019 at the Military Hospital of Clamart (France). A total of 34 patients treated between 1991 and 2013 (including one post-mortem) were included.
Results
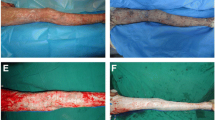
Four cases of squamous cell carcinoma occurred in areas previously covered by CEA. The data from clinical and histopathological examination as well as treatment modalities are presented. One patient died as a result of the evolution of his squamous cell carcinoma, and two others required salvage amputation due to locoregional recurrence. The prevalence of these CEA-MUs is estimated at between 5.9% and 11.7% and the person-time incidence rate of CEA-related MUs is about 5.9 per 1,000 persons-years. In our study, the average time to malignant transformation seems considerably shortened (32–35 years for “classic burn MU” versus 15.7 years for CEA-MU).
Conclusion
This first documented case series of CEA-MUs demonstrates the need to inform caregivers and educate patients. Further studies are needed to specify the true incidence of CEA-graft site malignancy.
Similar content being viewed by others
References
Copcu E. Marjolin’s ulcer: a preventable complication of burns? Plast Reconstr Surg 2009; 124: 156e–64e.
Dupree MT, Boyer JD, Cobb MW. Marjolin’s ulcer arising in a burn scar. Cutis 1998; 62: 49–51.
Fleming MD, Hunt JL, Purdue GF, Sandstad J. Marjolin’s ulcer: a review and reevaluation of a difficult problem. J Burn Care Rehabil 1990; 11: 460–9.
Copcu E, Aktas A, Sişman N, Oztan Y. Thirty-one cases of Marjolin’s ulcer. Clin Exp Dermatol 2003; 28: 138–41.
Yu N, Long X, Lujan-Hernandez JR, et al. Marjolin’s ulcer: a preventable malignancy arising from scars. World J Surg Oncol 2013; 11: 313.
Pratt DV, Pelton RW, Patel BC, Anderson RL. Burn scar malignancies of the eyelids. Ophthal Plast Reconstr Surg 2000; 16: 432–7.
Kadir AR. Burn scar neoplasm. Ann Burns Fire Disasters 2007; 20: 185–8.
Bozkurt M, Kapi E, Kuvat SV, Ozekinci S. Current concepts in the management of Marjolin’s ulcers: outcomes from a standardized treatment protocol in 16 cases. J Burn Care Res 2010; 31: 776–80.
Bean DJ, Rees RS, O’Leary JP, Lynch JB. Carcinoma of the hand: a 20-year experience. South Med J 1984; 77: 998–1000.
Ozek C, Celik N, Bilkay U, Akalin T, Erdem O, Cagdas A. Marjolin’s ulcer of the scalp: report of 5 cases and review of the literature. J Burn Care Rehabil 2001; 22: 65–9.
Kerr-Valentic MA, Samimi K, Rohlen BH, Agarwal JP, Rockwell WB. Marjolin’s ulcer: modern analysis of an ancient problem. Plast Reconstr Surg 2009; 123: 184–91.
Cantwell P, Brooks A. Multiple melanoma in a burns scar. BMJ Case Rep 2018; 11: e227295.
Gül U, Kiliç A. Squamous cell carcinoma developing on burn scar. Ann Plast Surg 2006; 56: 406–8.
Abdi MA, Yan M, Hanna TP. Systematic review of modern case series of squamous cell cancer arising in a chronic ulcer (Marjolin’s ulcer) of the Skin. JCO Glob Oncol 2020; 6: 809–18.
Khan K, Schafer C, Wood J. Marjolin ulcer: a comprehensive review. Adv Skin Wound Care 2020; 33: 629–34.
Theopold C, Hoeller D, Velander P, Demling R, Eriksson E. Graft site malignancy following treatment of full-thickness burn with cultured epidermal autograft. Plast Reconstr Surg 2004; 114: 1215–9.
Theopold C, Eriksson E. The need for aggressive follow-up after cultured epidermal autograft-grafted full-thickness burn. Plast Reconstr Surg 2006; 117: 708.
Hickerson WL, Remmers AE, Recker DP. Twenty-five years’ experience and beyond with cultured epidermal autografts for coverage of large burn wounds in adult and pediatric patients, 1989–2015. J Burn Care Res 2019;40:157–65.
Rheinwald JG, Green H. Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell 1975; 6: 331–43.
Cuono C, Langdon R, McGuire J. Use of cultured epidermal autografts and dermal allografts as skin replacement after burn injury. Lancet Lond Engl 1986; 1: 1123–4.
Cuono CB, Langdon R, Birchall N, Barttelbort S, McGuire J. Composite autologous-allogeneic skin replacement: development and clinical application. Plast Reconstr Surg 1987; 80: 626–37.
O’Connor N, et al. Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet Lond Engl 1981; 1: 75–8.
Atiyeh BS, Costagliola M. Cultured epithelial autograft (CEA) in burn treatment: three decades later. Burns J Int Soc Burn Inj 2007; 33: 405–13.
