Abstract
Background
Burden of Alzheimer’s disease (AD) and other dementias have grown rapidly over the decades, and high fasting plasma glucose (HFPG) was one of the well-established risk factors. It is urgently needed to estimate the global burden of AD and other dementias attributable to high fasting plasma glucose between regions, countries, age groups, and sexes to inform development of effective primary disease prevention strategies and intervention policies.
Methods
The burden of AD and other dementias attributable to HFPG was estimated based on a modeling strategy using the Global Burden of Disease Study 2019 dataset. The disease burden and time trend globally and by region, country, development level, age group, and sex were evaluated.
Results
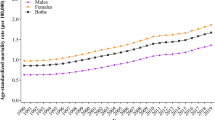
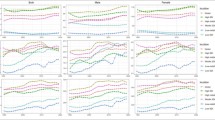
The number of AD and other dementias-related deaths attributable to HFPG increased from 42,998.23 (95% uncertainty interval, UI: 4459.86–163,455.78, the year of 1990) to 159,244.53 deaths (95% UI 18,385.23–583,514.15, the year of 2019). The age-standardized death rate increased from 1.69 (95% UI 0.18–6.54) in 1990 to 2.24 (95% UI 0.26–8.24) in 2019. The burden was higher in more developed regions. The burden in women was double that in men, that HFPG-attributable AD and other dementias caused 99,812.79 deaths (95% UI 9005.67–387,160.60) in women and 59,431.74 deaths (95% UI 5439.02–214,819.23) in men, with age-standardized death rate of 2.27 (95% UI 0.20–8.79) per 100,000 population in women and 2.20 (95% UI 0.20–8.00) in men.
Conclusion
Findings from the current study emphasizes the urgent requirement for targeted interventions in high-development regions, as well as the importance of proactive measures in middle-development countries in protection of AD and other dementias. The gender disparity necessitates the integration of gender-specific considerations in targeted approaches in prevention of AD and other dementias.



Similar content being viewed by others
Availability of data and materials: The datasets generated and/or analyzed during the current study are available in the Global Health Data Exchange (http://ghdx.healthdata.org).
Abbreviations
- AD:
-
Alzheimer’s disease
- DALYs:
-
Disability-adjusted Life Years
- FPG:
-
Fasting plasma glucose
- GBD:
-
Global Burden of Disease
- HFPG:
-
High Fasting Plasma Glucose
- SDI:
-
Sociodemographic Index
- UI:
-
Uncertainty Interval
- YLD:
-
year living with disability
- YLL:
-
year of life lost
References
Sims-Robinson C, Kim B, Rosko A, Feldman EL. How does diabetes accelerate Alzheimer disease pathology? Nature Reviews Neurology. 2010;6(10):551–9.
Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364(9):829–41.
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Kahn SE. Glucose control in type 2 diabetes: still worthwhile and worth pursuing. Jama. 2009;301(15):1590–2.
Liang R, Feng X, Shi D, Yang M, Yu L, Liu W, et al. The global burden of disease attributable to high fasting plasma glucose in 204 countries and territories, 1990–2019: An updated analysis for the Global Burden of Disease Study 2019. Diabetes/Metabolism Research and Reviews. 2022;38(8):e3572.
Li X, Feng X, Sun X, Hou N, Han F, Liu Y. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2019. Frontiers in Aging Neuroscience. 2022;14:937486.
GBD Collaborators, Nichols E, Abd-Allah F, Abdoli A, Abosetugn AE, Abrha WA, et al. Global mortality from dementia: Application of a new method and results from the Global Burden of Disease Study 2019. Alzheimer’s & Dementia: Translational Research & Clinical Interventions. 2021;7(1):e12200.
Crane PK, Walker R, Hubbard RA, Li G, Nathan DM, Zheng H, et al. Glucose Levels and Risk of Dementia. New England Journal of Medicine. 2013;369(6):540–8.
Rom S, Heldt NA, Gajghate S, Seliga A, Reichenbach NL, Persidsky Y. Hyperglycemia and advanced glycation end products disrupt BBB and promote occludin and claudin-5 protein secretion on extracellular microvesicles. Scientific reports. 2020;10(1):7274.
Russell JW, Sullivan KA, Windebank AJ, Herrmann DN, Feldman EL. Neurons undergo apoptosis in animal and cell culture models of diabetes. Neurobiol Dis. 1999;6(5):347–63.
Mohanty P, Hamouda W, Garg R, Aljada A, Ghanim H, Dandona P. Glucose challenge stimulates reactive oxygen species (ROS) generation by leucocytes. J Clin Endocrinol Metab. 2000;85(8):2970–3.
Sena CM, Pereira AM, Seiça R. Endothelial dysfunction - a major mediator of diabetic vascular disease. Biochim Biophys Acta. 2013;1832(12):2216–31.
Drake C, Boutin H, Jones MS, Denes A, McColl BW, Selvarajah JR, et al. Brain inflammation is induced by co-morbidities and risk factors for stroke. Brain Behav Immun. 2011;25(6):1113–22.
Wanrooy BJ, Kumar KP, Wen SW, Qin CX, Ritchie RH, Wong CHY. Distinct contributions of hyperglycemia and high-fat feeding in metabolic syndrome-induced neuroinflammation. J Neuroinflammation. 2018;15(1):293.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49.
Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS One. 2013;8(7):e65174.
Cahill S. WHO’s global action plan on the public health response to dementia: some challenges and opportunities. Aging & Mental Health. 2020;24(2):197–9.
