Abstract
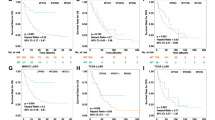
This study aimed to identify subtypes of genomic variants associated with the efficacy of immune checkpoint inhibitors (ICIs) by conducting systematic literature search in electronic databases up to May 31, 2021. The main outcomes including overall survival (OS), progression-free survival (PFS), objective response rate (ORR), and durable clinical benefit (DCB) were correlated with tumor genomic features. A total of 1546 lung cancer patients with available genomic variation data were included from 14 studies. The Kirsten rat sarcoma viral oncogene homolog G12C (KRASG12C) mutation combined with tumor protein P53 (TP53) mutation revealed the promising efficacy of ICI therapy in these patients. Furthermore, patients with epidermal growth factor receptor (EGFR) classical activating mutations (including EGFRL858R and EGFRΔ19) exhibited worse outcomes to ICIs in OS (adjusted hazard ratio (HR), 1.40; 95% confidence interval (CI), 1.01–1.95; P=0.0411) and PFS (adjusted HR, 1.98; 95% CI, 1.49–2.63; P<0.0001), while classical activating mutations with EGFRT790M showed no difference compared to classical activating mutations without EGFRT790M in OS (adjusted HR, 0.96; 95% CI, 0.48–1.94; P=0.9157) or PFS (adjusted HR, 0.72; 95% CI, 0.39–1.35; P=0.3050). Of note, for patients harboring the Usher syndrome type-2A (USH2A) missense mutation, correspondingly better outcomes were observed in OS (adjusted HR, 0.52; 95% CI, 0.32–0.82; P=0.0077), PFS (adjusted HR, 0.51; 95% CI, 0.38–0.69; P<0.0001), DCB (adjusted odds ratio (OR), 4.74; 95% CI, 2.75–8.17; P<0.0001), and ORR (adjusted OR, 3.45; 95% CI, 1.88–6.33; P<0.0001). Our findings indicated that, USH2A missense mutations and the KRASG12C mutation combined with TP53 mutation were associated with better efficacy and survival outcomes, but EGFR classical mutations irrespective of combination with EGFRT790M showed the opposite role in the ICI therapy among lung cancer patients. Our findings might guide the selection of precise targets for effective immunotherapy in the clinic.
概要
本研究以探索与免疫检查点抑制剂 (ICIs) 效果有关联的基因突变亚型为目标, 进行了系统文献检索 (电子数据库截至 2021 年 5 月 31 日). 与肿瘤基因特征相关联的主要结局事件包括: 总生存期、 无进展生存期、 客观反应率、 持久临床获益. 我们从 14 项研究中总计提取了 1546 个有基因突变数据的肺癌患者, 发现 ICIs 治疗在 KRASG12C联合 TP53 双突变的患者中有更好的疗效, 而在携带 EGFR 经典激活突变 (包括 EGFRL585R 和 EGFRΔ19) 的患者中的效果则截然相反: 总生存期 (调整后 HR, 1.40; 95% CI, 1.01–1.95; P=0.0411), 无进展生存期 (调整后 HR, 1.98; 95% CI, 1.49–2.63; P<0.0001). 另外, ICIs 治疗在 EGFR 经典突变联合 EGFRT790M双突变患者与仅有 EGFR 经典突变的患者在总生存期 (调整后 HR, 0.96; 95% CI, 0.48–1.94; P=0.9157) 与无进展生存期 (调整后 HR, 0.72; 95% CI, 0.39–1.35; P=0.3050) 中均无明显差异. 更重要的是, 我们发现 ICIs 在携带 USH2A 错义突变的患者中可能有更好的疗效: 总生存期 (调整后 HR, 0.52; 95% CI, 0.32–0.82; P=0.0077), 无进展生存期 (调整后 HR, 0.51; 95% CI, 0.38–0.69; P<0.0001), 持久临床获益 (调整后 OR, 4.74; 95% CI, 2.75–8.17; P<0.0001) 与客观反应率 (调整后 OR, 3.45; 95% CI, 1.88–6.33; P<0.0001). 综上, 我们的研究发现在使用 ICIs 疗法的肺癌患者中, USH2A 错义突变、 KRASG12C 联合 TP53 双突变与更好的疗效和生存结局有关, 而 EGFR 经典突变无论是否合并 EGFRT790M 突变都预示着不良结局, 我们的结果可能会对在肿瘤 ICIs 的精准治疗方案提供新的依据和靶标.
