Abstract
Introduction
Food insecurity (FI) may predispose individuals to suboptimal nutrition, leading to chronic disease and poor health outcomes. We sought to assess the impact of county-level FI on postoperative outcomes among patients undergoing resection of hepatopancreaticobiliary (HPB) cancer.
Methods
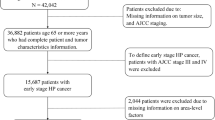
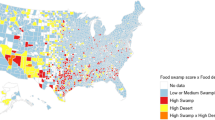
Patients who were diagnosed with HPB cancer between 2010 and 2015 were identified from the Surveillance, Epidemiology, and End Results (SEER)-Medicare database. Data on annual county-level FI were obtained from the Feeding America: Mapping the Meal Gap report and were categorized into tertiles. Textbook outcome was defined as no extended length of stay, perioperative complications, 90-day readmission, and 90-day mortality. Multiple logistic regression and Cox regression models were used to assess outcomes and survival relative to FI.
Results
Among 49,882 patients (hepatocellular: n = 11,937, 23.9%; intrahepatic cholangiocarcinoma: n = 2111, 4.2%; extrahepatic cholangiocarcinoma: n = 4047, 8.1%; gallbladder: n = 2853, 5.7%; pancreatic: n = 28,934, 58.0%), 6702 (13.4%) patients underwent a surgical resection. Median age was 75 years (interquartile range 69–82), and most patients were male (n = 25,767, 51.7%) and self-identified as White (n = 36,381, 72.9%). Overall, 5291 (10.6%) and 39,664 (79.5%) individuals resided in low or moderate FI counties, respectively, while 4927 (9.8%) patients resided in high FI counties. Achievement of textbook outcome (TO) was 56.3% (n = 6702). After adjusting for competing risk factors, patients residing in high FI counties had lower odds to achieve a TO versus individuals living in low FI counties (odds ratio 0.69, 95% confidence interval [CI] 0.54–0.88, p = 0.003). In addition, patients residing in moderate and high FI counties had a greater risk of mortality at 1- (referent, low, moderate: hazard ratio [HR] 1.09, 95% CI 1.05–1.14; high: HR 1.14, 95% CI 1.08–1.21), 3- (referent, low, moderate: HR 1.09, 95% CI 1.05–1.14; high: HR 1.14, 95% CI 1.08–1.21), and 5- (referent, low, moderate: HR 1.05, 95% CI 1.01–1.09; high: HR 1.07, 95% CI 1.02–1.13) years versus individuals from low FI counties.
Conclusions
FI was associated with adverse perioperative outcomes and long-term survival following resection of an HPB malignancy. Interventions directed towards mitigating nutritional inequities are needed to improve outcomes among vulnerable HPB populations.



Similar content being viewed by others
References
Zhang H, Zhang W, Jiang L, Chen Y. Recent advances in systemic therapy for hepatocellular carcinoma. Biomark Res. 2022;10(1):3. https://doi.org/10.1186/s40364-021-00350-4.
Blechacz B. Cholangiocarcinoma: current knowledge and new developments. Gut Liver. 2017;11(1):13–26. https://doi.org/10.5009/gnl15568.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24(43):4846–61. https://doi.org/10.3748/wjg.v24.i43.4846.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Pericleous M, Khan SA. Epidemiology of HPB malignancy in the elderly. Eur J Surg Oncol. 2021;47(3, Part A):503–13. https://doi.org/10.1016/j.ejso.2020.03.222.
Flores YN, Datta GD, Yang L, et al. Disparities in hepatocellular carcinoma incidence, stage, and survival: a large population-based study. Cancer Epidemiol Biomark Prev. 2021;30(6):1193–9. https://doi.org/10.1158/1055-9965.EPI-20-1088.
Noel M, Fiscella K. Disparities in pancreatic cancer treatment and outcomes. Health Equity. 2019;3(1):532–40. https://doi.org/10.1089/heq.2019.0057.
Munir MM, Woldesenbet S, Endo Y, et al. Racial segregation among patients with cholangiocarcinoma: impact on diagnosis, treatment, and outcomes. Ann Surg Oncol. 2023. https://doi.org/10.1245/s10434-023-13122-1.
Munir MM, Woldesenbet S, Endo Y, et al. Disparities in socioeconomic factors mediate the impact of racial segregation among patients with hepatopancreaticobiliary cancer. Ann Surg Oncol. 2023. https://doi.org/10.1245/s10434-023-13449-9.
Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1. Accessed 6 Mar 2023.
Closing the gap in a generation: health equity through action on the social determinants of health—final report of the commission on social determinants of health. https://www.who.int/publications-detail-redirect/WHO-IER-CSDH-08.1. Accessed 17 Nov 2022.
