Abstract
Background
Using residual values calculated from models regressing appendicular lean mass on fat mass and height is one of several suggested strategies for adjusting appendicular lean mass for body size when measuring sarcopenia. However, special consideration is required when using this technique in different subgroups in order to capture the correct individuals as sarcopenic.
Objectives
To provide guidance about how to conduct stratified analyses for the regression adjustment technique using age groups as an example.
Design
Cross-sectional study.
Setting
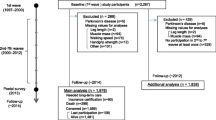
Data collected at baseline (2012–2015) for the Canadian Longitudinal Study on Aging.
Participants
Community dwelling participants of European descent aged 45 to 85 years (n=25,399).
Measurements
Appendicular lean mass, height, and weight were measured. Sex-specific residuals were calculated in participants before and after stratifying participants by age group (45–54, 55–64, 65–74, 75–85 years). Cut offs corresponding to the sex-specific 20th percentile residual values in participants ≥65 years were determined first in the residuals calculated in all participants and residuals calculated in only those aged ≥65 years. For each set of cut offs, the percentage of age and sex-stratified participants with low appendicular lean mass were compared for the residuals calculated in all participants and the residuals calculated after stratifying by age.
Results
In 12,622 males and 12,737 females, regardless of the cut off used, the percentage of participants with low appendicular lean mass decreased with age when residuals were calculated after age stratification. When the residuals were calculated in all participants, the percentage of participants with sarcopenia increased from the youngest to the oldest age groups.
Conclusions
Sex-specific residuals in all participants should be calculated prior to stratifying the sample by age group, or other stratification variables, for the purposes of developing appendicular lean mass cut offs or subgroup analyses.

Similar content being viewed by others
References
Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr 1997;127:990S–911S
Kim JH, Lim S, Choi SH, et al. Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. J Gerontol A Biol Sci Med Sci 2014;69:1244–1252
Landi F, Cruz-Jentoft AJ, Liperoti R, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing 2013;42:203–209
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairement and physical disability. J Am Geriatr Soc 2002;50:889–896
Yeung SSY, Reijnierse EM, Pham VK, et al. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 2019;10:485–500
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019;48:16–31
Cruz-Jentoft A, Baeyens J, Bauer J, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010;39:412–423
Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. Journals Gerontol Med Sci 2014;69:547–558
Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: An undiagnosed condition in older adults. Current consensus definition: Prevalence, etiology, and conseuqences. International Work Group on Sarcopenia. Am Med Dir Assoc 2011; 12:249–256
Chen L-K, Liu L-K, Woo J, et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 2014; 15:95–101
Gallagher D, Visser M, De Meersman RE, et al. Appendicular skeletal muscle mass: effects of age, gender, and ethnicity. J Appl Physiol 2017;83:229–239
Cawthon PM, Blackwell TL, Francisco S, et al. An evaluation of the usefulness of consensus definitions of sarcopenia in older men: results from the observational Osteoporotic Fractures in Men (MrOS) cohort study. J Am Diet Assoc 2016;63:2247–2259
Menant JC, Weber F, Lo J, et al. Strength measures are better than muscle mass measures in predicting health-related outcomes in older people: time to abandon the term sarcopenia? Osteoporos Int 2016; 1–12
Delmonico MJ, Harris TB, Lee J-S, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 2007;55:769–774
Newman AB, Kupelian V, Visser M, et al. Sarcopenia: Alternative Definitions and Associations with Lower Extremity Function. J Am Geriatr Soc 2003;51:1602–1609
