Abstract
Biomaterials used in bone tissue engineering should mimic the pore characteristics and micro-architectural features of bone to facilitate successful regeneration and repair of damaged tissue in vivo. The complete qualitative and quantitative analysis of pore characteristics in tissue engineering scaffolds remains a challenge. Compared to the other traditional methods, micro-tomography is a reliable, efficient, and non-destructive technique to assess micro-architectural characteristics in scaffolds. In this study, composite scaffolds comprising natural polymers (alginate, gelatin and chitosan) reinforced with glass–ceramic powder was fabricated using the freeze-drying technique. The micro-architectural features were analyzed with quantification of different parameters—pore size, pore shape, pore orientation, pore interconnectivity and fractal analysis. The scaffolds exhibited macro-porosity with good pore architecture and connectivity. The quantification of different parameters yielded promising results and micro-tomography proves to be an efficient tool for analyzing and quantifying pore characteristics in bone tissue engineering scaffolds.
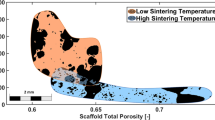
Graphical abstract







Similar content being viewed by others
Data availability
The data used for the study are included within the article.
References
P.X. Ma, Scaffolds for tissue fabrication. Mater. Today 7, 30–40 (2004). https://doi.org/10.1016/S1369-7021(04)00233-0
K.J.L. Burg, S. Porter, J.F. Kellam, Biomaterial developments for bone tissue engineering. Biomaterials 21, 2347–2359 (2000). https://doi.org/10.1016/S0142-9612(00)00102-2
L.L. Hench, J.M. Polak, Third-generation biomedical materials. Science (80-) (2002). https://doi.org/10.1126/science.1067404
A.I. Caplan, V.M. Goldberg, Principles of tissue engineered regeneration of skeletal tissues. Clin. Orthop. Relat. Res. (1999). https://doi.org/10.1097/00003086-199910001-00003
V. Karageorgiou, D. Kaplan, Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26, 5474–5491 (2005). https://doi.org/10.1016/j.biomaterials.2005.02.002
T. Russo, A. Gloria, V. D’Antò, U. D’Amora, G. Ametrano, F. Bollino, R. De Santis, G. Ausanio, M. Catauro, S. Rengo, L. Ambrosio, Poly(ε-caprolactone) reinforced with sol-gel synthesized organic-inorganic hybrid fillers as composite substrates for tissue engineering. J. Appl. Biomater. Biomech. 8, 146–152 (2010). https://doi.org/10.5301/JABB.2010.6094
A.S.P. Lin, T.H. Barrows, S.H. Cartmell, R.E. Guldberg, Microarchitectural and mechanical characterization of oriented porous polymer scaffolds. Biomaterials 24, 481–489 (2003). https://doi.org/10.1016/S0142-9612(02)00361-7
V. Guarino, F. Causa, L. Ambrosio, Porosity and mechanical properties relationship in PCL porous scaffolds. J. Appl. Biomater. Biomech. 5, 149–157 (2007). https://doi.org/10.1177/228080000700500303
J. Wu, Q. Zhao, J. Sun, Q. Zhou, Preparation of poly(ethylene glycol) aligned porous cryogels using a unidirectional freezing technique. Soft Matter 8, 3620–3626 (2012). https://doi.org/10.1039/c2sm07411g
M. Costantini, C. Colosi, P. Mozetic, J. Jaroszewicz, A. Tosato, A. Rainer, M. Trombetta, W. Więszkowski, M. Dentini, A. Barbetta, Correlation between porous texture and cell seeding efficiency of gas foaming and microfluidic foaming scaffolds. Mater. Sci. Eng. C 62, 668–677 (2016). https://doi.org/10.1016/j.msec.2016.02.010
J.S. Kaiser, M. Kamperman, E.J. de Souza, B. Schick, E. Arzt, Adhesion of biocompatible and biodegradable micropatterned surfaces. Int. J. Artif. Organs 34, 180–184 (2011). https://doi.org/10.5301/IJAO.2011.6393
S. Bertoldi, S. Farè, M.C. Tanzi, Assessment of scaffold porosity: The new route of micro-CT. J. Appl. Biomater. Biomech. 9, 165–175 (2011). https://doi.org/10.5301/JABB.2011.8863
M. Bartoš, T. Suchý, R. Foltán, Note on the use of different approaches to determine the pore sizes of tissue engineering scaffolds: What do we measure? Biomed. Eng. (2018). https://doi.org/10.1186/s12938-018-0543-z
F. Peyrin, Evaluation of bone scaffolds by micro-CT, in: Osteoporos. Int., 2011: pp. 2043–2048. https://doi.org/10.1007/s00198-011-1609-y.
