Abstract
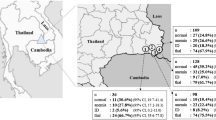
Samples from 916 members of various ethnic groups from malaria-endemic southern Shan State, Myanmar, were analyzed for α-thalassemia (α-thal), β -thalassemia (β -thal), abnormal hemoglobin variants, and glucose-6-phosphate dehydrogenase (G6PD) deficiency. Of these subjects, 530 (57.9%) were found to have at least one of these red cell genetic disorders.The overall frequencies for the various red cell genetic disorders were as follows: α-thal, 37.5% (343/916); hemoglobin E (Hb-E), 20.3% (186/916); G6PD-Mahidol, 17.5% (160/916); and β-thal, 0.3% (3/916). The frequencies of combined disorders were 6.9% (63/ 916) for α-thal/Hb-E, 5.7% (52/916) for α-thal/G6PD-Mahidol, 2.8% (26/916) for Hb-E/G6PD-Mahidol, 1.1% (10/916) for α-thal/Hb-E/G6PD-Mahidol, and 0.1% (1/916) for α-thal/β-thal/G6PD-Mahidol. Of the various ethnic and non-ethnic groups, the Bamar population showed the highest frequencies of α-thal (56.9%, 177/311), Hb-E (28.3%, 88/311), and G6PD-Mahidol (21.2%, 66/311) (all duplicated and triplicated cases were included). In addition, 2 new mutations, an a gene triplication (/αααanti3.7; 0.2%, 2/916) and Hb-Neapolis (0.1%, 1/916), were detected. Our results showed that race was the dominant factor affecting the frequencies of red cell genetic disorders in malaria-endemic areas of Myanmar.
Similar content being viewed by others
References
Badens C, Martinez di Montemuros F, Thuret I, et al. Molecular basis of haemoglobinopathies and G6PD deficiency in the Comorian population.Hematol J. 2000;1:264–268.
Weatherall DJ. Thalassemia in the next millennium: keynote address.Ann N Y Acad Sci. 1998;850:1–9.
Iwai K, Hirono A, Matsuoka H, et al. Distribution of glucose-6- phosphate dehydrogenase mutations in Southeast Asia.Hum Genet. 2001;108:445–449.
Matsuoka H, Wang J, Hirai M, et al. Glucose-6-phosphate dehydrogenase (G6PD) mutations in Myanmar: G6PD Mahidol (487G>A) is the most common variant in the Myanmar population.J Hum Genet. 2004;49:544–547.
Old JM, Varawalla NY, Weatherall DJ. Rapid detection and prenatal diagnosis of beta-thalassaemia: studies in Indian and Cypriot populations in the UK.Lancet. 1990;336:834–837.
Varawalla NY, Old JM, Sarkar R, Venkatesan R, Weatherall DJ. The spectrum of beta-thalassaemia mutations on the Indian subcontinent: the basis for prenatal diagnosis.Br J Haematol. 1991;78:242–247.
Brown JM, Thein SL, Weatherall DJ, Mar KM. The spectrum of beta thalassaemia in Burma.Br J Haematol. 1992;81:574–578.
Than AM, Harano T, Harano K, Okada S. Hemoglobinopathies and malaria infection in Myanmar.Kawasaki Med J. 2002;28:9–15.
Chong SS, Boehm CD, Higgs DR, Cutting GR. Single-tube multiplex- PCR screen for common deletional determinants of α-thalassemia.Blood. 2000;95:360–362.
Liu YT, Old JM, Miles K, Fisher CA, Weatherall DJ, Clegg JB. Rapid detection of α-thalassaemia deletions and α-globin gene triplication by multiplex polymerase chain reactions.Br J Haematol.. 2000;108:295–299.
Huang CS, Hung KL, Huang MJ, Li YC, Liu TH, Tang TK. Neonatal jaundice and molecular mutations in glucose-6-phosphate dehydrogenase deficient newborn infants.Am J Hematol. 1996;51:19–25.
Nuchprayoon I, Sanpavat S, Nuchprayoon S. Glucose-6-phosphate dehydrogenase (G6PD) mutations in Thailand: G6PD Viangchan (871G>A) is the most common deficiency variant in the Thai population.Hum Mutat. 2002;19:185.
Ganczakowski M, Bowden DK, Maitland K, et al. Thalassaemia in Vanuatu, south-west Pacific: frequency and haematological pheno-types o f young children.Br J Haematol. 1995;89:485–495.
Win N, Harano T, Harano K, et al. A wider molecular spectrum of beta-thalassaemia in Myanmar.Br J Haematol. 2002;117:988–992.
Pagano L, Lacerra G, Camardella L, et al. Hemoglobin Neapolis, beta 126(H4)Val—Gly: a novel beta-chain variant associated with a mild beta-thalassemia phenotype and displaying anomalous stability features.Blood. 1991;78:3070–3075.
Huisman THJ, Carver MFH, Baysal E.A Syllabus of Thalassaemia Mutations Augusta, Ga: The Sickle Cell Anaemia Foundation; 1997.
de Silva S, Fisher CA, Premawardhena A, et al. Thalassaemia in Sri Lanka: implications for the future health burden of Asian populations. Sri Lanka Thalassaemia Study Group.Lancet. 2000;355:786–791.
Kimura EM, Grignoli CR, Pinheiro VR, Costa FF, Sonati MF. Thalassemia intermedia as a result of heterozygosis for β0-thalassemia and αααanti-3.7/αα genotype in a Brazilian patient.Braz J Med Biol Res. 2003;36:699–701.
De Angioletti M, Lacerra G, Sabato V, Carestia C. Beta+45 G → C: a novel silent beta-thalassaemia mutation, the first in the Kozak sequence.Br J Haematol. 2004;124:224–231.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Than, A.M., Harano, T., Harano, K. et al. High Incidence of α-Thalassemia, Hemoglobin E, and Glucose-6-Phosphate Dehydrogenase Deficiency in Populations of Malaria-Endemic Southern Shan State, Myanmar. Int J Hematol 82, 119–123 (2005). https://doi.org/10.1532/IJH97.05028
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1532/IJH97.05028