Abstract
Background
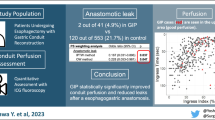
Impaired gastric conduit perfusion during esophagectomy and reconstruction is considered a key risk factor of anastomotic leaks. The aim of this study is to evaluate the indication and feasibility of additional microvascular anastomosis (AMA) to the gastric conduit in esophageal cancer surgery.
Patients and Methods
Patients who received an esophagectomy with gastric conduit reconstruction between July 2008 and July 2021 at a single center were reviewed. Patient characteristics, anastomotic viability index (AVI) of the gastric conduit measured with thermal imaging, and operative outcomes were analyzed using Fisher’s exact test and Mann–Whitney U test. Two propensity score weighting methods (inverse probability of treatment weighting and overlap weighting) were applied to investigate whether AMA reduces anastomotic leaks.
Results
Of the 293 patients who underwent an esophagectomy over the study period, 26 received AMA. AVI in the AMA group was significantly lower than that in the control group (0.64 vs. 0.74, p = 0.026). Overall anastomotic leak rates were 3.8% in the AMA group and 12.4% in the control group. Using two different propensity score weighting methods, the same conclusion was obtained that AMA significantly reduced anastomotic leaks after esophagectomy (both p < 0.001). The logistic regression model for estimating probability of anastomotic leaks provided AVI criteria for AMA application and revealed that AMA significantly reduced the estimated leak rates by a maximum of 49%.
Conclusions
Additional microvascular anastomosis significantly reduced anastomotic leaks after esophagectomy. The proposed AVI criteria for AMA application can help guide surgeons as to when AMA is needed.



Similar content being viewed by others
Data availability
The data underlying this article will be shared upon reasonable request to the corresponding author.
References
Raymond DP, Seder CW, Wright CD, et al. Predictors of major morbidity or mortality after resection for esophageal cancer: a society of thoracic surgeons general thoracic surgery database risk adjustment model. Ann Thorac Surg. 2016;102:207–14.
Markar SR, Arya S, Karthikesalingam A, et al. Technical factors that affect anastomotic integrity following esophagectomy: systematic review and meta-analysis. Ann Surg Oncol. 2013;20:4274–81.
Ishikawa Y, Breuler C, Chang AC, et al. Quantitative perfusion assessment of gastric conduit with indocyanine green dye to predict anastomotic leak after esophagectomy. Dis Esophagus. 2022;35(5):doab079. https://doi.org/10.1093/dote/doab079.
Nishikawa K, Fujita T, Yuda M, et al. Quantitative assessment of blood flow in the gastric conduit with thermal imaging for esophageal reconstruction. Ann Surg. 2020;271:1087–94.
Fujioka M, Hayashida K, Fukui K, et al. Venous superdrained gastric tube pull-up procedure for hypopharyngeal and cervical esophageal reconstruction reduces postoperative anastomotic leakage and stricture. Dis Esophagus. 2017;30:1–6.
Takeda FR, Tutihashi R, Tustumi F, et al. Supercharged cervical anastomosis for esophagectomy and gastric pull-up. J Thorac Cardiovasc Surg. 2021;162:688–97.
Coral RP, Constant-Neto M, Silva IS, et al. Comparative anatomical study of the anterior and posterior mediastinum as access routes after esophagectomy. Dis Esophagus. 2003;16(3):236–8. https://doi.org/10.1046/j.1442-2050.2003.00335.x.
Rice TW, Kelsen DP, Blackstone EH, et al. Esophagus and esophagogastric junction. In: MB Amin, SB Edge, FL Greene, et al., editors. AJCC cancer staging manual. 8th edn. New York: Springer; 2017. p. 185–202.
Low DE, Alderson D, Cecconello I, et al. International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg. 2015;262:286–94.
Li F, Thomas LE, Li F. Addressing extreme propensity scores via the overlap weights [published correction appears in Am J Epidemiol. 2021 Jan 4, 190(1), pp. 189–190]. Am J Epidemiol. 2019;188:250–7.
Kawai KI, Kakibuchi M, Sakagami M, et al. Supercharged gastric tube pull-up procedure for total esophageal reconstruction. Ann Plast Surg. 2001;47:390–3.
Yoshimi F, Asato Y, Ikeda S, et al. Using the supercharge technique to additionally revascularize the gastric tube after a subtotal esophagectomy for esophageal cancer. Am J Surg. 2006;191:284–7.
Mao H, Li L, Greene T. Propensity score weighting analysis and treatment effect discovery. Stat Methods Med Res. 2019;28:2439–54.
Kono K, Sugai H, Omata H, et al. Transient bloodletting of the short gastric vein in the reconstructed gastric tube improves gastric microcirculation during esophagectomy. World J Surg. 2007;31(4):780–6.
Yukaya T, Saeki H, Kasagi Y, et al. Indocyanine green fluorescence angiography for quantitative evaluation of gastric tube perfusion in patients undergoing esophagectomy. J Am Coll Surg. 2015;221:e37–42.
Acknowledgement
The authors would like to thank Lili Zhao, PhD, Department of Biostatistics, University of Michigan, for the statistics consultation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None of the authors has anything relevant to disclose. This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishikawa, Y., Nishikawa, K., Takahashi, K. et al. Additional Microvascular Anastomosis to Gastric Conduit During Esophagectomy Reduces Anastomotic Leaks: Propensity Score Weighting Study. Ann Surg Oncol 30, 874–881 (2023). https://doi.org/10.1245/s10434-022-12737-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12737-0