Abstract
Background
Application of patient-reported outcomes (PROs) in surgical oncology has been limited because of patient heterogeneity. We analyzed symptom trajectories and their associations with recovery outcomes after lung cancer surgery, aiming to profile the heterogeneity of patients’ experiences and to identify patients needing extensive care.
Methods
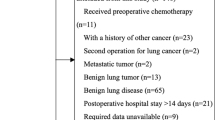
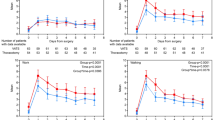
Symptoms were assessed with the MDASI-LC before surgery, daily after surgery in hospital and weekly within 1 month after discharge. Patients were clustered based on symptoms from post-operative day 1 (POD1) to POD5, using the latent-class-trajectory-model. Functional recovery was compared across the trajectories. Logistic regression was used to explore risk factors for trajectories of more severe symptoms.
Results
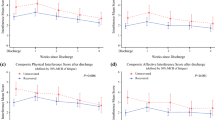
Based on the five most severe post-surgery symptoms (pain, fatigue, coughing, shortness of breath, and disturbed sleep), we identified three distinct symptom trajectories among 424 patients [mild, N = 225 (53.07%); severe-to-mild, N = 86 (20.28%); severe, N = 104 (24.53%)]. At discharge, more ‘severe’ patients (73.96%) did not achieve a functional recovery compared with those in mild (32.54%, P < 0.0001) or severe-to-mild (56.96%, P = 0.0274) groups. Factors of significant symptom increase on POD1 were younger-than-55 (OR = 1.94 [95% CI 1.30–2.93], P = 0.001), undergoing open or multi-port video-assisted thoracoscopic surgery (OR = 1.59 [95% CI 1.05–2.41], P = 0.03), and using two chest tubes (OR = 1.72 [95% CI 1.12–2.65], P = 0.01). For patients experiencing dramatic symptom increase on POD1, older age (OR = 2.51 [95% CI 1.40–4.59], P = 0.002) was associated with ‘severe’ trajectory.
Conclusions
This study demonstrated that PRO measures were capable of profiling heterogeneous symptom trajectories after lung cancer surgery. Those in-hospital trajectories were able to differentiate patients’ responses to treatments and signal the needs for extensive post-discharge care.



Similar content being viewed by others
References
Kluetz PG, Kanapuru B, Lemery S, et al. Informing the tolerability of cancer treatments using patient-reported outcome measures: Summary of an FDA and critical path institute workshop. Value Health. 2018;21(6):742–7. https://doi.org/10.1016/j.jval.2017.09.009.
Calvert M, Kyte D, Mercieca-Bebber R, et al. Guidelines for inclusion of patient-reported outcomes in clinical trial protocols: the SPIRIT-PRO extension. JAMA. 2018;319(5):483–94. https://doi.org/10.1001/jama.2017.21903.
Janelsins MC, Mohamed M, Peppone LJ, et al. Longitudinal changes in cognitive function in a nationwide cohort study of patients with lymphoma treated with chemotherapy. J Natl Cancer Inst. 2021. https://doi.org/10.1093/jnci/djab133.
Schoenbeck KL, Atallah E, Lin L, et al. Patient-reported functional outcomes in patients with chronic myeloid leukemia after stopping tyrosine kinase inhibitors. J Natl Cancer Inst. 2021. https://doi.org/10.1093/jnci/djab184.
Gonzalez BD, Eisel SL, Bowles KE, et al. Meta-analysis of quality of life in cancer patients treated with immune checkpoint inhibitors. J Natl Cancer Inst. 2021. https://doi.org/10.1093/jnci/djab171.
Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016;34(6):557–65. https://doi.org/10.1200/JCO.2015.63.0830.
Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27(7):2015–23. https://doi.org/10.1177/0962280216673085.
Wang XS, Fairclough DL, Liao Z, et al. Longitudinal study of the relationship between chemoradiation therapy for non-small-cell lung cancer and patient symptoms. J Clin Oncol. 2006;24(27):4485–91. https://doi.org/10.1200/JCO.2006.07.1126.
Cleeland CS, Mendoza TR, Wang XS, et al. Levels of symptom burden during chemotherapy for advanced lung cancer: differences between public hospitals and a tertiary cancer center. J Clin Oncol. 2011;29(21):2859–65. https://doi.org/10.1200/JCO.2010.33.4425.
Ferrat E, Paillaud E, Caillet P, et al. Performance of four frailty classifications in older patients with cancer: prospective elderly cancer patients cohort study. J Clin Oncol. 2017;35(7):766–77. https://doi.org/10.1200/JCO.2016.69.3143.
