Abstract
Background
Frailty is a physiologic state that affects perioperative outcomes. Studies evaluating the impact of frailty on long-term oncologic outcomes are limited. This study evaluated perioperative and long-term oncologic outcomes for elderly patients undergoing colorectal surgery.
Methods
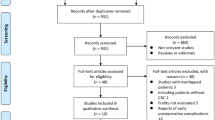
Patients older than 65 years at the time of colorectal resection between July 2011 and September 2020 at Roswell Park Comprehensive Cancer Center were identified. Variables from the National Surgical Quality Improvement Program (NSQIP), the tumor registry, and electronic medical records (EMRs) were used to identify frail patients using the revised Risk Analysis Index (RAI-A) score. A score of 38 or higher defined a patient as “frail.” Perioperative outcomes were evaluated using logistic regression and chi-square, and oncologic outcomes were evaluated using Kaplan-Meier analysis.
Results
The study analyzed 411 patients. The mean age at surgery was 75.1 years. The median RAI-A score was 37, and 29.9 % of the patients were frail. The frail patients had significantly higher rates of overall complications (30.1 % vs 14.6 %; p < 0.001). They also had significantly higher rates of postoperative hospitalization longer than 30 days, postoperative delirium, and discharge to rehabilitation. No mortality differences were observed. The 318 patients with colorectal adenocarcinoma undergoing curative-intent resection were evaluated for oncologic outcomes. No differences with frailty in terms of overall survival, disease-specific survival, or progression-free survival were observed except for frail patients with stage 0 or 1 adenocarcinoma, who had worse overall survival than non-frail patients but equivalent other outcomes.
Conclusions
For elderly patients undergoing colorectal surgery, frailty is associated with higher postoperative complications, discharge to rehabitation, and prolonged hospitalization rates. Frailty does not affect long-term oncologic outcomes, so frail elderly patients gain the same oncologic benefit with surgery as non-frail patients.


Similar content being viewed by others
References
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. https://doi.org/10.1093/gerona/56.3.m146. (PubMed PMID: 11253156).
Hall DE, Arya S, Schmid KK, Blaser C, Carlson MA, Bailey TL, et al. Development and initial validation of the risk analysis index for measuring frailty in surgical populations. JAMA Surg. 2017;152:175–82. https://doi.org/10.1001/jamasurg.2016.4202.PubMedPMID:27893030;PubMedCentralPMCID:PMCPMC7140150.
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901–8. Epub 2010/04/28. https://doi.org/10.1016/j.jamcollsurg.2010.01.028. (PubMed PMID: 20510798).
Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC, Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206:544–50. Epub 2013/07/20. Doi: https://doi.org/10.1016/j.amjsurg.2013.03.012. (PubMed PMID: 23880071; PubMed Central PMCID: PMCPMC3788864).
Huisman MG, van Leeuwen BL, Ugolini G, Montroni I, Spiliotis J, Stabilini C, et al. “Timed Up & Go”: a screening tool for predicting 30-day morbidity in onco-geriatric surgical patients? A multicenter cohort study. PloS One. 2014;9:e86863. Epub 2014/01/24. Doi: https://doi.org/10.1371/journal.pone.0086863. (PubMed PMID: 24475186; PubMed Central PMCID: PMCPMC3901725).
Vitzthum LK, Feng CH, Noticewala S, Hines PJ, Nguyen C, Zakeri K, et al. Comparison of comorbidity and frailty indices in patients with head and neck cancer using an online tool. JCO Clin Cancer Inform. 2018;2:1–9. https://doi.org/10.1200/CCI.18.00082. (PubMed PMID: 30652602).
Hersh AM, Pennington Z, Hung B, et al. Comparison of frailty metrics and the Charlson Comorbidity Index for predicting adverse outcomes in patients undergoing surgery for spine metastases. J Neurosurg Spine. 2022;36(5):849–857. https://doi.org/10.3171/2021.8.SPINE21559. (PubMed PMID: 34826820).
Turner G, Clegg A, Society BG, UK A, Practioners RcoG. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing. 2014;43:744–7. Doi: https://doi.org/10.1093/ageing/afu138. (PubMed PMID: 25336440).
Subra J, Gillette-Guyonnet S, Cesari M, Oustric S, Vellas B, Team P. The integration of frailty into clinical practice: preliminary results from the Gérontopôle. J Nutr Health Aging. 2012;16:714–20. https://doi.org/10.1007/s12603-012-0391-7. (PubMed PMID: 23076514).
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x. (PubMed PMID: 1991946).
Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13:881–9. Doi: https://doi.org/10.1007/s12603-009-0246-z. (PubMed PMID: 19924348).