S.T. Ho, D.W. Hutmacher, A comparison of micro CT with other techniques used in the characterization of scaffolds. Biomaterials 27, 1362–1376 (2006). https://doi.org/10.1016/j.biomaterials.2005.08.035
J.R. Jones, R.C. Atwood, G. Poologasundarampillai, S. Yue, P.D. Lee, Quantifying the 3D macrostructure of tissue scaffolds, in: J. Mater. Sci. Mater. Med., 2009: pp. 463–471. https://doi.org/10.1007/s10856-008-3597-9.
F. Beltrame, R. Cancedda, B. Canesi, A. Crovace, M. Mastrogiacomo, R. Quarto, S. Scaglione, C. Valastro, F. Viti, A simple non invasive computerized method for the assessment of bone repair within osteoconductive porous bioceramic grafts. Biotechnol. Bioeng. 92, 189–198 (2005). https://doi.org/10.1002/bit.20591
N. Kotobuki, K. Ioku, D. Kawagoe, H. Fujimori, S. Goto, H. Ohgushi, Observation of osteogenic differentiation cascade of living mesenchymal stem cells on transparent hydroxyapatite ceramics. Biomaterials 26, 779–785 (2005). https://doi.org/10.1016/j.biomaterials.2004.03.020
C. Vitale-Brovarone, S. Di Nunzio, O. Bretcanu, E. Verné, Macroporous glass-ceramic materials with bioactive properties. J. Mater. Sci. Mater. Med. 15, 209–217 (2004). https://doi.org/10.1023/B:JMSM.0000015480.49061.e1
D.J. Mooney, D.F. Baldwin, N.P. Suh, J.P. Vacanti, R. Langer, Novel approach to fabricate porous sponges of poly(D, L-lactic-co-glycolic acid) without the use of organic solvents. Biomaterials (1996). https://doi.org/10.1016/0142-9612(96)87284-X
S.G. Kumbar, C. Laurencin, M. Deng, Natural and Synthetic Biomedical Polymers (Elsevier, Amsterdam, 2014)
J. Sun, H. Tan, Alginate-based biomaterials for regenerative medicine applications. Materials (Basel). 6, 1285–1309 (2013). https://doi.org/10.3390/ma6041285
M.C. Echave, L.S. Burgo, J.L. Pedraz, G. Orive, Gelatin as biomaterial for tissue engineering. Curr. Pharm. Des. 23, 3567–3584 (2017). https://doi.org/10.2174/0929867324666170511123101
I.Y. Kim, S.J. Seo, H.S. Moon, M.K. Yoo, I.Y. Park, B.C. Kim, C.S. Cho, Chitosan and its derivatives for tissue engineering applications. Biotechnol. Adv. 26, 1–21 (2008). https://doi.org/10.1016/j.biotechadv.2007.07.009
A.R. Boccaccini, C. Fleck, D.W. Schubert, J.A. Roether, A. Philippart, A.R. Boccaccini, C. Fleck, D.W. Schubert, J.A. Roether, Toughening and functionalization of bioactive ceramic and glass bone scaffolds by biopolymer coatings and infiltration: A review of the last 5 years. Expert Rev. Med. Devices 12, 93–111 (2014). https://doi.org/10.1586/17434440.2015.958075
Q. Hou, D.W. Grijpma, J. Feijen, Preparation of interconnected highly porous polymeric structures by a replication and freeze-drying process. J. Biomed. Mater. Res. Part B (2003). https://doi.org/10.1002/jbm.b.10066
M.K. Narbat, F. Orang, M.S. Hashtjin, A. Goudarzi, Fabrication of porous hydroxyapatite-gelatin composite scaffolds for bone tissue engineering. Iran. Biomed. J. 10, 215–223 (2006)
D.W. Hutmacher, Scaffolds in tissue engineering bone and cartilage. Biomaterials 21, 2529–2543 (2000). https://doi.org/10.1016/S0142-9612(00)00121-6