Ungar F, Ungar B, Alivisatos SG, Mosnaim AD, Wolf ME. Non-enzymic interactions of nicotinamide adenine dinucleotide, of some of its synthetic analogues and other compounds with orthophosphate. Res Commun Chem Pathol Pharmacol. 1979;25(2):395–8.
Dai W, Xie S, Zhang R, et al. Developing and validating utility parameters to establish patient-reported outcome-based perioperative symptom management in patients with lung cancer: a multicentre, prospective, observational cohort study protocol. BMJ Open. 2019;9(10):e030726. https://doi.org/10.1136/bmjopen-2019-030726.
Wei X, Yu H, Dai W, et al. Patient-reported outcomes of video-assisted thoracoscopic surgery versus thoracotomy for locally advanced lung cancer: a longitudinal cohort study. Ann Surg Oncol. 2021;28(13):8358–71. https://doi.org/10.1245/s10434-021-09981-1.
Bower JE, Bak K, Berger A, et al. Screening, assessment, and management of fatigue in adult survivors of cancer: an American society of clinical oncology clinical practice guideline adaptation. J Clin Oncol. 2014;32(17):1840–50. https://doi.org/10.1200/JCO.2013.53.4495.
Denlinger CS, Ligibel JA, Are M, et al. Survivorship: sleep disorders, version 1.2014. J Natl Compr Canc Netw. 2014;12(5):630–42. https://doi.org/10.6004/jnccn.2014.0067.
Molassiotis A, Smith JA, Bennett MI, et al. Clinical expert guidelines for the management of cough in lung cancer: report of a UK task group on cough. Cough. 2010;6:9. https://doi.org/10.1186/1745-9974-6-9.
Parshall MB, Schwartzstein RM, Adams L, et al. An official American thoracic society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4):435–52. https://doi.org/10.1164/rccm.201111-2042ST.
Swarm RA, Paice JA, Anghelescu DL, et al. Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(8):977–1007. https://doi.org/10.6004/jnccn.2019.0038.
Wang XS, Wang Y, Guo H, Mendoza TR, Hao XS, Cleeland CS. Chinese version of the M. D Anderson symptom inventory: validation and application of symptom measurement in cancer patients. Cancer. 2004;101(8):1890–901. https://doi.org/10.1002/cncr.20448.
Frost MH, Reeve BB, Liepa AM, Stauffer JW, Hays RD, Mayo FDAP-ROCMG. What is sufficient evidence for the reliability and validity of patient-reported outcome measures?. Value Health. 2007;10(Suppl 2):S94-S105. https://doi.org/10.1111/j.1524-4733.2007.00272.x
Cleeland CS. The M. D. Anderson Symptom Inventory User Guide. https://www.mdandersonorg/content/dam/mdanderson/documents/Departments-and-Divisions/Symptom-Research/MDASI_userguidepdf. 2009
Fagundes CP, Shi Q, Vaporciyan AA, et al. Symptom recovery after thoracic surgery: measuring patient-reported outcomes with the MD Anderson Symptom Inventory. J Thorac Cardiovasc Surg. 2015;150(3):613–92. https://doi.org/10.1016/j.jtcvs.2015.05.057.
Proust-Lima C, Philipps V, Liquet B. Estimation of extended mixed models using latent classes and latent processes: the R package lcmm. J Stat Softw. 2015;78(2)
Shi Q, Mendoza TR, Wang XS, Cleeland CS. Using a symptom-specific instrument to measure patient-reported daily functioning in patients with cancer. Eur J Cancer. 2016;67:83–90. https://doi.org/10.1016/j.ejca.2016.07.027.
Shi Q, Mendoza Tr Fau-Dueck AC, Dueck Ac Fau-Ma H, et al. Determination of mild, moderate, and severe pain interference in patients with cancer. (1872-6623 (Electronic))
FDA U. Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. https://www.fdagov/regulatory-information/search-fda-guidance-documents/patient-reported-outcome-measures-use-medical-product-development-support-labeling-claims. 2009
FDA U. Principles for Selecting, Developing, Modifying, and Adapting Patient-Reported Outcome Instruments for Use in Medical Device Evaluation. https://www.fdagov/regulatory-information/search-fda-guidance-documents/principles-selecting-developing-modifying-and-adapting-patient-reported-outcome-instruments-use. 2020
Vandrevala T, Senior V, Spring L, Kelliher L, Jones C. “Am I really ready to go home?”: a qualitative study of patients’ experience of early discharge following an enhanced recovery programme for liver resection surgery. Support Care Cancer. 2016;24(8):3447–54. https://doi.org/10.1007/s00520-016-3158-6.
de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503–13. https://doi.org/10.1056/NEJMoa1911793.