Similar content being viewed by others
References
Abou Alaiwi S, Nassar AH, Xie WL, et al., 2020. Mammalian SWI/SNF complex genomic alterations and immune checkpoint blockade in solid tumors. Cancer Immunol Res, 8(8): 1075–1084. https://doi.org/10.1158/2326-6066.Cir-19-0866
Addeo A, Banna GL, Weiss GJ, 2019. Tumor mutation burden—from hopes to doubts. JAMA Oncol, 5(7):934–935. https://doi.org/10.1001/jamaoncol.2019.0626
Anagnostou V, Niknafs N, Marrone K, et al., 2020. Multimodal genomic features predict outcome of immune checkpoint blockade in non-small-cell lung cancer. Nat Cancer, 1(1): 99–111. https://doi.org/10.1038/s43018-019-0008-8
Arbour KC, Rizvi H, Plodkowski AJ, et al., 2021. Treatment outcomes and clinical characteristics of patients with KRAS-G12C-mutant non-small cell lung cancer. Clin Cancer Res, 27(8):2209–2215. https://doi.org/10.1158/1078-0432.Ccr-20-4023
Assoun S, Theou-Anton N, Nguenang M, et al., 2019. Association of TP53 mutations with response and longer survival under immune checkpoint inhibitors in advanced non-small-cell lung cancer. Lung Cancer, 132:65–71. https://doi.org/10.1016/j.lungcan.2019.04.005
Bentham R, Litchfield K, Watkins TBK, et al., 2021. Using DNA sequencing data to quantify T cell fraction and therapy response. Nature, 597(7877):555–560. https://doi.org/10.1038/s41586-021-03894-5
Brahmer JR, 2013. Harnessing the immune system for the treatment of non-small-cell lung cancer. J Clin Oncol, 31(8):1021–1028. https://doi.org/10.1200/jco.2012.45.8703
Cai WJ, Zhou DP, Wu WB, et al., 2018. MHC class II restricted neoantigen peptides predicted by clonal mutation analysis in lung adenocarcinoma patients: implications on prognostic immunological biomarker and vaccine design. BMC Genomics, 19:582. https://doi.org/10.1186/s12864-018-4958-5
Canon J, Rex K, Saiki AY, et al., 2019. The clinical KRAS (G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature, 575(7781):217–223. https://doi.org/10.1038/s41586-019-1694-1
Cho JW, Park S, Kim G, et al., 2021. Dysregulation of TFII-B-TRM lymphocyte cooperation is associated with unfavorable anti-PD-1 responses in EGFR-mutant lung cancer. Nat Commun, 12:6068. https://doi.org/10.1038/s41467-021-26362-0
Dong ZY, Zhong WZ, Zhang XC, et al., 2017. Potential predictive value of TP53 and KRAS mutation status for response to PD-1 blockade immunotherapy in lung adenocarcinoma. Clin Cancer Res, 23(12):3012–3024. https://doi.org/10.1158/1078-0432.Ccr-16-2554
Eisenhauer EA, Therasse P, Bogaerts J, et al., 2009. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer, 45(2):228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Eudy JD, Weston MD, Yao SF, et al., 1998. Mutation of a gene encoding a protein with extracellular matrix motifs in Usher syndrome type IIa. Science, 280(5370):1753–1757. https://doi.org/10.1126/science.280.5370.1753
Fang WF, Ma YX, Yin JC, et al., 2019. Comprehensive genomic profiling identifies novel genetic predictors of response to anti-PD- (L)1 therapies in non-small cell lung cancer. Clin Cancer Res, 25(16):5015–5026. https://doi.org/10.1158/1078-0432.Ccr-19-0585
Fang WF, Jin HX, Zhou HQ, et al., 2021. Intratumoral heterogeneity as a predictive biomarker in anti-PD-(L)1 therapies for non-small cell lung cancer. Mol Cancer, 20:37. https://doi.org/10.1186/s12943-021-01331-9
Frigola J, Navarro A, Carbonell C, et al., 2021. Molecular profiling of long-term responders to immune checkpoint inhibitors in advanced non-small cell lung cancer. Mol Oncol, 15(4):887–900. https://doi.org/10.1002/1878-0261.12891
