Abstract
Purpose
The study aimed to identify the value and optimal age cutoff to predict the progression of highly suspicious thyroid nodules ≤ 10 mm during active surveillance (AS), and to reveal distinct risk factors in patients of different ages.
Methods
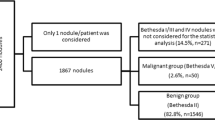
A total of 779 patients with highly suspicious thyroid nodules were enrolled and followed up by ultrasonography. Locally weighted scatterplot smoothing (LOWESS) and the package ‘changepoint’ were used to identify the optimal age cutoffs using R. Multivariate Cox regression was performed to identify independent prognostic factors in each patient group divided according to age.
Results
Age was an independent predictor of nodule progression (P = 0.038). The optimal age cutoff to stratify the risk of nodule progression was 30 years. Younger patients were more likely to have progression of nodules during AS (P < 0.001), including enlargement of nodule size (P = 0.011) and new lesion occurrence (P < 0.001). Nodule size was identified as a risk factor for disease progression in patients younger than 30 years old (P = 0.008, OR 7.946, 95% CI 1.715–36.820), while multifocality (P = 0.018, OR 2.315, 95% CI 1.155–4.639) and thyroiditis (P = 0.028, OR 2.265, 95% CI 1.092–4.699) were independent predictors in patients over 30 years old.
Conclusions
Highly suspicious thyroid nodules ≤ 10 mm in young patients tended to be more progressive. The predictors of disease progression were distinct in patients of different ages.



Similar content being viewed by others
References
Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006;295:2164–7.
Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014;140(4):317–22.
Park S, Oh CM, Cho H, et al. Association between screening and the thyroid cancer “epidemic” in South Korea: evidence from a nationwide study. BMJ. 2016;355:i5745.
Li M, Dal Maso L, Vaccarella S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 2020;8(6):468–70.
Brenner DR, Weir HK, Demers AA, et al. Projected estimates of cancer in Canada in 2020. CMAJ. 2020;192(9):E199–205.
Patel KN, Yip L, Lubitz CC, et al. The American Association of endocrine surgeons guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. 2020;271(3):e21-93.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133.
Sugitani I, Ito Y, Takeuchi D, et al. Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: consensus statements from the Japan Association of Endocrine Surgery Task Force on management for papillary thyroid microcarcinoma. Thyroid. 2021;31(2):183–92.
Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”—screening and overdiagnosis. N Engl J Med. 2014;371(19):1765–7.
Tuttle RM, Fagin JA, Minkowitz G, et al. Natural history and tumor volume kinetics of papillary thyroid cancers during active surveillance. JAMA Otolaryngol Head Neck Surg. 2017;143(10):1015–20.
Sakai T, Sugitani I, Ebina A, et al. Active surveillance for T1bN0M0 papillary thyroid carcinoma. Thyroid. 2019;29(1):59–63.
Fukuoka O, Sugitani I, Ebina A, et al. Natural history of asymptomatic papillary thyroid microcarcinoma: time-dependent changes in calcification and vascularity during active surveillance. World J Surg. 2016;40(3):529–37.
Ito Y, Miyauchi A, Inoue H, et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg. 2010;34(1):28–35.
Nagaoka R, Ebina A, Toda K, et al. Multifocality and progression of papillary thyroid microcarcinoma during active surveillance. World J Surg. 2021;45(9):2769–76.
Ito Y, Miyauchi A, Kihara M, et al. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014;24(1):27–34.
Liu C, Zhao H, Xia Y, et al. Active surveillance of highly suspicious thyroid nodules cohort in China shows a worse psychological status in younger patients. Front Oncol. 2022;12:981495.
Zanocco KA, Hershman JM, Leung AM. Active surveillance of low-risk thyroid cancer. JAMA. 2019;321(20):2020–1.
Oh HS, Ha J, Kim HI, et al. Active surveillance of low-risk papillary thyroid microcarcinoma: a multi-center cohort study in Korea. Thyroid. 2018;28(12):1587–94.
Sugitani I, Toda K, Yamada K, et al. Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J Surg. 2010;34(6):1222–31.
Vasileiadis I, Karakostas E, Charitoudis G, et al. Papillary thyroid microcarcinoma: clinicopathological characteristics and implications for treatment in 276 patients. Eur J Clin Investig. 2012;42(6):657–64.
Cappelli C, Castellano M, Braga M, et al. Aggressiveness and outcome of papillary thyroid carcinoma (PTC) versus microcarcinoma (PMC): a mono-institutional experience. J Surg Oncol. 2007;95(7):555–60.
Acknowledgment
This work was supported by a grant provided by the Capital Clinical Features Application Research (Z171100001017211).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhuge, L., Huang, Z., Cai, H. et al. The Optimal Age Threshold for Stratifying the Risks of Disease Progression in Patients with Highly Suspicious Sub-centimeter Thyroid Nodules. Ann Surg Oncol 30, 5463–5469 (2023). https://doi.org/10.1245/s10434-023-13497-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13497-1