Abstract
Background
The short-term outcome and long-term survival of pancreaticoduodenectomy with additional para-aortic dissection (PAD) for patients with resectable pancreatic cancer remain obscure.
Patients and Methods
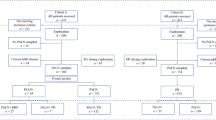
Consecutive patients who underwent radical pancreaticoduodenectomy for resectable pancreatic cancer in a single high-volume center during a 7-year period were included retrospectively. Both short- and long-term effects of PAD were compared between the PAD group and the no PAD group. Then, the PAD group was divided into the non-metastatic para-aortic lymph node (PALN−) group and the metastatic PALN (PALN+) group to further analyze the prognosis of PALN+.
Results
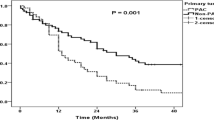
Of the 909 included patients, 280 (30.8%) underwent PAD during pancreaticoduodenectomy. The PAD group had a higher rate of intra-abdominal infection compared with the no PAD group (28.6% vs. 20.7%, P = 0.009) but no differences were found in the incidence of other complications. The overall survival (OS) and recurrence-free survival (RFS) were also comparable between the two groups. Subgroup analysis showed that patients with PALN+ had a worse OS than patients in the PALN− group (median of 14 vs. 20 months, P = 0.048). Multivariate Cox regression analysis further revealed that PALN+ was an independent adverse predictor of OS (hazard ratio: 1.70, P = 0.007).
Conclusions
This study suggests that the addition of PAD during pancreaticoduodenectomy does not improve the prognosis of patients with resectable pancreatic cancer and may lead to an increased risk of infection. However, the accurate preoperative assessment and appropriate treatment strategy for patients with PALN+ need further investigation due to the poor prognosis.



Similar content being viewed by others
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics 2022. CA Cancer J Clin. 2022;72(1):7–33.
Nimura Y, Nagino M, Takao S, et al. Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci. 2012;19(3):230–41.
Jang JY, Kang MJ, Heo JS, et al. A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg. 2014;259(4):656–64.
Jang JY, Kang JS, Han Y, et al. Long-term outcomes and recurrence patterns of standard versus extended pancreatectomy for pancreatic head cancer: a multicenter prospective randomized controlled study. J Hepatobiliary Pancreat Sci. 2017;24(7):426–33.
Staerkle RF, Vuille-Dit-Bille RN, Soll C, et al. Extended lymph node resection versus standard resection for pancreatic and periampullary adenocarcinoma. Cochrane Database Syst Rev. 2021. https://doi.org/10.1002/14651858.CD011490.pub2.
Tol JA, Gouma DJ, Bassi C, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2014;156(3):591–600.
Peparini N. Paraaortic dissection in “total mesopancreas excision” and “mesopancreas-first resection” pancreaticoduodenectomies for pancreatic cancer: useless, optional, or necessary? A systematic review. Surg Oncol. 2021;38:101639.
Yi S, Nagakawa Y, Ren K, et al. The mesopancreas and pancreatic head plexus: morphological, developmental, and clinical perspectives. Surg Radiol Anat. 2020;42(12):1501–8.
Komo T, Murakami Y, Kondo N, et al. Prognostic impact of para-aortic lymph node micrometastasis in pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2016;23(6):2019–27.
Shimada K, Sakamoto Y, Sano T, Kosuge T. The role of paraaortic lymph node involvement on early recurrence and survival after macroscopic curative resection with extended lymphadenectomy for pancreatic carcinoma. J Am Coll Surg. 2006;203(3):345–52.
Sperti C, Gruppo M, Blandamura S, et al. Para-aortic node involvement is not an independent predictor of survival after resection for pancreatic cancer. World J Gastroenterol. 2017;23(24):4399–406.
Sakai M, Nakao A, Kaneko T, et al. Para-aortic lymph node metastasis in carcinoma of the head of the pancreas. Surgery. 2005;137(6):606–11.
Safi SA, Rehders A, Haeberle L, et al. Para-aortic lymph nodes and ductal adenocarcinoma of the pancreas: distant neighbors? Surgery. 2021;170(6):1807–14.
Schwarz L, Lupinacci RM, Svrcek M, et al. Para-aortic lymph node sampling in pancreatic head adenocarcinoma. Br J Surg. 2014;101(5):530–8.
Sho M, Murakami Y, Motoi F, et al. Postoperative prognosis of pancreatic cancer with para-aortic lymph node metastasis: a multicenter study on 822 patients. J Gastroenterol. 2015;50(6):694–702.
Pranger BK, Tseng DSJ, Ubels S, et al. How to approach para-aortic lymph node metastases during exploration for suspected periampullary carcinoma: resection or bypass? Ann Surg Oncol. 2020;27(8):2949–58.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg. 2004;240(2):205–13.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Hirai I, Murakami G, Kimura W, Nara T, Dodo Y. Long descending lymphatic pathway from the pancreaticoduodenal region to the para-aortic nodes: its laterality and topographical relationship with the celiac plexus. Okajimas Folia Anat Jpn. 2001;77(6):189–99.