Kyte K, Ekstedt M, Rustoen T, Oksholm T. Longing to get back on track: patients’ experiences and supportive care needs after lung cancer surgery. J Clin Nurs. 2019;28(9–10):1546–54. https://doi.org/10.1111/jocn.14751.
Rajabiyazdi F, Alam R, Pal A, et al. Understanding the meaning of recovery to patients undergoing abdominal surgery. JAMA Surg. 2021. https://doi.org/10.1001/jamasurg.2021.1557.
Aahlin EK, von Meyenfeldt M, Dejong CH, et al. Functional recovery is considered the most important target: a survey of dedicated professionals. Perioper Med (Lond). 2014;3:5. https://doi.org/10.1186/2047-0525-3-5.
Park J, Neuman HB, Bennett AV, et al. Patient expectations of functional outcomes after rectal cancer surgery: a qualitative study. Dis Colon Rectum. 2014;57(2):151–7. https://doi.org/10.1097/DCR.0000000000000036.
Wang XS, Kamal M, Chen TH, et al. Assessment of physical function by subjective and objective methods in patients undergoing open gynecologic surgery. Gynecol Oncol. 2021;161(1):83–8. https://doi.org/10.1016/j.ygyno.2021.01.021.
Hensel M, Egerer G, Schneeweiss A, Goldschmidt H, Ho AD. Quality of life and rehabilitation in social and professional life after autologous stem cell transplantation. Ann Oncol. 2002;13(2):209–17. https://doi.org/10.1093/annonc/mdf031.
Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol. 2016;34(15):1732–40. https://doi.org/10.1200/JCO.2015.63.2232.
Blank TO, Bellizzi KM. A gerontologic perspective on cancer and aging. Cancer. 2008;112(11 Suppl):2569–76. https://doi.org/10.1002/cncr.23444.
Mao JJ, Armstrong K, Bowman MA, Xie SX, Kadakia R, Farrar JT. Symptom burden among cancer survivors: impact of age and comorbidity. J Am Board Fam Med. 2007;20(5):434–43. https://doi.org/10.3122/jabfm.2007.05.060225.
Wang Y, Li H, Ye H, et al. Postoperative infectious complications in elderly patients after elective surgery in China: results of a 7-day cohort study from the international surgical outcomes study. Psychogeriatrics. 2021;21(2):158–65. https://doi.org/10.1111/psyg.12648.
Cataldo JK, Paul S, Cooper B, et al. Differences in the symptom experience of older versus younger oncology outpatients: a cross-sectional study. BMC Cancer. 2013;13:6. https://doi.org/10.1186/1471-2407-13-6.
Oksholm T, Miaskowski C, Kongerud JS, et al. Does age influence the symptom experience of lung cancer patients prior to surgery? Lung Cancer. 2013;82(1):156–61. https://doi.org/10.1016/j.lungcan.2013.06.016.
Aloia TA, Lee JE, Vauthey JN, et al. Delayed recovery after pancreaticoduodenectomy: a major factor impairing the delivery of adjuvant therapy? J Am Coll Surg. 2007;204(3):347–55. https://doi.org/10.1016/j.jamcollsurg.2006.12.011.
Acknowledgement
We thank the patients and staff at the participating centers. We thank Yuxian Nie, Yaqin Wang, and Jia Liao for help with the data collection. We would also like to thank Editage (www.editage.com) for English language edits.
Funding
This work was supported by National Natural Science Foundation of China (No. 81872506).
Author information
Authors and Affiliations
Contributions
Conceptualization: QS, QL, CC, XW; Data curation: QS, LT, HY, WD, XW, QL, XY; Formal analysis: QS, LT, HY, XW; Funding acquisition: QS; Investigation: QS, LT, HY, XW, XW; Methodology: QS, LT, HY, XW; Project administration: QS, QL; Resources: LT, WD, XW; Software: QS, LT, HY; Supervision: HY, WD, XW; Validation: QS, LT, HY; Visualization: HY, WD, XW; Writing – original draft: QS, LT; Writing – review & editing: QS, LT, HY, WD, XW, QL, XY, XW, CC.
Corresponding author
Ethics declarations
Disclosure
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, L., Yu, H., Dai, W. et al. Symptom Trajectories Informing Patient Care After Lung Cancer Surgery: A Longitudinal Patient-Reported Outcome Study. Ann Surg Oncol 30, 2607–2617 (2023). https://doi.org/10.1245/s10434-022-13065-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-13065-z