Abstract
Background
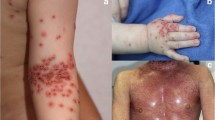
Dermatitis herpetiformis (DH) and celiac disease (CD) are considered to be autoimmune diseases that share a specific trigger (gluten) and a common genetic background (HLA-DQ2/DQ8). However, the pathogenesis of DH is not yet fully understood and no data are available regarding a possible role of fibroblasts in this disease.
Objectives
The aim of this study was to assess baseline DNA damage in fibroblasts in DH-diagnosed patients vs. fibroblasts of controls without DH or CD.
Materials and Methods
Primary fibroblast cultures were derived from dermal biopsies from DH patients and controls (without DH or CD). In vitro genotoxic damage was investigated using the comet assay and γH2AX test after different treatments (with 33mer peptide and digested gliadin [DG]) in order to investigate a correlation between oxidative stress (evaluated by reactive oxygen species formation) and glutathione content.
Results
Our results demonstrate a difference in baseline DNA damage between cutaneous fibroblasts of controls and DH patients, moreover, DNA damage significantly increased after exposure to gluten (DG and 33mer peptide) in fibroblasts from DH patients. DNA damage in fibroblasts from patients under dapsone treatment was similar to that of the control group.
Conclusion
Our data indicate that oxidative stress and DNA damage may be characteristics of fibroblasts from DH patients who are not treated with dapsone, particularly after exposure to gliadin peptides.
Similar content being viewed by others
References
Collin P, Salmi TT, Hervonen K, Kaukinen K, Reunala T. Dermatitis herpetiformis: a cutaneous manifestation of coeliac disease. Ann Med 2017; 49:23–31.
Bonciani D, Verdelli A, Bonciolini V, et al. dermatitis herpetiformis: from the genetics to the development of skin lesions. Clin Dev Immunol 2012; 2012:7.
Hietikko M, Hervonen K, Ilus T, et al. Ex vivo Culture of duodenal biopsies from patients with dermatitis herpetiformis indicates that transglutaminase 3 antibody production occurs in the gut. Acta Derm Venereol 2018; 98:366–72.
Mendes FBR, Hissa-Elian A, De Abreu M, Scaff Gonc¸alves V. Review: dermatitis herpetiformis. An Bras Dermatol 2013; 88:594–9.
Herrera MG, Benedini LA, Lonez C, et al. Self-assembly of 33-mer gliadin peptide oligomers. Soft Matter 2015; 11:8648–60.
Paolella G, Lepretti M, Barone V, et al. Celiac anti-type 2 trans-glutaminase antibodies induce differential effects in fibroblasts from celiac disease patients and from healthy subjects. Amino Acids 2017; 49:541–50.
Qiao S, Bergseng E, Molberg O, et al. Antigen presentation to celiac lesion-derived T cells of a 33-mer gliadin peptide naturally formed by gastrointestinal digestion. J Immunol 2017; 173:1757–62.
Berroth A, Kühnl J, Kurschat N, et al. Role of fibroblasts in the pathogenesis of atopic dermatitis. J Allergy Clin Immunol 2013; 131:1547–54.
Clarindo MV, Soligo EM, Ruaro RT. Presentation diagnosis and treatment. An Bras Dermatol 2014; 89:865–77.
Salmi TT, Hervonen K, Kurppa K, Collin P, Kaukinen K, Reunala T. Celiac disease evolving into dermatitis herpetiformis in patients adhering to normal or gluten-free diet. Scand J Gastroenterol 2015; 50:387–92.
Reunala T, Salmi TT, Hervonen K, et al. IgA antiepidermal transglutaminase antibodies in dermatitis herpetiformis: a significant but not complete response to a gluten-free diet treatment. Brit J Dermatol 2015; 172:1139–41.
Kotze L. Review: dermatitis herpetiformis. Arq Gastroenterol 2013; 50:231–5.
Kelly C, Bai J, Edwin L, Leffler D. Advances in diagnosis and management of celiac disease. Gastroenterology 2015; 148:1175–86.
Antiga E, Caproni M. The diagnosis and treatment of dermatitis herpetiformis. Clin Cosmet Investig Dermatol 2015; 8:257–65.
Ferretti G, Bacchetti T, Masciangelo S, Saturni L. Celiac disease, inflammation and oxidative damage: a nutrigenetic approach. Nutrients 2012; 4:243–57.
Hall RP, Takeuchi F, Benbenisty KM, Streilein RD Cutaneous endothelial cell activation in normal skin of patients with dermatitis herpetiformis associated with increased serum levels of IL-8, sE-selectin, and TNF-alpha. J Invest Dermatol 2006; 126:1331–7.
Reunala T, Salmi TT, Hervonen K. Dermatitis herpetiformis: pathognomonic transglutaminase IGA deposits in the skin and excellent prognosis on a gluten-free diet. Acta Derm Venereol 2015; 95:917–22.
Schraufstatter I, Hyslop PA, Jackson JH, Cochrane CG. Oxidantinduced DNA damage of target cells. J Clin Invest 1988; 82:1040–50.
Vaira V, Roncoroni L, Barisani D, et al. MicroRNA profiles in coeliac patients distinguish different clinical phenotypes and are modulated by gliadin peptides in primary duodenal fibroblasts. Clin Sci 2014; 126:417–23.
Price P, Mcmillan TJ. Use of the tetrazolium assay in measuring the response of human tumor cells to ionizing radiation. Cancer Res 1990; 50:1392–6.
Friis S, Dabelsteen E, Sjostrom H, Noren O, Jarnum S. Gliadin uptake in human enterocytes. Differences between coelic patients in remission and control individuals. Gut 1992; 33:1487–92.
Widel M, Krzywon A, Gajda K, Skonieczna M, Rzeszowska-Wolny J. Induction of bystander effects by UVA, UVB, and UVC radiation in human fibroblasts and the implication of reactive oxygen species. Free Radic Biol Med 2014; 68:278–87.
Lowry OH, Rosebrough NJ, Farr AL, Randal RJ. Protein measurement with the Folin phenol reagent. J Biol Chem 1951; 193:265–75.
Fairweather D. Autoimmune Disease: Mechanisms. Chichester: John Wiley & Sons Ltd.; Encyclopedia of Life Sciences, 2007.
Smith TJ. Insights into the role of fibroblasts in human autoimmune diseases. Clin Exp Immunol 2005; 141:388–97.
Cardones RG, Hall RP. Pathophysiology of dermatitis herpetiformis: a model for cutaneous manifestations of gastrointestinal inflammation. Immunol Allergy Clin 2012; 32:263–74.
Nicolas MEO, Krause PK, Gibson LE, Murray JA. Dermatitis her-petiformis. Int J Dermatol 2003; 42:588–600.
Görög K, Németh L, Szabó B, et al. Decreased fibrinolytic potential and morphological changes of fibrin structure in dermatitis herpetiformis. J Dermatol Sci 2016; 84:17–23.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lombardo, G., Marabini, L., Doneda, L. et al. DNA damage in human skin fibroblasts from patients with dermatitis herpetiformis. Eur J Dermatol 29, 167–173 (2019). https://doi.org/10.1684/ejd.2019.3528
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1684/ejd.2019.3528