Hirono S, Tani M, Kawai M, et al. Identification of the lymphatic drainage pathways from the pancreatic head guided by indocyanine green fluorescence imaging during pancreaticoduodenectomy. Dig Surg. 2012;29(2):132–9.
Bouassida M, Mighri MM, Chtourou MF, et al. Retroportal lamina or mesopancreas? Lessons learned by anatomical and histological study of thirty three cadaveric dissections. Int J Surg. 2013;11(9):834–6.
Sharma D, Isaji S. Mesopancreas is a misnomer: time to correct the nomenclature. J Hepatobiliary Pancreat Sci. 2016;23(12):745–9.
Fernandes ESM, Strobel O, Girao C, Moraes-Junior JMA, Torres OJM. What do surgeons need to know about the mesopancreas. Langenbecks Arch Surg. 2021;406(8):2621–32.
Xu J, Tian X, Chen Y, et al. Total mesopancreas excision for the treatment of pancreatic head cancer. J Cancer. 2017;8(17):3575–84.
Inoue Y, Saiura A, Yoshioka R, et al. Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg. 2015;262(6):1092–101.
Shyr BU, Shyr BS, Chen SC, Shyr YM, Wang SE. Mesopancreas level 3 dissection in robotic pancreaticoduodenectomy. Surgery. 2021;169(2):362–8.
Peparini N, Chirletti P. Mesopancreas: a boundless structure, namely R1 risk in pancreaticoduodenectomy for pancreatic head carcinoma. Eur J Surg Oncol. 2013;39(12):1303–8.
Paiella S, Sandini M, Gianotti L, Butturini G, Salvia R, Bassi C. The prognostic impact of para-aortic lymph node metastasis in pancreatic cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2016;42(5):616–24.
Doussot A, Bouvier A, Santucci N, et al. Pancreatic ductal adenocarcinoma and paraaortic lymph nodes metastases: the accuracy of intraoperative frozen section. Pancreatology. 2019;19(5):710–5.
Asaoka T, Miyamoto A, Maeda S, et al. CA19-9 level determines therapeutic modality in pancreatic cancer patients with para-aortic lymph node metastasis. Hepatobiliary Pancreat Dis Int. 2018;17(1):75–80.
Liu C, Lu Y, Luo G, et al. Which patients with para-aortic lymph node (LN16) metastasis will truly benefit from curative pancreaticoduodenectomy for pancreatic head cancer? Oncotarget. 2016;7(20):29177–86.
Liu C, Chen R, Chen Y, et al. Should a standard lymphadenectomy during pancreatoduodenectomy exclude para-aortic lymph nodes for all cases of resectable pancreatic head cancer? A consensus statement by the chinese study group for pancreatic cancer (CSPAC). Int J Oncol. 2015;47(4):1512–6.
Motoi F, Kosuge T, Ueno H, et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol. 2019;49(2):190–4.
Versteijne E, van Dam JL, Suker M, et al. Neoadjuvant chemoradiotherapy versus upfront surgery for resectable and borderline resectable pancreatic cancer: long-term results of the Dutch randomized PREOPANC trial. J Clin Oncol. 2022;40(11):1220–30.
van Dam JL, Janssen QP, Besselink MG, et al. Neoadjuvant therapy or upfront surgery for resectable and borderline resectable pancreatic cancer: a meta-analysis of randomised controlled trials. Eur J Cancer. 2022;160:140–9.
Funding
The Medical Engineering Cross Research Fund of Shanghai Jiao Tong University, YG2021QN16, Shanghai Anti-Cancer Association, SACA-CY20C02
Author information
Authors and Affiliations
Contributions
Z.S., H. C., W. W., and B. S.: study conception, design. Z. S., H. C., S.Z., Y. J., Y. W., Y. Z., J. Z., X. D., C. P., and B. S.: acquisition of data. Z. S. and H. C.: analysis and interpretation of data. Z. S. and H. C.: drafting of the manuscript. Z. S., H. C., W. W., and B. S.: critical revision. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Disclosure
We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work, there is no professional or other personal interest of any nature or kind in any product, service and/or company that could be construed as influencing the position presented in, or the review of, the manuscript entitled, “The Impact of Additional Para-aortic Dissection during Pancreaticoduodenectomy for Resectable Pancreatic Cancer.”
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, Z., Chen, H., Zhao, S. et al. The Impact of Additional Para-aortic Dissection During Pancreaticoduodenectomy for Resectable Pancreatic Cancer. Ann Surg Oncol 30, 1474–1482 (2023). https://doi.org/10.1245/s10434-022-12700-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12700-z