Abstract
Introduction: Control of blood pressure can be a problem for intracranial procedures. To investigate the relationship between hemodynamic variables and endogenous vasoactive substances, we studied patients undergoing resection of arteriovenous malformations (AVMs).
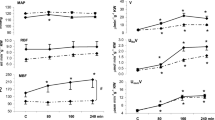
Methods: This was a nonrandomized, prospective study of six patients who had resection of an intracranial AVM and six patients who had clipping of an intracranial aneurysm (ICA) that had not bled. Operative and postoperative blood pressure was controlled with sodium nitroprusside. Heart rate (HR), mean arterial pressure, pulmonary capillary wedge pressure, and cardiac index (CI) were measured after induction of anesthesia; before, during, and after hypotensive anesthesia; immediately postoperatively; and at 12, 24, and 36 hours postoperatively. Blood samples were drawn simultaneously in the AVM group to measure levels of norepinephrine, epinephrine, renin, aldosterone, vasopressin, angiotensin I, and angiotensin II and correlated with significant hemodynamic changes.
Results: HR and CI increased significantly among patients with AVMs compared with patients with ICAs (p<0.001 and p=0.05, respectively). HR was significantly correlated with renin (r=0.60), norepinephrine (r=1.00), and vasopressin (r=0.66). CI was significantly correlated with epinephrine (r=1.00), renin (r=0.77), angiotensin II (r=0.71), and vasopressin (r=0.82). Patients with AVMs had a hyperdynamic state characterized by increases in HR and CI. These increases were accompanied by increased renin, norepinephrine, vasopressin, epinephrine, and angiotensin II serum concentrates.
Conclusions: There were no significant differences in blood pressure changes between patients who had resection for AVM and those who had clipping of ICA, probably due to the use of sodium nitroprusside in the AVM group. Patients with AVMs had a hyperdynamic state with increases in epinephrine, norepinephrine, angiotensin II, plasma renin activity, and vasopressin. Whether this hyperdynamic state is caused by the resection of the AVM or the use of sodium nitroprusside (SNP) cannot be concluded. Blockage of these mediators preoperatively may help control blood pressure without sodium nitroprusside.
Similar content being viewed by others
References
Basali A, Mascha EJ, Kalfas I, Schubert A. Relation between perioperative hypertension and intracranial hemorrhage after craniotomy. Anesthesiology 2000;93:48–54.
Muzzi DA, Black S, Losasso TJ, Cucchiara RF. Labetalol and esmolol in the control of hypertension after intracranial surgery. Anesth Analg 1990;70:68–71.
Orlowski JP, Shiesley D, Vidt DG, Barnett GH, Little JR. Labetalol to control blood pressure after cerebrovascular surgery. Crit Care Med 1988;16:765–68.
Kalfas IH, Little JR. Postoperative hemorrhage: a survey of 4,992 intracranial procedures. Neurosurgery 1988;23:343–347.
Szabo MD, Crosby G, Sundaram P, Dodson BA, Kjellberg RN. Hypertension does not cause spontaneous hemorrhage of intracranial arteriovenous malformations. Anesthesiology 1989;70:761–763.
Bloomfield EL, Schubert A, Secic M, Barnett G, Shutway F, Ebrahim ZY. The influence of scalp infiltration with bupivacaine on hemodynamics and postoperative pain in adult patients undergoing craniotomy. Anesth Analg 1998;87:579–582.
Bloomfield EL, Porembka DT, Ebrahim ZY, et al. Analysis of catecholamine and vasoactive peptide release in intracranial arterial venous malformations. J Neurosurg Anesthesiol 1996;8:101–110.
Suzuki H, Smeby RR, Mimaki H, et al. Nonrenal factors contribute to plasma and cerebrospinal fluid angiotensin II. Hypertension 1986;8 (Suppl 1):I95-I100.
Haber E, Koerner T, Page LB, Kliman B, Purnode A. Application of a radioimmunoassay for angiotensin I to the physiologic measurements of plasma renin activity in normal human subjects. J Clin Endocrinol Metab 1969;29:1349–1355.