2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 2020.
Jagust W. Imaging the evolution and pathophysiology of Alzheimer disease. Nature Reviews Neuroscience. 2018;19(11):687–700.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Cause List Mapped to ICD Codes [Available from: http://ghdx.healthdata.org/record/ihme-data/gbd-2019-cause-icd-code-mappings.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Global Burden of Disease Collaborative Network. Global burden of disease study 2019 (GBD 2019) socio-demographic index (SDI) 1950–2019. Global Burden of Disease Seattle; 2020.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–30.
Jao HF, Wung CH, Yu HC, Lee MY, Chen PC, Chen SC, et al. Sex Difference in the Associations among Obesity-Related Indices with Metabolic Syndrome in Patients with Type 2 Diabetes Mellitus. Int J Med Sci. 2021;18(15):3470–7.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes research and clinical practice. 2010;87(1):4–14.
Li Y, He Y, Qi L, Jaddoe VW, Feskens EJ, Yang X, et al. Exposure to the Chinese famine in early life and the risk of hyperglycemia and type 2 diabetes in adulthood. Diabetes. 2010;59(10):2400–6.
Zabuga O, Vaiserman A. Malnutrition in early life and risk of type 2 diabetes: Theoretical framework and epidemiological evidence. Moscow University Biological Sciences Bulletin. 2017;72:37–46.
van Abeelen AF, Elias SG, Bossuyt PM, Grobbee DE, van der Schouw YT, Roseboom TJ, et al. Famine exposure in the young and the risk of type 2 diabetes in adulthood. Diabetes. 2012;61(9):2255–60.
Halpern A, Mancini MC, Magalhães MEC, Fisberg M, Radominski R, Bertolami MC, et al. Metabolic syndrome, dyslipidemia, hypertension and type 2 diabetes in youth: from diagnosis to treatment. Diabetology & metabolic syndrome. 2010;2(1):1–20.
An J, Li H, Tang Z, Zheng D, Guo J, Liu Y, et al. Cognitive impairment and risk of all-cause and cardiovascular disease mortality over 20-year follow-up: Results from the BLSA. Journal of the American Heart Association. 2018;7(15):e008252.
Taylor CA, Greenlund SF, McGuire LC, Lu H, Croft JB. Deaths from alzheimer’s disease—United States, 1999–2014. Morbidity and mortality weekly report. 2017;66(20):521.
Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. The Lancet Public Health. 2022;7(2):e105–e25.
Sohn D, Shpanskaya K, Lucas JE, Petrella JR, Saykin AJ, Tanzi RE, et al. Sex Differences in Cognitive Decline in Subjects with High Likelihood of Mild Cognitive Impairment due to Alzheimer’s disease. Scientific reports. 2018;8(1):7490.
Pike CJ. Sex and the development of Alzheimer’s disease. J Neurosci Res. 2017;95(1–2):671–80.
C Carroll J, R Rosario E. The potential use of hormone-based therapeutics for the treatment of Alzheimer’s disease. Current Alzheimer Research. 2012;9(1):18–34.
Xu W, Tan L, Wang HF, Tan MS, Tan L, Li JQ, et al. Education and Risk of Dementia: Dose-Response Meta-Analysis of Prospective Cohort Studies. Mol Neurobiol. 2016;53(5):3113–23.
Fratiglioni L, Wang H-X. Brain reserve hypothesis in dementia. Journal of Alzheimer’s disease. 2007;12(1):11–22.
Perani D, Farsad M, Ballarini T, Lubian F, Malpetti M, Fracchetti A, et al. The impact of bilingualism on brain reserve and metabolic connectivity in Alzheimer’s dementia. Proceedings of the National Academy of Sciences. 2017;114(7):1690–5.
Valenzuela MJ. Brain reserve and the prevention of dementia. Current opinion in psychiatry. 2008;21(3):296–302.
Carter CL, Resnick EM, Mallampalli M, Kalbarczyk A. Sex and gender differences in Alzheimer’s disease: recommendations for future research. Journal of women’s health. 2012;21(10):1018–23.
Wu Y-T, Fratiglioni L, Matthews FE, Lobo A, Breteler MM, Skoog I, et al. Dementia in western Europe: epidemiological evidence and implications for policy making. The Lancet Neurology. 2016;15(1):116–24.
Acknowledgements
Not applicable.
Funding
Funding: This study was funded by the China Postdoctoral Science Foundation (2023M730112) and Bill and Melinda Gates Foundation (No. INV-0045085). The study sponsor had no role in the study design, data analysis and interpretation of data, the writing of the manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
Authors’ contributions: All authors helped develop the study concept and design. MW and KH contributed to the data collection, statistical analysis and manuscript writing. YJ and ZZ provided overall guidance and critical revision. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate: Not applicable.
Competing interests: The authors declare that they have no competing interests.
Additional information
How to cite this article: M. Wang, K. Huang, Y. Jin, et al. Global Burden of Alzheimer’s Disease and Other Dementias Attributed to High Fasting Plasma Glucose from 1990 to 2019. J Prev Alz Dis 2024; https://doi.org/10.14283/jpad.2024.47
Consent for publication: Not applicable.
Rights and permissions
About this article
Cite this article
Wang, M., Huang, K., Jin, Y. et al. Global Burden of Alzheimer’s Disease and Other Dementias Attributed to High Fasting Plasma Glucose from 1990 to 2019. J Prev Alzheimers Dis 11, 780–786 (2024). https://doi.org/10.14283/jpad.2024.47
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jpad.2024.47