Abstract
Introduction
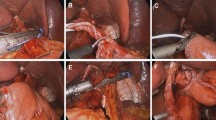
Overlap guiding tube (OGT)-assisted overlap oesophagojejunostomy (EJS), which was first designed and reported by our team, has shown feasibility. However, its safety and efficiency have not yet been compared with the conventional overlap approach.
Methods
We retrospectively analysed the data of 155 gastric/gastroesophageal junction (G/GEJ) cancer patients who underwent laparoscopic total gastrectomy by conventional (conventional group, n = 83) or OGT-assisted (OGT group, n = 72) overlap methods at Nanfang Hospital. The anastomotic efficiency and surgical outcomes were compared between the two groups.
Results
The success rate of inserting an anvil fork into the oesophageal lumen at the first attempt in the OGT group was much higher than in the conventional group (86.7% vs. 97.2%, P = 0.019). Consistently, the duration of EJS (P < 0.001) in the OGT group was significantly shorter than that in the conventional group. Operatively, there was one case in which oesophageal pseudocanals developed; another case was converted to thoracoscopic surgery in the conventional group, but there were no such cases in the OGT group. In terms of postoperative recovery, the OGT group was superior to the conventional group. The incidence of postoperative complications (28.9% vs. 20.8%, P = 0.247) and the classification of complication severity (P = 0.450) were milder in the OGT group, although the difference was not statistically significant. Notably, the conventional group had four cases (4.8%) of oesophagojejunal anastomotic leakage (EJAL) and one case (1.2%) of anastomotic stenosis. In the OGT group, two patients (2.8%) developed EJAL, but none developed anastomotic stenosis or anastomotic bleeding. Neither group had any cases of unplanned secondary surgery or perioperative deaths.
Conclusions
The OGT-assisted method reduced the surgical difficulty of overlap EJS with good safety. This study provides new perspectives for optimizing EJS.




Similar content being viewed by others
References
Hu Y, Huang C, Sun Y, et al. Morbidity and mortality of laparoscopic versus open d2 distal gastrectomy for advanced gastric cancer: a randomized controlled trial. J Clin Oncol. 2016;34:1350–7. https://doi.org/10.1200/JCO.2015.63.7215.
Yu J, Huang C, Sun Y, et al. Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial. JAMA. 2019. https://doi.org/10.1001/jama.2019.5359.
Chen XH, Hu YF, Luo J, et al. The safety of esophagojejunostomy via a transorally inserted-anvil method vs extracorporeal anastomosis using a circular stapler during total gastrectomy for Siewert type 2 adenocarcinoma of the esophagogastric junction. Gastroenterol Rep (Oxf). 2020. https://doi.org/10.1093/gastro/goz046.
Chen X, Luo J, Zhu Y, et al. Surgical safety of laparoscopic total gastrectomy with intracorporeal esophagojejunostomy via transoral anvil versus mini-laparotomy anastomosis: a propensity score matching analysis. Zhonghua Wei Chang Wai Ke Za Zhi. 2018;21:887–95.
Inaba K, Satoh S, Ishida Y, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg. 2010. https://doi.org/10.1016/j.jamcollsurg.2010.09.005.
Tsujimoto H, Uyama I, Yaguchi Y, et al. Outcome of overlap anastomosis using a linear stapler after laparoscopic total and proximal gastrectomy. Langenbecks Arch Surg. 2012. https://doi.org/10.1007/s00423-012-0939-3.
Morimoto M, Kitagami H, Hayakawa T, et al. The overlap method is safe and feasible for esophagojejunostomy after laparoscopic-assisted total gastrectomy. World J Surg Oncol. 2014. https://doi.org/10.1186/1477-7819-12-392.
Kitagami H, Morimoto M, Nakamura K, et al. Technique of Roux-en-Y reconstruction using overlap method after laparoscopic total gastrectomy for gastric cancer: 100 consecutively successful cases. Surg Endosc. 2016. https://doi.org/10.1007/s00464-015-4724-6.
Kawamura H, Ohno Y, Ichikawa N, et al. Anastomotic complications after laparoscopic total gastrectomy with esophagojejunostomy constructed by circular stapler (OrVil©) versus linear stapler (overlap method). Surg Endosc. 2017. https://doi.org/10.1007/s00464-017-5584-z.
Yoshikawa K, Shimada M, Higashijima J, et al. Usefulness of the transoral anvil delivery system for esophagojejunostomy after laparoscopic total gastrectomy: a single-institution comparative study of transoral anvil delivery system and the overlap method. Surg Laparosc Endosc Percutan Tech. 2018. https://doi.org/10.1097/SLE.0000000000000495.
Xinhua C, Tian L, Huilin H, et al. Application value of overlap guiding tube (OGT) in assisting overlap esophagojejunostomy during laparoscopic total gastrectomy for gastric/gastroesophageal junction (G/GEJ) tumors. Gastric Cancer. 2022. https://doi.org/10.1007/s10120-022-01296-8.