S.J. Hollister, Porous scaffold design for tissue engineering. Nat. Mater. 4, 518–524 (2005). https://doi.org/10.1038/nmat1421
Y. Kuboki, Q. Jin, H. Takita, Geometry of carriers controlling phenotypic expression in BMP-induced osteogenesis and chondrogenesis. J. Bone Jt. Surg. Am. 83 A Suppl, S101–S105 (2001)
E. Tsuruga, H. Takita, H. Itoh, Y. Wakisaka, Y. Kuboki, Pore size of porous hydroxyapatite as the cell-substratum controls BMP-induced osteogenesis. J. Biochem. 121, 317–324 (1997). https://doi.org/10.1093/oxfordjournals.jbchem.a021589
E.C. Shors, Coralline bone graft substitutes. Orthop. Clin. North Am. 30, 599–613 (1999). https://doi.org/10.1016/S0030-5898(05)70113-9
B.N. Singh, V. Veeresh, S.P. Mallick, S. Sinha, A. Rastogi, P. Srivastava, Generation of scaffold incorporated with nanobioglass encapsulated in chitosan/chondroitin sulfate complex for bone tissue engineering. Int. J. Biol. Macromol. (2020). https://doi.org/10.1016/j.ijbiomac.2020.02.173
F. Polyak, G. Reich, Infrared spectroscopic study of the coil-helix transition of highly concentrated gelatin formulations. Eur. J. Pharm. Biopharm. (2019). https://doi.org/10.1016/j.ejpb.2019.04.010
F. Milano, A. Masi, M. Madaghiele, A. Sannino, L. Salvatore, N. Gallo, Current trends in gelatin-based drug delivery systems. Pharmaceutics (2023). https://doi.org/10.3390/pharmaceutics15051499
C.S. Julie Chandra, S. Sasi, T.K. Bindu Sharmila, Material Applications of Gelatin, in: Handb. Biopolym., 2023. https://doi.org/10.1007/978-981-16-6603-2_28-1.
S. Van Vlierberghe, G.J. Graulus, S.K. Samal, I. Van Nieuwenhove, P. Dubruel, Porous hydrogel biomedical foam scaffolds for tissue repair. Biomed. Foam. Tissue Eng. Appl. (2014). https://doi.org/10.1533/9780857097033.2.335
P. Rivero-Ramos, M.G. Unthank, T. Sanz, M.D. Rodrigo, M. Benlloch-Tinoco, Synergistic depolymerisation of alginate and chitosan by high hydrostatic pressure (HHP) and pulsed electric fields (PEF) treatment in the presence of H2O2. Carbohydr. Polym. (2023). https://doi.org/10.1016/j.carbpol.2023.120999
M.I. Gariboldi, S.M. Best, Effect of ceramic scaffold architectural parameters on biological response. Front. Bioeng. Biotechnol. (2015). https://doi.org/10.3389/fbioe.2015.00151
G. Hannink, J.J.C. Arts, Bioresorbability, porosity and mechanical strength of bone substitutes: What is optimal for bone regeneration? Injury 42, S22–S25 (2011). https://doi.org/10.1016/j.injury.2011.06.008
S.K. Lan Levengood, S.J. Polak, M.B. Wheeler, A.J. Maki, S.G. Clark, R.D. Jamison, A.J. Wagoner Johnson, Multiscale osteointegration as a new paradigm for the design of calcium phosphate scaffolds for bone regeneration. Biomaterials 31, 3552–3563 (2010). https://doi.org/10.1016/j.biomaterials.2010.01.052
C.M. Murphy, M.G. Haugh, F.J. O’Brien, The effect of mean pore size on cell attachment, proliferation and migration in collagen-glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials 31, 461–466 (2010). https://doi.org/10.1016/j.biomaterials.2009.09.063