CDC: attaining health equity—healthy communities program. Published 29 May 2019. https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/overview/healthequity.htm. Accessed 17 Nov 2022.
World Health Organization. Monitoring health inequality: an essential step for achieving health equity. World Health Organization; 2014. https://apps.who.int/iris/handle/10665/133849. Accessed 17 Nov 2022.
Coleman-Jensen A. Household Food Security in the United States in 2021. Published online 2021. https://www.ers.usda.gov/publications/pub-details/?pubid=104655. Accessed 6 Mar 2023.
USDA ERS: key statistics & graphics. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/key-statistics-graphics/. Accessed 6 Mar 2023.
Gundersen C, Seligman HK. Food insecurity and health outcomes. Econ Voice. 2017. https://doi.org/10.1515/ev-2017-0004.
Pan L, Sherry B, Njai R, Blanck HM. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet. 2012;112(9):1403–9. https://doi.org/10.1016/j.jand.2012.06.011.
Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–10. https://doi.org/10.3945/jn.109.112573.
The Economics of Food Insecurity in the United States: Gundersen—2011—Applied Economic Perspectives and Policy. Wiley Online Library. https://doi.org/10.1093/aepp/ppr022. Accessed 6 Mar 2023.
Donaldson MS. Nutrition and cancer: a review of the evidence for an anti-cancer diet. Nutr J. 2004;3(1):19. https://doi.org/10.1186/1475-2891-3-19.
Béliveau R, Gingras D. Role of nutrition in preventing cancer. Can Fam Physician. 2007;53(11):1905–11.
Patel KG, Borno HT, Seligman HK. Food insecurity screening: a missing piece in cancer management. Cancer. 2019;125(20):3494–501. https://doi.org/10.1002/cncr.32291.
Raber M, Jackson A, Basen-Engquist K, et al. Food insecurity among people with cancer: nutritional needs as an essential component of care. J Natl Cancer Inst. 2022;114(12):1577–83. https://doi.org/10.1093/jnci/djac135.
Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31–46. https://doi.org/10.3322/caac.21586.
Avgerinos KI, Spyrou N, Mantzoros CS, Dalamaga M. Obesity and cancer risk: emerging biological mechanisms and perspectives. Metabolism. 2019;92:121–35. https://doi.org/10.1016/j.metabol.2018.11.001.
Iadeluca L, Mardekian J, Chander P, Hopps M, Makinson GT. The burden of selected cancers in the US: health behaviors and health care resource utilization. Cancer Manag Res. 2017;9:721–30. https://doi.org/10.2147/CMAR.S143148.
Tabung FK, Brown LS, Fung TT. Dietary patterns and colorectal cancer risk: a review of 17 years of evidence (2000–2016). Curr Colorectal Cancer Rep. 2017;13(6):440–54. https://doi.org/10.1007/s11888-017-0390-5.
Map the Meal Gap Data | Feeding America. https://www.feedingamerica.org/research/map-the-meal-gap/how-we-got-the-map-data. Accessed 6 Mar 2023.
United States Census Bureau. American Community Survey (ACS). Census.gov. https://www.census.gov/programs-surveys/acs. Accessed 17 Dec 2022.
Merath K, Chen Q, Bagante F, et al. Textbook outcomes among medicare patients undergoing hepatopancreatic surgery. Ann Surg. 2020;271(6):1116–23. https://doi.org/10.1097/SLA.0000000000003105.
Azap RA, Paredes AZ, Diaz A, Hyer JM, Pawlik TM. The association of neighborhood social vulnerability with surgical textbook outcomes among patients undergoing hepatopancreatic surgery. Surgery. 2020;168(5):868–75. https://doi.org/10.1016/j.surg.2020.06.032.
Mehta R, Tsilimigras DI, Paredes AZ, et al. Comparing textbook outcomes among patients undergoing surgery for cancer at U.S. News & World Report ranked hospitals. J Surg Oncol. 2020;121(6):927–35. https://doi.org/10.1002/jso.25833.
Gany F, Lee T, Ramirez J, et al. Do our patients have enough to eat? Food insecurity among urban low-income cancer patients. J Health Care Poor Underserved. 2014;25(3):1153–68. https://doi.org/10.1353/hpu.2014.0145.
Gany F, Lee T, Ramirez J, et al. Are our severely ill patients hungry? JCO. 2011;29(15 Suppl):e19626. https://doi.org/10.1200/jco.2011.29.15_suppl.e19626.
Simmons LA, Modesitt SC, Brody AC, Leggin AB. Food insecurity among cancer patients in Kentucky: a pilot study. J Oncol Pract. 2006;2(6):274–9. https://doi.org/10.1200/JOP.2006.2.6.274.