Figueiredo CP, Domiciano DS, Lopes JB, et al. Prevalence of sarcopenia and associated risk factors by two diagnostic criteria in community-dwelling older men: The São Paulo Ageing & Health Study (SPAH). Osteoporos Int 2014;25:589–596
Domiciano DS, Figueiredo CP, Lopes JB, et al. Discriminating sarcopenia in community-dwelling older women with high frequency of overweight/obesity: The São Paulo Ageing & Health Study (SPAH). Osteoporos Int 2013;24:595–603
Chalhoub D, Cawthon PM, Ensrud KE, et al. Risk of nonspine fractures in older adults with sarcopenia, low bone mass, or both. J Am Geriatr Soc 2015;63:1733–1740
Scott D, Chandrasekara SD, Lasiert LL, Cicuttini F, Ebeling PR, Jones G. Associations of sarcopenic obesity and dynapenic obesity with bone mineral density and incident fractures over 5–10 years in community-dwelling older adults. Calcif Tissue Int 2016;99:30–42
Raina PS, Wolfson C, Kirkland SA, et al. Cohort profile: The Canadian Longitudinal Study on Aging (CLSA). Can J Aging 2009;28:221–229
Capistrant BD, Glymour MM, Berkman LF. Assessing mobility difficulties for cross-national comparisons: Results from the World Health Organiation Study on Global AGEing and Adult Health. J Am Geriatr Soc 2015;62:329–335
Leong DP, Teo KK, Rangarajan S, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015;386:266–273
Silva AM, Shen W, Heo M, et al. Ethnicity-related skeletal muscle differences across the lifespan. Am J Hum Biol 2010;22:76–82
Buckinx F, Landi F, Cesari M, et al. Pitfalls in the measurement of muscle mass: a need for a reference standard. J Cachexia Sarcopenia Muscle 2018;9:269–278
Kullberg J, Brandberg J, Angelhed JE, et al. Whole-body adipose tissue analysis: Comparison of MRI, CT and dual energy X-ray absorptiometry. Br J Radiol 2009;82:123–130
Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Stat Med 2000; 19:1141–1164
Falaschetti E, Laiho J, Primatesta P, Purdon S. Prediction equations for normal and low lung function from the health survey for England. Eur Respir J 2004;23:456–463
Beaudart C, Zaaria M, Reginster J. Health outcomes of sarcopenia: A systematic review and meta-analysis. PLoS One 2017;12:e0169548
Schaap LA, Schoor NM Van, Lips P, Visser M. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: The Longitudinal Aging Study Amsterdam. Journals Gerontol Med Sci 2018;73:1199–1204
Bischoff-Ferrari HA, Orav JE, Kanis JA, et al. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos Sarcopenia 2015;26:2793–2802
Acknowledgements
This research was made possible using the data/biospecimens collected by the Canadian Longitudinal Study on Aging (CLSA). Funding for the Canadian Longitudinal Study on Aging (CLSA) is provided by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference: LSA 94473 and the Canada Foundation for Innovation. This research has been conducted using the CLSA dataset, Baseline Comprehensive Dataset version 4.0, under Application Number 160608. The CLSA is led by Drs. Parminder Raina, Christina Wolf son and Susan Kirkland. The opinions expressed in this manuscript are the author’s own and do not reflect the views of the Canadian Longitudinal Study on Aging.
Funding
No funding to report.
Author information
Authors and Affiliations
Contributions
AJM, SMP, and PR conceptualized this project with feedback from NS, LT, PDM, RJd and GP. AJM and NS completed the analysis of the data. AJM, NS, and PR interpreted the results. AJM completed the draft of the manuscript with revisions from the remaining authors. All authors provided approval for the final version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval for this project was received by the Hamilton Research Ethics Board (#2686).
Additional information
Conflict of interest
None declared
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Mayhew, A.J., Phillips, S.M., Sohel, N. et al. Methodological Issues and the Impact of Age Stratification on the Proportion of Participants with Low Appendicular Lean Mass When Adjusting for Height and Fat Mass Using Linear Regression: Results from the Canadian Longitudinal Study on Aging. J Frailty Aging 10, 150–155 (2021). https://doi.org/10.14283/jfa.2020.48
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2020.48