Gainor JF, Shaw AT, Sequist LV, et al., 2016. EGFR mutations and ALK rearrangements are associated with low response rates to PD-1 pathway blockade in non-small cell lung cancer: a retrospective analysis. Clin Cancer Res, 22(18):4585–4593. https://doi.org/10.1158/1078-0432.Ccr-15-3101
Gandara DR, Paul SM, Kowanetz M, et al., 2018. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat Med, 24(9):1441–1448. https://doi.org/10.1038/s41591-018-0134-3
Gao G, Liao WT, Ma QZ, et al., 2020. KRAS G12D mutation predicts lower TMB and drives immune suppression in lung adenocarcinoma. Lung Cancer, 149:41–45. https://doi.org/10.1016/j.lungcan.2020.09.004
Gu ZG, Eils R, Schlesner M, 2016. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics, 32(18):2847–2849. https://doi.org/10.1093/bioinformatics/btw313
Gao ZR, Ling XY, Shi CY, et al., 2022. Tumor immune checkpoints and their associated inhibitors. J Zhejiang Univ-Sci B (Biomed & Biotechnol), 23(10):823–843. https://doi.org/10.1631/jzus.B2200195
Hastings K, Yu HA, Wei W, et al., 2019. EGFR mutation subtypes and response to immune checkpoint blockade treatment in non-small-cell lung cancer. Ann Oncol, 30(8): 1311–1320. https://doi.org/10.1093/annonc/mdz141
Hata A, Katakami N, Nanjo S, et al., 2017. Programmed death-ligand 1 expression and T790M status in EGFR-mutant non-small cell lung cancer. Lung Cancer, 111: 182–189. https://doi.org/10.1016/j.lungcan.2017.07.022
Hellmann MD, Nathanson T, Rizvi H, et al., 2018. Genomic features of response to combination immunotherapy in patients with advanced non-small-cell lung cancer. Cancer Cell, 33(5):843–852.e4. https://doi.org/10.1016/j.ccell.2018.03.018
Jeanson A, Tomasini P, Souquet-Bressand M, et al., 2019. Efficacy of immune checkpoint inhibitors in KRAS-mutant non-small cell lung cancer (NSCLC). J Thorac Oncol, 14(6):1095–1101. https://doi.org/10.1016/j.jtho.2019.01.011
Jia QZ, Wang J, He N, et al., 2019. Titin mutation associated with responsiveness to checkpoint blockades in solid tumors. JCI Insight, 4(10):e127901. https://doi.org/10.1172/jci.insight.127901
Jia QZ, Chiu L, Wu SX, et al., 2020. Tracking neoantigens by personalized circulating tumor DNA sequencing during checkpoint blockade immunotherapy in non-small cell lung cancer. Adv Sci (Weinh), 7(9):1903410. https://doi.org/10.1002/advs.201903410
Kumagai S, Koyama S, Nishikawa H, 2021. Antitumour immunity regulated by aberrant ERBB family signalling. Nat Rev Cancer, 21(3):181–197. https://doi.org/10.1038/s41568-020-00322-0
Lee CK, Man J, Lord S, et al., 2017. Checkpoint inhibitors in metastatic EGFR-mutated non-small cell lung cancer—a meta-analysis. J Thorac Oncol, 12(2):403–407. https://doi.org/10.1016/j.jtho.2016.10.007
Liu CM, Zheng SF, Jin RS, et al., 2020. The superior efficacy of anti-PD-1/PD-L1 immunotherapy in KRAS-mutant non-small cell lung cancer that correlates with an inflammatory phenotype and increased immunogenicity. Cancer Lett, 470:95–105. https://doi.org/10.1016/j.canlet.2019.10.027
Mazieres J, Drilon A, Lusque A, et al., 2019. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann Oncol, 30(8):1321–1328. https://doi.org/10.1093/annonc/mdz167
Miao DN, Margolis CA, Vokes NI, et al., 2018. Genomic correlates of response to immune checkpoint blockade in microsatellite-stable solid tumors. Nat Genet, 50(9): 1271–1281. https://doi.org/10.1038/s41588-018-0200-2
Moding EJ, Liu YF, Nabet BY, et al., 2020. Circulating tumor DNA dynamics predict benefit from consolidation immunotherapy in locally advanced non-small-cell lung cancer. Nat Cancer, 1(2):176–183. https://doi.org/10.1038/s43018-019-0011-0