Arya S, Varley P, Youk A, Borrebach JD, Perez S, Massarweh NN, et al. Recalibration and external validation of the Risk Analysis Index: a surgical frailty assessment tool. Ann Surg. 2020;272:996–1005. https://doi.org/10.1097/SLA.0000000000003276.PubMedPMID:30907757;PubMedCentralPMCID:PMCPMC8785437.
Kristjansson SR, Nesbakken A, Jordhøy MS, Skovlund E, Audisio RA, Johannessen HO, et al. Comprehensive geriatric assessment can predict complications in elderly patients after elective surgery for colorectal cancer: a prospective observational cohort study. Crit Rev Oncol Hematol. 2010;76:208–17. Epub 2009/12/14. Doi: https://doi.org/10.1016/j.critrevonc.2009.11.002. (PubMed PMID: 20005123).
Tan KY, Kawamura YJ, Tokomitsu A, Tang T. Assessment for frailty is useful for predicting morbidity in elderly patients undergoing colorectal cancer resection whose comorbidities are already optimized. Am J Surg. 2012;204:139–43. Epub 2011/12/16. Doi: https://doi.org/10.1016/j.amjsurg.2011.08.012. (PubMed PMID: 22178483).
Reisinger KW, van Vugt JL, Tegels JJ, Snijders C, Hulsewé KW, Hoofwijk AG, et al. Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg. 2015;261:345–52. https://doi.org/10.1097/SLA.0000000000000628. (PubMed PMID: 24651133).
Shah R, Attwood K, Arya S, Hall DE, Johanning JM, Gabriel E, et al. Association of frailty with failure to rescue after low-risk and high-risk inpatient surgery. JAMA Surg. 2018;153:e180214. Epub 20180516. Doi: https://doi.org/10.1001/jamasurg.2018.0214. (PubMed PMID: 29562073; PubMed Central PMCID: PMCPMC5875343).
Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, et al. Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg. 2020;155:233–42. https://doi.org/10.1001/jamasurg.2019.5474.PubMedPMID:31968063;PubMedCentralPMCID:PMCPMC6990653.
Carli F, Gillis C, Scheede-Bergdahl C. Promoting a culture of prehabilitation for the surgical cancer patient. Acta Oncol. 2017;56:128–33. Epub 2017/01/09. Doi: https://doi.org/10.1080/0284186X.2016.1266081. (PubMed PMID: 28067101).
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS, et al. Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc. 2013;27:1072–82. Epub 20121009. Doi: https://doi.org/10.1007/s00464-012-2560-5. (PubMed PMID: 23052535).
Bousquet-Dion G, Awasthi R, Loiselle S, Minnella EM, Agnihotram RV, Bergdahl A, et al. Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol. 2018;57:849–59. Epub 20180112. Doi: https://doi.org/10.1080/0284186X.2017.1423180. (PubMed PMID: 29327644).
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121:937–47. https://doi.org/10.1097/ALN.0000000000000393. (PubMed PMID: 25076007).
Trépanier M, Minnella EM, Paradis T, Awasthi R, Kaneva P, Schwartzman K, et al. Improved disease-free survival after prehabilitation for colorectal cancer surgery. Ann Surg. 2019;270:493–501. https://doi.org/10.1097/SLA.0000000000003465. (PubMed PMID: 31318793).
van Rooijen SJ, Molenaar CJL, Schep G, van Lieshout RHMA, Beijer S, Dubbers R, et al. Making patients fit for surgery: introducing a four-pillar multimodal prehabilitation program in colorectal cancer. Am J Phys Med Rehabil. 2019;98:888–96. https://doi.org/10.1097/PHM.0000000000001221. (PubMed PMID: 31090551).
McIsaac DI, Saunders C, Hladkowicz E, Bryson GL, Forster AJ, Gagne S, et al. PREHAB study: a protocol for a prospective randomised clinical trial of exercise therapy for people living with frailty having cancer surgery. BMJ Open. 2018;8:e022057. Epub 20180622. Doi: https://doi.org/10.1136/bmjopen-2018-022057. (PubMed PMID: 29934394; PubMed Central PMCID: PMCPMC6020976).
Ommundsen N, Wyller TB, Nesbakken A, Jordhøy MS, Bakka A, Skovlund E, et al. Frailty is an independent predictor of survival in older patients with colorectal cancer. Oncologist. 2014;19:1268–75. Epub 2014/10/29. Doi: https://doi.org/10.1634/theoncologist.2014-0237. (PubMed PMID: 25355846; PubMed Central PMCID: PMCPMC4257747).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdelfatah, E., Ramos-Santillan, V., Cherkassky, L. et al. High Risk, High Reward: Frailty in Colorectal Cancer Surgery is Associated with Worse Postoperative Outcomes but Equivalent Long-Term Oncologic Outcomes. Ann Surg Oncol 30, 2035–2045 (2023). https://doi.org/10.1245/s10434-022-12970-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12970-7