Summary
Introduction: Benign tumors of the liver are increasingly being diagnosed and continue to represent a management challenge. These lesions constitute a substantial component of hepatic neoplasms evaluated and resected at a tertiary referral center. We reviewed our experience with resection of benign liver lesions to clarify the safety and effectiveness of this treatment.
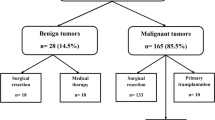
Methods: Between January 1996 and January 2000, 28 patients with benign hepatic lesions were identified from a cohort of 140 hepatic resection patients. Demographic characteristics, operative management, morbidity, mortality and follow-up were retrospectively analyzed.
Results: The mean age in our patients was 35±14, with 24/28 (86%) patients being female. Seven of the 24 woman (29%) at presentation were either pregnant or immediate postpartum. A history of OCP use was noted in 14/24 (58%) female patients. The most common presenting symptom was abdominal pain in 12/28 (43%). Resection for an undiagnosed mass occurred in 11/28 (39%) patients. The distribution of pathology was hemangioma 10/28 (35.7%), adenoma 8/28 (28.6%), hepatic cyst 5/28 (17.9%), hamartoma 2/28 (7.1%), and FNH 3/28 (10.7%). Average size of the tumor was 7.4±3.9 (range 2.5–15 cm) with a mean of 1.4±0.8 lesions (range 1–3) per patient. Tumors were evenly distributed between the right and left side while eight patients (29%) had bilobar tumors. Enucleation rather than anatomic resection was performed in 18/28 (64%) patients, with a mean blood loss of 457±532 cc (range 50–2200 cc). Blood transfusion was required in only 3/28 (10%) patients, while total vascular isolation was used in only a single patient undergoing an extended left hepatectomy. Mean length of stay was 6.8±3.2 d (range 3–14 d). Three complications (10.7%) were encountered: pulmonary embolus, ileus and non-operative bile leak. There were no mortalities in this series. Recurrence of tumor occurred in only one patient with a giant hepatic cyst managed laparoscopically.
Conclusions: In our institution, the management of clinically relevant benign tumors of the liver comprises a significant proportion of our resectional practice (20%). Our data suggests that both enucleation and anatomically based resections can be performed safely with minimal blood loss and transfusion requirements. Resection of symptomatic lesions was highly effective in treating abdominal pain due to these benign tumors. We advocate resection of non-resolving hepatic adenomas, symptomatic lesions, or when malignancy cannot be excluded.
Similar content being viewed by others
References
Nichols FC 3rd, van Heerden JA, Weiland LH. Benign liver tumors. Surg Clin North Am. 1989;69(2):297–314.
Nagorney DM. Benign hepatic tumors: focal nodular hyperplasia and hepatocellular adenoma. World J Surg 1995;19(1):13–18.
Pain JA, Gimson AE, Williams R, Howard ER. Focal nodular hyperplasia of the liver: results of treatment and options in management. Gut 1991;32(5):524–527.
Leese T, Farges O, Bismuth H. Liver cell adenomas. A 12-year surgical experience from a specialist hepatobiliary unit. Ann Surg 1988;208(5):558–564.
Iwatsuki S, Todo S, Starzl TE. Excisional therapy for benign hepatic lesions. Surg Gynecol Obstet 1990;171(3):240–246.
Belghiti J, Pateron D, Panis Y, et al. Resection of presumed benign liver tumours. Br J Surg 1993;80(3):380–383.
Brady MS, Coit DG. Focal nodular hyperplasia of the liver. Surg Gynecol Obstet 1990;171(5):377–381.
Farges O, Daradkeh S, Bismuth H. Cavernous hemangiomas of the liver: are there any indications for resection? World J Surg 1995;19(1):19–24.
Kerlin P, Davis GL, McGill DB, Weiland LH, Adson MA, Sheedy PF 2nd. Hepatic adenoma and focal nodular hyperplasia: clinical, pathologic, and radiologic features. Gastroenterology 1983;84(5 Pt 1):994–1002.