F.J. O’Brien, B.A. Harley, I.V. Yannas, L.J. Gibson, The effect of pore size on cell adhesion in collagen-GAG scaffolds. Biomaterials 26, 433–441 (2005). https://doi.org/10.1016/j.biomaterials.2004.02.052
S. Srinivasan, R. Jayasree, K.P.P. Chennazhi, S.V.V. Nair, R. Jayakumar, Biocompatible alginate/nano bioactive glass ceramic composite scaffolds for periodontal tissue regeneration. Carbohydr. Polym. 87, 274–283 (2012). https://doi.org/10.1016/j.carbpol.2011.07.058
H.W. Kim, J.C. Knowles, H.E. Kim, Hydroxyapatite and gelatin composite foams processed via novel freeze-drying and crosslinking for use as temporary hard tissue scaffolds. J. Biomed. Mater. Res. Part A 72, 136–145 (2005). https://doi.org/10.1002/jbm.a.30168
K. Maji, S. Dasgupta, B. Kundu, A. Bissoyi, Development of gelatin-chitosan-hydroxyapatite based bioactive bone scaffold with controlled pore size and mechanical strength. J. Biomater. Sci. Polym. Ed. 26, 1190–1209 (2015). https://doi.org/10.1080/09205063.2015.1082809
K. Maji, S. Dasgupta, K. Pramanik, A. Bissoyi, Preparation and evaluation of gelatin-chitosan-nanobioglass 3D porous scaffold for bone tissue engineering. Int. J. Biomater. (2016). https://doi.org/10.1155/2016/9825659
Y. Xu, J. Guan, Interaction of Cells with Polyurethane Scaffolds, in: Adv. Polyurethane Biomater., 2016: pp. 523–542. https://doi.org/10.1016/B978-0-08-100614-6.00018-4.
E.H. Macdonald, Sedimentation and detrital gold, in: Handb. Gold Explor. Eval., 2007: pp. 195–266. https://doi.org/10.1533/9781845692544.195.
C.M. Nelson, R.P. Jean, J.L. Tan, W.F. Liu, N.J. Sniadecki, A.A. Spector, C.S. Chen, Emergent patterns of growth controlled by multicellular form and mechanics. Proc. Natl. Acad. Sci. U.S.A. 102, 11594–11599 (2005). https://doi.org/10.1073/pnas.0502575102
D. Veljović, R. Jančić-Hajneman, I. Balać, B. Jokić, S. Putić, R. Petrović, D. Janaćković, The effect of the shape and size of the pores on the mechanical properties of porous HAP-based bioceramics. Ceram. Int. 37, 471–479 (2011). https://doi.org/10.1016/j.ceramint.2010.09.014
M. Nacucchi, F. De Pascalis, M. Scatto, L. Capodieci, R. Albertoni, Structural analysis of advanced polymeric foams by means of high resolution X-ray computed tomography. AIP Conf. Proc. (2016). https://doi.org/10.1063/1.4954492
M.S. Rizvi, P. Kumar, D.S. Katti, A. Pal, Mathematical model of mechanical behavior of micro/nanofibrous materials designed for extracellular matrix substitutes. Acta Biomater. 8, 4111–4122 (2012). https://doi.org/10.1016/j.actbio.2012.07.025
G.C. Engelmayr, G.D. Papworth, S.C. Watkins, J.E. Mayer, M.S. Sacks, Guidance of engineered tissue collagen orientation by large-scale scaffold microstructures. J. Biomech. 39, 1819–1831 (2006). https://doi.org/10.1016/j.jbiomech.2005.05.020
B.B. Mandal, E.S. Gil, B. Panilaitis, D.L. Kaplan, Laminar silk scaffolds for aligned tissue fabrication. Macromol. Biosci. 13, 48–58 (2013). https://doi.org/10.1002/mabi.201200230