Oscanoa J, Sivapalan L, Gadaleta E, et al., 2020. SNPnexus: a web server for functional annotation of human genome sequence variation (2020 update). Nucleic Acids Res, 48(W1):W185–W192. https://doi.org/10.1093/nar/gkaa420
Pender A, Titmuss E, Pleasance ED, et al., 2021. Genome and transcriptome biomarkers of response to immune checkpoint inhibitors in advanced solid tumors. Clin Cancer Res, 27(1):202–212. https://doi.org/10.1158/1078-0432.Ccr-20-1163
Peng DJ, Kryczek I, Nagarsheth N, et al., 2015. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature, 527(7577):249–253. https://doi.org/10.1038/nature15520
Reuss JE, Anagnostou V, Cottrell TR, et al., 2020. Neoadjuvant nivolumab plus ipilimumab in resectable non-small cell lung cancer. J Immunother Cancer, 8(2):e001282. https://doi.org/10.1136/jitc-2020-001282
Rivolta C, Berson EL, Dryja TP, 2002. Paternal uniparental heterodisomy with partial isodisomy of chromosome 1 in a patient with retinitis pigmentosa without hearing loss and a missense mutation in the Usher syndrome type II gene USH2A. Arch Ophthalmol, 120(11):1566–1571. https://doi.org/10.1001/archopht.120.11.1566
Rizvi H, Sanchez-Vega F, La K, et al., 2018. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung cancer profiled with targeted next-generation sequencing. J Clin Oncol, 36(7): 633–641. https://doi.org/10.1200/jco.2017.75.3384
Rizvi NA, Hellmann MD, Snyder A, et al., 2015. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science, 348(6230):124–128. https://doi.org/10.1126/science.aaa1348
Sabapathy K, Lane DP, 2018. Therapeutic targeting of p53: all mutants are equal, but some mutants are more equal than others. Nat Rev Clin Oncol, 15(1):13–30. https://doi.org/10.1038/nrclinonc.2017.151
Samstein RM, Lee CH, Shoushtari AN, et al., 2019. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet, 51 (2):202–206. https://doi.org/10.1038/s41588-018-0312-8
Sequist LV, Waltman BA, Dias-Santagata D, et al., 2011. Genotypic and histological evolution of lung cancers acquiring resistance to egfr inhibitors. Sci Transl Med, 3(75):75ra26. https://doi.org/10.1126/scitranslmed.3002003
Steven A, Fisher SA, Robinson BW, 2016. Immunotherapy for lung cancer. Respirology, 21(5):821–833. https://doi.org/10.1111/resp.12789
Sugiyama E, Togashi Y, Takeuchi Y, et al., 2020. Blockade of EGFR improves responsiveness to PD-1 blockade in EGFR-mutated non-small cell lung cancer. Sci Immunol, 5(43):eaav3937. https://doi.org/10.1126/sciimmunol.aav3937
Sun H, Liu SY, Zhou JY, et al., 2020. Specific TP53 subtype as biomarker for immune checkpoint inhibitors in lung adenocarcinoma. EBioMedicine, 60:102990. https://doi.org/10.1016/j.ebiom.2020.102990
Sun YY, Li L, Yao WC, et al., 2021. USH2A mutation is associated with tumor mutation burden and antitumor immunity in patients with colon adenocarcinoma. Front Genet, 12:762160. https://doi.org/10.3389/fgene.2021.762160
Szolek A, Schubert B, Mohr C, et al., 2014. OptiType: precision HLA typing from next-generation sequencing data. Bioinformatics, 30(23):3310–3316. https://doi.org/10.1093/bioinformatics/btu548
Talevich E, Shain AH, Botton T, et al., 2016. CNVkit: genome-wide copy number detection and visualization from targeted DNA sequencing. PLoS Comput Biol, 12(4): e1004873. https://doi.org/10.1371/journal.pcbi.1004873
Toualbi L, Toms M, Moosajee M, 2020. USH2A-retinopathy: from genetics to therapeutics. Exp Eye Res, 201:108330. https://doi.org/10.1016/j.exer.2020.108330