Adler NE, Glymour MM, Fielding J. Addressing social determinants of health and health inequalities. JAMA. 2016;316(16):1641–2. https://doi.org/10.1001/jama.2016.14058.
Social Determinants of Health: Healthy People 2030 | health.gov. https://health.gov/healthypeople/priority-areas/social-determinants-health. Accessed 17 Nov 2022.
Food Accessibility, Insecurity and Health Outcomes. NIMHD. https://www.nimhd.nih.gov/resources/understanding-health-disparities/food-accessibility-insecurity-and-health-outcomes.html. Accessed 6 Mar 2023.
Wight V, Kaushal N, Waldfogel J, Garfinkel I. Understanding the link between poverty and food insecurity among children: does the definition of poverty matter? J Child Poverty. 2014;20(1):1–20. https://doi.org/10.1080/10796126.2014.891973.
Hunger in America Study | Feeding America. https://www.feedingamerica.org/research/hunger-in-america. Accessed 6 Mar 2023.
Zhang FF, Cudhea F, Shan Z, et al. Preventable cancer burden associated with poor diet in the United States. JNCI Cancer Spectr. 2019;3(2):pkz034. https://doi.org/10.1093/jncics/pkz034.
Sharkey JR, Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the ground-truthed food environment in a large rural area. J Nutr. 2008;138(3):620–7. https://doi.org/10.1093/jn/138.3.620.
Moore LV, Diez Roux AV, Franco M. Measuring availability of healthy foods: agreement between directly measured and self-reported data. Am J Epidemiol. 2012;175(10):1037–44. https://doi.org/10.1093/aje/kwr445.
Bardenhagen CJ, Pinard CA, Pirog R, Yaroch AL. Characterizing rural food access in remote areas. J Community Health. 2017;42(5):1008–19. https://doi.org/10.1007/s10900-017-0348-1.
Vilar-Compte M, Burrola-Méndez S, Lozano-Marrufo A, et al. Urban poverty and nutrition challenges associated with accessibility to a healthy diet: a global systematic literature review. Int J Equity Health. 2021;20(1):40. https://doi.org/10.1186/s12939-020-01330-0.
Pooler JA, Hartline-Grafton H, DeBor M, Sudore RL, Seligman HK. Food insecurity: a key social determinant of health for older adults. J Am Geriatr Soc. 2019;67(3):421–4. https://doi.org/10.1111/jgs.15736.
Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26-32. https://doi.org/10.1542/peds.2009-3146.
Gundersen C, Engelhard EE, Crumbaugh AS, Seligman HK. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. 2017;20(8):1367–71. https://doi.org/10.1017/S1368980017000180.
Marques ES, Reichenheim ME, de Moraes CL, Antunes MML, Salles-Costa R. Household food insecurity: a systematic review of the measuring instruments used in epidemiological studies. Public Health Nutr. 2015;18(5):877–92. https://doi.org/10.1017/S1368980014001050.
Banks AR, Bell BA, Ngendahimana D, Embaye M, Freedman DA, Chisolm DJ. Identification of factors related to food insecurity and the implications for social determinants of health screenings. BMC Public Health. 2021;21(1):1410. https://doi.org/10.1186/s12889-021-11465-6.
Lussiez A, Englesbe M, Howard R. Surgery and population health: closing the gap between margin and mission. Ann Surg. 2022;275(2):e286–7. https://doi.org/10.1097/SLA.0000000000005010.
Barrett S, Begg S, Sloane A, Kingsley M. Surgeons and preventive health: a mixed methods study of current practice, beliefs and attitudes influencing health promotion activities amongst public hospital surgeons. BMC Health Serv Res. 2019;19(1):358. https://doi.org/10.1186/s12913-019-4186-y.
Warner DO, Sarr MG, Offord KP, Dale LC. Anesthesiologists, general surgeons, and tobacco interventions in the perioperative period. Anesth Analg. 2004;99(6):1766–73. https://doi.org/10.1213/01.ANE.0000136773.40216.87.
Lussiez A, Hallway A, Lui M, et al. Evaluation of an intervention to address smoking and food insecurity at preoperative surgical clinic appointments. JAMA Netw Open. 2022;5(10):e2238677. https://doi.org/10.1001/jamanetworkopen.2022.38677.
Acknowledgment
None.
Funding
No sources of funding were used to assist in the preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Akpunonu Chinaemelum, Muhammad Musaab Munir, Lovette Azap, Selamawit Woldesenbet, Mary Dillhoff, Jordan Cloyd, Aslam Ejaz, and Timothy M. Pawlik have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chinaemelum, A., Munir, M.M., Azap, L. et al. Impact of Food Insecurity on Outcomes Following Resection of Hepatopancreaticobiliary Cancer. Ann Surg Oncol 30, 5365–5373 (2023). https://doi.org/10.1245/s10434-023-13723-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13723-w