Amin MB, Greene FL, Edge SB, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017. https://doi.org/10.3322/caac.21388.
Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer (2021). https://doi.org/10.1007/s10120-020-01042-y.
Zhu Y, Chen XH, Li TT, et al. Method and experience of lymph node examination after gastrectomy with D2 lymphadenectomy for gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 2019. https://doi.org/10.3760/cma.j.issn.1671-0274.2019.08.018.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Schardey HM, Joosten U, Finke U, et al. The prevention of anastomotic leakage after total gastrectomy with local decontamination. A prospective, randomized, double-blind, placebo-controlled multicenter trial. Ann Surg. 1997. https://doi.org/10.1097/00000658-199702000-00005.
Umemura A, Koeda K, Sasaki A, et al. Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg. 2015. https://doi.org/10.1016/j.asjsur.2014.09.006.
Meng M, Dong SX, Liu DM. Totally laparoscopic total gastrectomy by using modified overlap esophagojejunostomy, clinical report of 36 cases. Chin J Oper Proced Gen Surg (Electron Ed). 2021. https://doi.org/10.3877/cma.j.issn.1674-3946.2021.02.016.
Chen C, Wei M, Han HF. Comparison of reverse puncture device and overlap in laparoscopic total gastrectomy for gastric cancer. J Laparosc Surg. 2020. https://doi.org/10.13499/j.cnki.fqjwkzz.2020.01.025.
Xie SP, Fan GH, Kang GJ, et al. Esophageal reconstruction with remnant stomach: a case report and review of literature. World J Gastroenterol. 2013. https://doi.org/10.3748/wjg.v19.i20.3169.
Kamarajah SK, Navidi M, Griffin SM, et al. Impact of anastomotic leak on long-term survival in patients undergoing gastrectomy for gastric cancer. Br J Surg. 2020. https://doi.org/10.1002/bjs.11749.
Watanabe M, Miyata H, Gotoh M, et al. Total gastrectomy risk model: Data from 20,011 Japanese patients in a nationwide internet-based database. Ann Surg. 2014. https://doi.org/10.1097/SLA.0000000000000781.
Schietroma M, Cecilia EM, Carlei F, et al. Prevention of anastomotic leakage after total gastrectomy with perioperative supplemental oxygen administration: a prospective randomized, double-blind, controlled, single-center trial. Ann Surg Oncol. 2013. https://doi.org/10.1245/s10434-012-2714-7.
Lin T, Mou TY, Hu YF, et al. Reduced port laparoscopic distal gastrectomy with d2 lymphadenectomy. Ann Surg Oncol. 2018. https://doi.org/10.1245/s10434-017-6066-1.
Lu YM, Lin T, Hu YF, et al. Initial experience of dual-port laparoscopic distal gastrectomy for gastric cancer: a single-arm study. Adv Ther. 2019;36(9):2342–50. https://doi.org/10.1007/s12325-019-01029-x.
Kim HB, Kim SM, Ha MH, et al. Comparison of reduced port totally laparoscopic-assisted total gastrectomy (Duet TLTG) and conventional laparoscopic-assisted total gastrectomy. Surg Laparosc Endosc Percutan Tech. 2016. https://doi.org/10.1097/SLE.0000000000000329.
Kim SM, Ha MH, Seo JE, et al. Comparison of reduced port totally laparoscopic distal gastrectomy (Duet TLDG) and conventional laparoscopic-assisted distal gastrectomy. Ann Surg Oncol. 2015. https://doi.org/10.1245/s10434-014-4333-y.
Kawamura H, Tanioka T, Kuji M, et al. The initial experience of dual port laparoscopy-assisted total gastrectomy as a reduced port surgery for total gastrectomy. Gastric Cancer. 2013. https://doi.org/10.1007/s10120-012-0212-z.
Acknowledgement
This work was supported by grants from the Guangdong Provincial Key Laboratory of Precision Medicine for Gastrointestinal Cancer (2020B121201004) and the Clinical Research Program of Nanfang Hospital, Southern Medical University (2021CR001). Many thanks are extended to Dr Mengyao Li for drawing the outline of the OGT-assisted overlap method.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
The authors declare no conflict of interest.
Ethics Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for such consent was obtained from all patients for inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 88400 KB)
Supplementary file2 (MP4 35735 KB)
Supplementary file3 (MP4 46319 KB)
Supplementary file4 (MP4 44449 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, X., Lin, T., Zhao, M. et al. Safety and Efficacy of OGT-Assisted Overlap Oesophagojejunostomy Versus the Traditional Overlap Method in Laparoscopic Total Gastrectomy for Gastric/Gastroesophageal Junction (G/GEJ) Tumours. Ann Surg Oncol 30, 2729–2738 (2023). https://doi.org/10.1245/s10434-022-13031-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-13031-9