Tsao MS, Kerr KM, Kockx M, et al., 2018. PD-L1 immunohistochemistry comparability study in real-life clinical samples: results of blueprint phase 2 project. J Thorac Oncol, 13(9): 1302–1311. https://doi.org/10.1016/j.jtho.2018.05.013
Weston MD, Eudy JD, Fujita S, et al., 2000. Genomic structure and identification of novel mutations in Usherin, the gene responsible for Usher syndrome type IIa. Am J Hum Genet, 66(4): 1199–1210. https://doi.org/10.1086/302855
Wu SG, Shih JY, 2018. Management of acquired resistance to EGFR TKI-targeted therapy in advanced non-small cell lung cancer. Mol Cancer, 17:38. https://doi.org/10.1186/s12943-018-0777-1
Yarchoan M, Hopkins A, Jaffee EM, 2017. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med, 377(25):2500–2501. https://doi.org/10.1056/NEJMc1713444
Yu HA, Arcila ME, Rekhtman N, et al., 2013. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res, 19(8):2240–2247. https://doi.org/10.1158/1078-0432.Ccr-12-2246
Yu YF, Lin DG, Li AL, et al., 2020. Association of immune checkpoint inhibitor therapy with survival in patients with cancers with MUC16 variants. JAMA Netw Open, 3(6): e205837. https://doi.org/10.1001/jamanetworkopen.2020.5837
Zhang L, Han XH, Shi YK, 2020. Association of MUC16 mutation with response to immune checkpoint inhibitors in solid tumors. JAMA Netw Open, 3(8):e2013201. https://doi.org/10.1001/jamanetworkopen.2020.13201
Zhu GS, Ren D, Lei X, et al., 2021. Mutations associated with no durable clinical benefit to immune checkpoint blockade in non-s-cell lung cancer. Cancers (Basel), 13(6): 1397. https://doi.org/10.3390/cancers13061397
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Nos. 21976155, 81802881, and 81773016), the Zhejiang Provincial Natural Science Foundation of China (No. LY18C060001), the Fundamental Research Funds for the Central Universities, and the Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (CIFMS) (No. 2019-I2M-5-044), China.
Author information
Authors and Affiliations
Contributions
Yihua WU and Dajing XIA contributed to the conception and design of the study. Yihua WU, Dexin YANG, and Yuqin FENG developed the workflow and methodology. Dexin YANG, Yuqin FENG, Haohua LU, Kelie CHEN, Jinming XU, Peiwei LI, and Tianru WANG contributed to data collection, data analysis, and interpretation. Yuqin FENG, Dexin YANG, Yihua WU, and Dajing XIA contributed to writing and review of the manuscript. All authors have read and approved the final manuscript, and therefore, have full access to all the data in the study and take responsibility for the integrity and security of the data.
Corresponding authors
Ethics declarations
Dexin YANG, Yuqin FENG, Haohua LU, Kelie CHEN, Jinming XU, Peiwei LI, Tianru WANG, Dajing XIA, and Yihua WU declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Supplementary information
Figs. S1–S8; Tables S1–S8
Supplementary Information
Rights and permissions
About this article
Cite this article
Yang, D., Feng, Y., Lu, H. et al. USH2A mutation and specific driver mutation subtypes are associated with clinical efficacy of immune checkpoint inhibitors in lung cancer. J. Zhejiang Univ. Sci. B 24, 143–156 (2023). https://doi.org/10.1631/jzus.B2200292
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B2200292
Key words
- Immune checkpoint inhibitor (ICI)
- Lung cancer
- Usher syndrome type-2A (USH2A) missense mutation
- Kirsten rat sarcoma viral oncogene homolog G12C (KRAS 12C) mutation combined with tumor protein P53 (TP53) mutation
- Epidermal growth factor receptor (EGFR) mutation