K.S. Halonen, M.E. Mononen, J.S. Jurvelin, J. Töyräs, R.K. Korhonen, Importance of depth-wise distribution of collagen and proteoglycans in articular cartilage-A 3D finite element study of stresses and strains in human knee joint. J. Biomech. 46, 1184–1192 (2013). https://doi.org/10.1016/j.jbiomech.2012.12.025
A. Arora, A. Kothari, D.S. Katti, Pore orientation mediated control of mechanical behavior of scaffolds and its application in cartilage-mimetic scaffold design. J. Mech. Behav. Biomed. Mater. 51, 169–183 (2015). https://doi.org/10.1016/j.jmbbm.2015.06.033
S. Blacher, V. Maquet, R. Jérôme, J.P. Pirard, A.R. Boccaccini, Study of the connectivity properties of Bioglass®-filled polylactide foam scaffolds by image analysis and impedance spectroscopy. Acta Biomater. 1, 565–574 (2005). https://doi.org/10.1016/j.actbio.2005.06.003
K.F. Leong, C.M. Cheah, C.K. Chua, Solid freeform fabrication of three-dimensional scaffolds for engineering replacement tissues and organs. Biomaterials 24, 2363–2378 (2003). https://doi.org/10.1016/S0142-9612(03)00030-9
S.L. Ishaug-Riley, G.M. Crane-Kruger, M.J. Yaszemski, A.G. Mikos, Three-dimensional culture of rat calvarial osteoblasts in porous biodegradable polymers. Biomaterials 19, 1405–1412 (1998). https://doi.org/10.1016/S0142-9612(98)00021-0
A. Odgaard, H.J.G. Gundersen, Quantification of connectivity in cancellous bone, with special emphasis on 3-D reconstructions. Bone 14, 173–182 (1993). https://doi.org/10.1016/8756-3282(93)90245-6
L. Brabant, J. Vlassenbroeck, Y. De Witte, V. Cnudde, M.N. Boone, J. Dewanckele, L. Van Hoorebeke, Three-dimensional analysis of high-resolution X-ray computed tomography data with morpho+. Microsc. Microanal. 17, 252–263 (2011). https://doi.org/10.1017/S1431927610094389
C.H. Arns, M.A. Knackstedt, W.V. Pinczewski, K.R. Mecke, Euler-Poincaré characteristics of classes of disordered media. Phys. Rev. E 63, 311121–3111213 (2001). https://doi.org/10.1103/PhysRevE.63.031112
S. Anuradha, K. Uma Maheswari, S. Swaminathan, Fabrication of uniaxially aligned 3D electrospun scaffolds for neural regeneration. Biomed. Mater. 6, 25004 (2011)
K. Stuckensen, A. Schwab, M. Knauer, E. Muiños-López, F. Ehlicke, J. Reboredo, F. Granero-Moltó, U. Gbureck, F. Prósper, H. Walles, J. Groll, Tissue mimicry in morphology and composition promotes hierarchical matrix remodeling of invading stem cells in osteochondral and meniscus scaffolds. Adv. Mater. (2018). https://doi.org/10.1002/adma.201706754
P. Tayalia, C.R. Mendonca, T. Baldacchini, D.J. Mooney, E. Mazur, 3D cell-migration studies using two-photon engineered polymer scaffolds. Adv. Mater. 20, 4494–4498 (2008). https://doi.org/10.1002/adma.200801319
C.H. Lee, H.J. Shin, I.H. Cho, Y.M. Kang, I.A. Kim, K.D. Park, J.W. Shin, Nanofiber alignment and direction of mechanical strain affect the ECM production of human ACL fibroblast. Biomaterials 26, 1261–1270 (2005). https://doi.org/10.1016/j.biomaterials.2004.04.037