Paddle-Ledinek JE, Cruickshank DG, Masterton JP. Skin replacement by cultured keratinocyte grafts: an Australian experience. Burns J Int Soc Burn Inj 1997; 23: 204–11.
Cirodde A, Leclerc T, Jault P, Duhamel P, Lataillade J-J, Bargues L. Cultured epithelial autografts in massive burns: a single-center retrospective study with 63 patients. Burns J Int Soc Burn Inj 2011; 37: 964–72.
Teepe RG, Kreis RW, Koebrugge EJ, et al. The use of cultured autologous epidermis in the treatment of extensive burn wounds. J Trauma 1990; 30: 269–75.
Iqbal FM, Sinha Y, Jaffe W. Marjolin’s ulcer: a rare entity with a call for early diagnosis. BMJ Case Rep 2015; 2015: bcr2014208176.
Metwally IH, Roshdy A, Saleh SS, Ezzat M. Epidemiology and predictors of recurrence of Marjolin’s ulcer: experience from Mansoura Universityxs. Ann R Coll Surg Engl 2017; 99: 245–9.
Xiao-Wu W, Herndon DN, Spies M, Sanford AP, Wolf SE. Effects of delayed wound excision and grafting in severely burned children. Arch Surg Chic Ill 2002; 137: 1049–54.
Türegün M, Nişanci M, Güler M. Burn scar carcinoma with longer lag period arising in previously grafted area. Burns J Int Soc Burn Inj 1997; 23: 496–7.
Lawrence EA. Carcinoma arising in the scars of thermal burns, with special reference to the influence of the age at burn on the length of the induction period. Surg Gynecol Obstet 1952; 95: 579–88.
Das KK, Chakaraborty A, Rahman A, Khandkar S. Incidences of malignancy in chronic burn scar ulcers: experience from Bangladesh. Burns J Int Soc Burn Inj 2015; 41: 1315–21.
Edwards MJ, Hirsch RM, Broadwater JR, Netscher DT, Ames FC. Squamous cell carcinoma arising in previously burned or irradiated skin. Arch Surg Chic Ill 1989; 124: 115–7.
Costache M, Desa LT, Mitrache LE, et al. Cutaneous verrucous carcinoma — report of three cases with review of literature. Rom J Morphol Embryol 2014; 55: 383–8.
Braye F, Oddou L, Bertin-Maghit M, et al. Widely meshed autograft associated with cultured autologous epithelium for the treatment of major burns in children: report of 12 cases. Eur J Pediatr Surg 2000; 10: 35–40.
Nthumba PM. Marjolin’s ulcers in sub-Saharan Africa. World J Surg 2010; 34: 2272–7.
Ozek C, Cankayali R, Bilkay U, et al. Marjolin’s ulcers arising in burn scars. J Burn Care Rehabil 2001; 22: 384–9.
Reich-Schupke S, Doerler M, Wollina U, et al. Squamous cell carcinomas in chronic venous leg ulcers. Data of the German Marjolin Registry and review. J Dtsch Dermatol Ges 2015; 13: 1006–13.
Delaitre L, Martins-Héricher J, Truchot E, et al. [Regression of cutaneous basal cell and squamous cell carcinoma under pembrolizumab]. Ann Dermatol Venereol 2020; 147: 279–84.
Lavaud J, Blom A, Longvert C, Fort M, Funck-Brentano E, Saiag P. Pembrolizumab and concurrent hypo-fractionated radiotherapy for advanced non-resectable cutaneous squamous cell carcinoma. Eur J Dermatol 2019; 29: 63640.
Baus A, Chatard M, Bich CS, et al. [Current place of cultured epithelial autografts in the management of massive burns and future prospects: Literature review]. Ann Chir Plast Esthet 2021; 66: 10–8.
Acknowledgment and disclosures
Acknowledgments: We would like to thank Dr. N’Guyen Anhtuan (Pathology Department, Begin Military Hospital, Saint Mandé, France), Dr. Benali-Abdeellaoui Khadija (Nuclear Medicine Department, Bichat Hospital, Paris, France), Dr Pinatel Baptiste (Plastic and Reconstructive Surgery, Saint Luc and Saint Joseph Hospital, Lyon, France), Dr Trouillas Marina (PhD, IRBA/French Armed-forces Biomedical Research Institute, Clamart, France) and Dr Jacob Louis (Physical and Rehabilitation Medicine Department, Garches Hospital, France) for their proofreading and scientific contribution.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflicts of interest
None of the authors has a financial interest in any of the products, devices or drugs mentioned in this manuscript. This review did not receive any funding. The opinions or assertions expressed here are the private views of the authors and are not to be considered as official or as reflecting the views of the French Defence Health Service.
About this article
Cite this article
Baus, A., Keilani, C., Brunet-Possenti, F. et al. Marjolin ulcers after cultured epidermal autograft in severely burned patients: a rare case series and literature review. Eur J Dermatol 31, 759–770 (2021). https://doi.org/10.1684/ejd.2021.4174
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1684/ejd.2021.4174