Collins GB, Brosnihan KB, Zuti RA, Messina M, Gupta MK. Neuroendocrine, fluid balance, and thirst responses to alcohol in alcoholics. Alcohol Clin Exp Res 1992;16:228–233.
Shapiro HM. Intracranial hypertension: therapeutic and anesthetic considerations. Anesthesiology 1975;43:445–71.
Wilkins RH. Natural history of intracranial vascular malformations: a review. Neurosurgery 1985;16:421–430.
Hillman DR, Rung GW, Thompson WR, Davis NJ. The effect of bupivacaine scalp infiltration on the hemodynamic response to craniotomy under general anesthesia. Anesthesiology 1987;67:1001–1003.
Tinker JH, Michenfelder JD. Sodium nitroprusside: pharmacology, toxicology and therapeutics. Anesthesiology 1976;45:340–354.
Rawlinson WA, Loach AB, Benedict CR. Changes in plasma concentration of adrenaline and noradrenaline in anaesthetized patients during sodium nitroprusside-induced hypotension. Br J Anaesth 1978;50:937–943.
Khambatta HJ, Stone JG, Khan E. Hypertension during anesthesia on discontinuation of sodium nitroprusside-induced hypotension. Anesthesiology 1979;51:127–130.
Cameron SJ, Doig A. Cerebellar tumours presenting with clinical features of phaeochromocytoma. Lancet 1970;1:492–494.
Evans CH, Westfall V, Atuk NO. Astrocytoma mimicking the features of pheochromocytoma. N Engl J Med 1972;286:1397–1399.
Gabriel R, Harrison BD. Meningioma mimicking features of a phaeochromocytoma. Br Med J. 1974;2:312.
Meyer BC. Neoplasm of posterior fossa stimulating cerebral vascular disease: report of 5 cases with reference to the role of medulla in production of arterial hypertension. Arch Neurol Psychiatr 1941;45:468–80.
Emanuele MA, Dorsch TR, Scarff TB, Lawrence AM. Basilar artery aneurysm simulating pheochromocytoma. Neurology 1981;31:1560–1561.
Edvinsson L, Nielsen KC, Owman C, Sporrong B. Cholinergic mechanisms in pial vessels. Histochemistry, electron microscopy and pharmacology. Z Zellforsch Mikrosk Anat 1972;134:311–325.
Falck B, McHedlishvili GI, Owman C. Histochemical demonstration of adrenergic nerves in cortex-pia of rabbit. Acta Pharmacol Toxicol 1965;23:133–142.
Edvinsson L, Lindvall M, Nielsen KC, Owman C. Are brain vessels innervated also by central (non-sympathetic) adrenergic neurones? Brain Res 1973;63:496–499.
Uddman R, Edvinsson L, Owman C, Sundler F. Perivascular substance P: occurrence and distribution in mammalian pial vessels. J Cereb Blood Flow Metab 1981;1:227–232.
Uddman R, Edvinsson L, Hakanson R, Owman C, Sundler F. Immunohistochemical demonstration of APP (avian pancreatic polypeptide)-immunoreactive nerve fibres around cerebral blood vessels. Brain Res Bull 1982;9:715–718.
Uddman R, Edvinsson L, Owman C, Sundler F. Nerve fibres containing gastrin-releasing peptide around pial vessels. J Cereb Blood Flow Metab 1983;3:386–390.
Ferrario CM, Averill DB. Do primary dysfunctions in neural control of arterial pressure contribute to hypertension? Hypertension 1991;18:138–151.
Jannetta PJ, Gendell HM. Clinical observations on etiology of essential hypertension. Surg Forum 1979;30:431–432.
Scott BB, McGillicuddy JE, Seeger JF, Kindt GW, Giannotta SL. Vascular dynamics of an experimental cerebral arteriovenous shunt in the primate. Surg Neurol 1978;10:34–38.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bloomfield, E.L., Secic, M. & Porembka, D. A correlation of catecholamine and vasoactive peptide release with hemodynamics in patients undergoing resection of arteriovenous malformations. Neurocrit Care 3, 127–131 (2005). https://doi.org/10.1385/NCC:3:2:127
Issue Date:
DOI: https://doi.org/10.1385/NCC:3:2:127