Abstract
Background
Local en bloc resection of pT1 colon cancer has been gaining acceptance during the last few years. In the absence of histological risk factors, the risk of lymph-node metastases (LNM) is negligible and does not outweigh the morbidity and mortality of an oncologic resection. Colonoscopy-assisted laparoscopic wedge resection (CAL-WR) has proved to be an effective and safe technique for removing complex benign polyps. The role of CAL-WR for the primary resection of suspected T1 colon cancer has to be established.
Methods
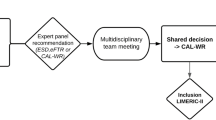
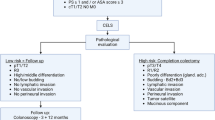
This retrospective study aimed to determine the radicality and safety of CAL-WR as a local en bloc resection technique for a suspected T1 colon cancer. Therefore, the study identified patients in whom high-grade dysplasia or a T1 colon carcinoma was suspected based on histology and/or macroscopic assessment, requiring an en bloc resection.
Results
The study analyzed 57 patients who underwent CAL-WR for a suspected macroscopic polyp or polyps with biopsy-proven high-grade dysplasia or T1 colon carcinoma. For 27 of these 57 patients, a pT1 colon carcinoma was diagnosed at pathologic examination after CAL-WR. Histological risk factors for LNM were present in three cases, and 70% showed deep submucosal invasion (Sm2/Sm3). For patients with pT1 colon carcinoma, an overall R0-resection rate of 88.9% was achieved. A minor complication was noted in one patient (1.8%).
Conclusions
The CAL-WR procedure is an effective and safe technique for suspected high-grade dysplasia or T1-colon carcinoma. It may fill the gap for tumors that are macroscopic suspected for deep submucosal invasion, providing more patients an organ-preserving treatment option.


Similar content being viewed by others
References
Ebbehøj AL, Jørgensen LN, Krarup P, Smith HG. Histopathological risk factors for lymph node metastases in T1 colorectal cancer: meta-analysis. Br J Surg. 2021;108:769–776. https://doi.org/10.1093/bjs/znab168.
Argilés G, Tabernero J, Labianca R, et al. Localised colon cancer: ESMO clinical practice guidelines for diagnosis, treatment, and follow-up. Ann Oncol. 2020;31:1291–305. https://doi.org/10.1016/j.annonc.2020.06.022.
Benson AB, Venook AP, Al-Hawary MM, et al. Colon cancer, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021;19:329–59. https://doi.org/10.6004/jnccn.2021.0012.
Ueno H, Hase K, Hashiguchi Y, et al. Site-specific tumor grading system in colorectal cancer: multicenter pathologic review of the value of quantifying poorly differentiated clusters. Am J Surg Pathol. 2014;38:197–204. https://doi.org/10.1097/PAS.0000000000000113.
Wada H, Shiozawa M, Katayama K, et al. Systematic review and meta-analysis of histopathological predictive factors for lymph node metastasis in T1 colorectal cancer. J Gastroenterol. 2015;50:727–34. https://doi.org/10.1007/s00535-015-1057-0.
Shaukat A, Kaltenbach T, Dominitz JA, et al. Endoscopic recognition and management strategies for malignant colorectal polyps: recommendations of the US multi-society task force on colorectal cancer. Gastroenterology. 2020;159:1916-34.e2. https://doi.org/10.1053/j.gastro.2020.08.050.
Yoshii S, Nojima M, Nosho K, et al. Factors associated with risk for colorectal cancer recurrence after endoscopic resection of T1 tumors. Clin Gastroenterol Hepatol. 2014;12:292-302.e3. https://doi.org/10.1016/j.cgh.2013.08.008.
Backes Y, de Vos tot Nederveen Cappel WH, van Bergeijk J, et al. Risk for incomplete resection after macroscopic radical endoscopic resection of T1 colorectal cancer: a multicenter cohort study. ACG. 2017;112:785–96. https://doi.org/10.1038/ajg.2017.58.
Ikematsu H, Yoda Y, Matsuda T, et al. Long-term outcomes after resection for submucosal invasive colorectal cancers. Gastroenterology. 2013;144:551–9. https://doi.org/10.1053/j.gastro.2012.12.003.
Vermeer NCA, Backes Y, Snijders HS, et al. National cohort study on postoperative risks after surgery for submucosal invasive colorectal cancer. BJS Open. 2019;3:210–7. https://doi.org/10.1002/bjs5.50125.
Zwager LW, Bastiaansen BAJ, Montazeri NSM, et al. Deep submucosal invasion is not an independent risk factor for lymphnode metastasis in T1 colorectal cancer: a meta-analysis. Gastroenterology. 2022. https://doi.org/10.1053/j.gastro.2022.04.010.
Watanabe D, Toyonaga T, Ooi M, et al. Clinical outcomes of deep invasive submucosal colorectal cancer after ESD. Surg Endosc. 2018;32:2123–30. https://doi.org/10.1007/s00464-017-5910-5.
Zwager LW, Bastiaansen BAJ, Bronzwaer MES, et al. Endoscopic full-thickness resection (eFTR) of colorectal lesions: results from the Dutch colorectal eFTR registry. Endoscopy. 2020;52:1014–23. https://doi.org/10.1055/a-1176-1107.
Kuellmer A, Mueller J, Caca K, et al. Endoscopic full-thickness resection for early colorectal cancer. Gastrointest Endosc. 2019;89:1180–9. https://doi.org/10.1016/j.gie.2018.12.025.