K. Stuckensen, J.M. Lamo-Espinosa, E. Muiños-López, P. Ripalda-Cemboráin, T. López-Martínez, E. Iglesias, G. Abizanda, I. Andreu, M. Flandes-Iparraguirre, J. Pons-Villanueva, R. Elizalde, J. Nickel, A. Ewald, U. Gbureck, F. Prósper, J. Groll, F. Granero-Moltó, Anisotropic cryostructured collagen scaffolds for efficient delivery of RhBMP-2 and enhanced bone regeneration. Materials (Basel) (2019). https://doi.org/10.3390/ma12193105
I. Sánchez, G. Uzcátegui, Fractals in dentistry. J. Dent. 39, 273–292 (2011). https://doi.org/10.1016/j.jdent.2011.01.010
J. Guédon, F. Autrusseau, Y. Amouriq, P. Bléry, J.-M. Bouler, P. Weiss, F.-X. Barbarin, T. Dallet, V. Dallerit, Exploring relationships between fractal dimension and trabecular bone characteristics, in: Med. Imaging 2012 Biomed. Appl. Mol. Struct. Funct. Imaging 2012: p. 831717. https://doi.org/10.1117/12.911164.
D. Ulrich, B. van Rietbergen, A. Laib, P. R̈uegsegger, The ability of three-dimensional structural indices to reflect mechanical aspects of trabecular bone. Bone 25, 55–60 (1999). https://doi.org/10.1016/S8756-3282(99)00098-8
J.L. Drummond, M. Thompson, B.J. Super, Fracture surface examination of dental ceramics using fractal analysis. Dent. Mater. 21, 586–589 (2005). https://doi.org/10.1016/j.dental.2004.12.002
J.J. Mecholsky, D.E. Passoja, K.S. Feinberg-Ringel, Quantitative analysis of brittle fracture surfaces using fractal geometry. J. Am. Ceram. Soc. 72, 60–65 (1989). https://doi.org/10.1111/j.1151-2916.1989.tb05954.x
T. Uchiyama, T. Tanizawa, H. Muramatsu, N. Endo, H.E. Takahashi, T. Hara, Three-dimensional microstructural analysis of human trabecular bone in relation to its mechanical properties. Bone 25, 487–491 (1999). https://doi.org/10.1016/S8756-3282(99)00188-X
A. Thomas, J. Bera, Sol–gel synthesis and in vitro bioactivity of glass–ceramics in SiO2–CaO–Na2O–P2O5 system. J. Sol-Gel Sci. Technol. 80, 411–416 (2016). https://doi.org/10.1007/s10971-016-4110-4
A. Thomas, J. Bera, Preparation and characterization of gelatin-bioactive glass ceramic scaffolds for bone tissue engineering. J. Biomater. Sci. Polym. Ed. 30, 1–19 (2019). https://doi.org/10.1080/09205063.2019.1587697
A. Thomas, E. Johnson, A.K. Agrawal, J. Bera, Preparation and characterization of glass-ceramic reinforced alginate scaffolds for bone tissue engineering. J. Mater. Res. 34, 3798–3809 (2019). https://doi.org/10.1557/jmr.2019.343
Acknowledgments
The authors would like to thank RRCAT, Indore for providing experimental facility
Funding
This research received no specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
AT was involved in conceptualization, study design and execution of the work. AA and YSK were involved in data acquisition, analysis and interpretation. I PK and JB were involved in data validation and critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thomas, A., Agarwal, A.K., Kashyap, Y.S. et al. Quantifying pore characteristics in polymer glass–ceramics composite scaffolds using micro-tomography. Journal of Materials Research 39, 1258–1272 (2024). https://doi.org/10.1557/s43578-024-01307-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/s43578-024-01307-7