Herman P, Pugliese V, Machado MA, et al. Hepatic adenoma and focal nodular hyperplasia: differential diagnosis and treatment. World J Surg 2000;24(3):372–376.
Shortell CK, Schwartz SI. Hepatic adenoma and focal nodular hyperplasia. Surg Gynecol Obstet 1991;173(5):426–431.
Klatskin G. Hepatic tumors: possible relationship to use of oral contraceptives. Gastroenterology 1977;73(2):386–394.
Gyorffy EJ, Bredfeldt JE, Black WC. Transformation of hepatic cell adenoma to hepatocellular carcinoma due to oral contraceptive use. Ann Intern Med 1989;110(6):489–490.
Neuberger J, Portmann B, Nunnerley HB, Laws JW, Davis M, Williams R. Oral-contraceptive-associated liver tumours: occurrence of malignancy and difficulties in diagnosis. Lancet 1980;1(8163):273–276.
Gordon SC, Reddy KR, Livingstone AS, Jeffers LJ, Schiff ER. Resolution of a contraceptive-steroid-induced hepatic adenoma with subsequent evolution into hepatocellular carcinoma. Ann Intern Med 1986;105(4):547–549.
Katkhouda N, Mavor E, Gugenheim J, Mouiel J. Laparoscopic management of benign cystic lesions of the liver. J Hepatobiliary Pancreat Surg 2000;7(2):212–217.
Katkhouda N, Hurwitz M, Gugenheim J, et al. Laparoscopic management of benign solid and cystic lesions of the liver. Ann Surg 1999;229(4):460–466.
Kelly D, Emre S, Guy SR, Sheiner PA, Miller CM, Schwartz ME. Resection of benign hepatic lesions with selective use of total vascular isolation. J Am Coll Surg 1996;183(2):113–116.
Emre S, Schwartz ME, Katz E, Miller CM. Liver resection under total vascular isolation. Variations on a theme. Ann Surg 1993;217(1):15–19.
Heaney JP, Stanton WK, Halbert DS, Seidel J, Vice T. An improved technic for vascular isolation of the liver: experimental study and case reports. Ann Surg 1966;163(2):237–241.
Bismuth H, Castaing D, Garden OJ. Major hepatic resection under total vascular exclusion. Ann Surg 1989;210(1):13–19.
Huguet C, Addario-Chieco P, Gavelli A, Arrigo E, Harb J, Clement RR. Technique of hepatic vascular exclusion for extensive liver resection. Am J Surg 1992;163(6):602–605.
Torzilli G, Makuuchi M, Midorikawa Y, et al. Liver resection without total vascular exclusion: hazardous or beneficial? An analysis of our experience. Ann Surg 2001;233(2):167–175.
Belghiti J, Noun R, Zante E, Ballet T, Sauvanet A. Portal triad clamping or hepatic vascular exclusion for major liver resection. A controlled study. Ann Surg 1996;224(2):155–161.
Grazi GL, Mazziotti A, Jovine E, et al. Total vascular exclusion of the liver during hepatic surgery. Selective use, extensive use, or abuse? Arch Surg 1997;132(10):1104–1109.
Berney T, Mentha G, Morel P. Total vascular exclusion of the liver for the resection of lesions in contact with the vena cava or the hepatic veins. Br J Surg 1998;85(4):485–488.
Habib NA, Koh MK, Zografos G, Awad RW, Bottino G. Elective hepatic resection for benign and malignant liver disease: early results. Br J Surg 1993;80(8):1039–1041.
Emond JC, Renz JF. Surgical anatomy of the liver and its application to hepatobiliary surgery and transplantation. Semin Liver Dis 1994;14(2):158–168.
Sitzmann JV, Greene PS. Perioperative predictors of morbidity following hepatic resection for neoplasm. A multivariate analysis of a single surgeon experience with 105 patients. Ann Surg 1994;219(1):13–17.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kammula, U.S., Buell, J.F., Labow, D.M. et al. Surgical management of benign tumors of the liver. Int J Gastrointest Canc 30, 141–146 (2001). https://doi.org/10.1385/IJGC:30:3:141
Issue Date:
DOI: https://doi.org/10.1385/IJGC:30:3:141