Didden P, van Eijck van Heslinga RAH, Schwartz MP, et al. Relevance of polyp size for primary endoscopic full-thickness resection of suspected T1 colorectal cancers. Endoscopy. 2022. https://doi.org/10.1055/a-1790-5539.
Backes Y, Schwartz MP, Ter Borg F, et al. Multicentre prospective evaluation of real-time optical diagnosis of T1 colorectal cancer in large non-pedunculated colorectal polyps using narrow band imaging (the OPTICAL study). Gut. 2019;68:271–9. https://doi.org/10.1136/gutjnl-2017-314723.
Noren ER, Wickham C, Lee SW. Current techniques for combined endoscopic and laparoscopic surgery (CELS). Ann Laparosc Endosc Surg. 2019. https://doi.org/10.21037/ales.2019.05.07.
Leicher LW, Huisman JF, van Grevenstein WM U, et al. Colonoscopic-assisted laparoscopic wedge resection for colonic lesions: a prospective multicentre cohort study (LIMERIC-study). Ann Surg. 2022. https://doi.org/10.1097/SLA.0000000000005417.
Leicher LW, de VosTot Nederveen Cappel WH, van Westreenen HL. Limited endoscopic-assisted wedge resection for excision of colon polyps. Dis Colon Rectum. 2017;60:299–2. https://doi.org/10.1097/DCR.0000000000000716.
Giavarini L, Boni L, Cortellezzi CC, et al. Laparoscopic caecal wedge resection with intraoperative endoscopic assistance. Int J Surg. 2013;11:S58-60. https://doi.org/10.1016/S1743-9191(13)60018-7.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Gijsbers KM, van derSchee L, Vanveen T, et al. Impact of ≥0.1-mm free resection margins on local intramural residual cancer after local excision of T1 colorectal cancer. Endosc Int Open. 2022;10:282–90. https://doi.org/10.1055/a-1736-6960.
Leicher LW, de Vos Tot Nederveen Cappel WH, van Westreenen HL. Limited endoscopic-assisted wedge resection for excision of colon polyps. Dis Colon Rectum. 2017;60:299–302. https://doi.org/10.1097/DCR.0000000000000716.
Fuccio L, Repici A, Hassan C, et al. Why attempt en bloc resection of non-pedunculated colorectal adenomas? A systematic review of the prevalence of superficial submucosal invasive cancer after endoscopic submucosal dissection. Gut. 2018;67:1464–74. https://doi.org/10.1136/gutjnl-2017-315103.
Overwater A, Kessels K, Elias SG, et al. Endoscopic resection of high-risk T1 colorectal carcinoma prior to surgical resection has no adverse effect on long-term outcomes. Gut. 2018;67:284–90. https://doi.org/10.1136/gutjnl-2015-310961.
Nian J, Tao L, Zhou W. Prior endoscopic resection does not affect the outcome of secondary surgery for T1 colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2022;37:273–81. https://doi.org/10.1007/s00384-021-04049-8.
Oh EH, Kim N, Hwang SW, et al. Comparison of long-term recurrence-free survival between primary surgery and endoscopic resection followed by secondary surgery in T1 colorectal cancer. Gastrointest Endosc. 2021;94:394–404. https://doi.org/10.1016/j.gie.2021.02.021.
Takamaru H, Saito Y, Sekiguchi M, et al. Endoscopic resection before surgery does not affect the recurrence rate in patients with high-risk T1 colorectal cancer. Clin Transl Gastroenterol. 2021;12:00336. https://doi.org/10.14309/ctg.0000000000000336.
Yamaoka Y, Imai K, Shiomi A, et al. Endoscopic resection of T1 colorectal cancer prior to surgery does not affect surgical adverse events and recurrence. Surg Endosc. 2020;34:5006–16. https://doi.org/10.1007/s00464-019-07295-8.
Koyama Y, Yamada M, Makiguchi ME, et al. New scoring system to distinguish deep invasive submucosal and muscularis propria colorectal cancer during colonoscopy: a development and global multicenter external validation study (e-T2 score). Gastrointest Endosc. 2022. https://doi.org/10.1016/j.gie.2022.03.002.
Group E. C. The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an international registry. Ann Surg. 2015;261:1153–9. https://doi.org/10.1097/SLA.0000000000001029.
Tweed TTT, Woortman C, Tummers S, Bakens Maikel JA. M, van Bastelaar J, Stoot JHMB. Reducing hospital stay for colorectal surgery in ERAS setting by means of perioperative patient education of expected day of discharge. Int J Colorectal Dis. 2021;36:1535–42. https://doi.org/10.1007/s00384-021-03948-0.
Govaert JA, Fiocco M, van Dijk WA, et al. Multicenter stratified comparison of hospital costs between laparoscopic and open colorectal cancer resections: influence of tumor location and operative risk. Ann Surg. 2017;266:1021–8. https://doi.org/10.1097/SLA.0000000000002000.
Jayaram A, Barr N, Plummer R, Yao M, Chen L, Yoo J. Combined endo-laparoscopic surgery (CELS) for benign colon polyps: a single-institution cost analysis. Surg Endosc. 2019;33:3238–42. https://doi.org/10.1007/s00464-018-06610-z.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
DISCLOSURE
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hanevelt, J., Moons, L.M.G., Hentzen, J.E.K.R. et al. Colonoscopy-Assisted Laparoscopic Wedge Resection for the Treatment of Suspected T1 Colon Cancer. Ann Surg Oncol 30, 2058–2065 (2023). https://doi.org/10.1245/s10434-022-12973-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12973-4