Abstract
Background
The association between Medicaid expansion and postoperative mortality after surgery for gynecologic cancer is unknown. Our objective was to compare 30- and 90-day postoperative mortality after gynecologic cancer surgery before and after 2014 in states that did and did not expand Medicaid.
Methods
We searched the National Cancer Database for women aged 40–64 years old between 2010 and 2016 who underwent surgery for a primary gynecologic malignancy. We used pre/post and quasi-experimental difference-in-difference (DID) multivariable logistic regressions to evaluate mortality pre-2014 (2010–2013) and post-2014 (2014–2016) for states that did and did not expand Medicaid in January 2014. We completed univariable logistic regressions for covariates of interest.
Results
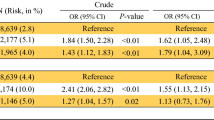
Among 169,731 women, 30-day postoperative mortality in expansion states after 2014 significantly decreased for endometrial cancer (odds ratio [OR] 0.42, 95% confidence interval [CI] 0.26–0.67) and ovarian cancer (OR 0.67, 95% CI 0.46–0.99) and increased for cervical cancer (OR 3.82, 95% CI 1.12–13.01). Compared with non-expansion states, expansion states had improved 30-day postoperative mortality for endometrial cancer after 2014 (DID OR 0.54, 95% CI 0.31–0.96). Univariable analysis demonstrated improved 30-day postoperative mortality for Black women with endometrial cancer in expansion states (DID OR 0.22, 95% CI 0.05–0.95). There was improved 90-day postoperative mortality for endometrial cancer in expansion states (OR 0.66, 95% CI 0.50–0.85), and improved 90-day postoperative mortality for Midwestern women with ovarian cancer in expansion states on univariable analysis (DID OR 0.48, 95% CI 0.26–0.91).
Conclusions
State Medicaid legislation was associated with improved postoperative survival in women with endometrial cancer and subgroups of women with endometrial and ovarian cancer.
Similar content being viewed by others
References
Grossman EGSC, Blount EC, Volberding EM. Compilation of Patient Protection and Affordable Care Act. Office of the Legislative Counsel; 2010.
Sommers BD, Maylone B, Blendon RJ, Orav EJ, Epstein AM. Three-year impacts of the affordable care act: improved medical care and health among low-income adults. Health Aff (Millwood). 2017;36(6):1119–28.
Wherry LR, Miller S. Early coverage, access, utilization, and health effects associated with the affordable care act medicaid expansions: a quasi-experimental study. Ann Intern Med. 2016;164(12):795–803.
Nathan NH, Bakhsheshian J, Ding L, Mack WJ, Attenello FJ. Evaluating medicaid expansion benefits for patients with cancer: national cancer database analysis and systematic review. J Cancer Policy. 2021;29:100292.
Barnes JM, Srivastava AJ, Gabani P, Perkins SM. Associations of early medicaid expansion with insurance status and stage at diagnosis among cancer patients receiving radiation therapy. Pract Radiat Oncol. 2020;10(4):e207–18.
Takvorian SU, Oganisian A, Mamtani R, et al. Association of medicaid expansion under the affordable care act with insurance status, cancer stage, and timely treatment among patients with breast, colon, and lung cancer. JAMA Netw Open. 2020;3(2):e1921653.
Lam MB, Phelan J, Orav EJ, Jha AK, Keating NL. Medicaid expansion and mortality among patients with breast, lung, and colorectal cancer. JAMA Netw Open. 2020;3(11):e2024366.
Barnes JM, Johnson KJ, Boakye EA, et al. Early medicaid expansion and cancer mortality. J Natl Cancer Inst. 2021;113(12):1714–22.
Charles EJ, Johnston LE, Herbert MA, et al. Impact of medicaid expansion on cardiac surgery volume and outcomes. Ann Thorac Surg. 2017;104(4):1251–8.
Dakour-Aridi H, Malas MB, Farber A, Avgerinos ED, Eslami MH. Association of medicaid expansion with in-hospital outcomes after abdominal aortic aneurysm repair. J Surg Res. 2021;266:201–12.
Eguia E, Baker MS, Chand B, Sweigert PJ, Kuo PC. The impact of the affordable care act (ACA) medicaid expansion on access to minimally invasive surgical care. Am J Surg. 2020;219(1):15–20.
Eslami MH, Dakour-Aridi H, Avgerinos ED, Makaroun MS, Malas MB. Impact of medicaid expansion of the affordable care on the outcomes of lower extremity bypass for patients with peripheral artery disease in the vascular quality initiative database. Ann Surg. 2019;270(4):647–55.
Brooks ES, Tong J, Mavroudis CW, et al. The effects of the affordable care act on access and outcomes of colon surgery. Am J Surg. 2021;222(3):613–8.
Eguia E, Baker MS, Bechara C, Shames M, Kuo PC. The impact of the affordable care act medicaid expansion on vascular surgery. Ann Vasc Surg. 2020;66:454-461.e451.
Loehrer AP, Song Z, Haynes AB, Chang DC, Hutter MM, Mullen JT. Impact of health insurance expansion on the treatment of colorectal cancer. J Clin Oncol. 2016;34(34):4110–5.
Eguia E, Cobb AN, Kothari AN, et al. Impact of the affordable care act (ACA) medicaid expansion on cancer admissions and surgeries. Ann Surg. 2018;268(4):584–90.
Mesquita-Neto JWB, Cmorej P, Mouzaihem H, Weaver D, Kim S, Macedo FI. Disparities in access to cancer surgery after Medicaid expansion. Am J Surg. 2020;219(1):181–4.
Diaz A, Chavarin D, Paredes AZ, Pawlik TM. Utilization of high-volume hospitals for high-risk cancer surgery in california following medicaid expansion. J Gastrointest Surg. 2021;25(7):1875–84.
Albright BB, Nasioudis D, Craig S, et al. Impact of medicaid expansion on women with gynecologic cancer: a difference-in-difference analysis. Am J Obstet Gynecol. 2020;224(2):195.e1-195.e17.
Sia TY, Wen T, Cham S, Friedman AM, Wright JD. Effect of frailty on postoperative readmissions and cost of care for ovarian cancer. Gynecol Oncol. 2020;159(2):426–33.
Sia TY, Wen T, Cham S, Friedman AM, Wright JD. The effect of frailty on postoperative readmissions, morbidity, and mortality in endometrial cancer surgery. Gynecol Oncol. 2021;161(2):353–60.
Mahdi H, Wiechert A, Lockhart D, Rose PG. Impact of age on 30-day mortality and morbidity in patients undergoing surgery for ovarian cancer. Int J Gynecol Cancer. 2015;25(7):1216–23.
Lindemann K, Kok PS, Stockler M, Jaaback K, Brand A. Enhanced recovery after surgery for advanced ovarian cancer: a systematic review of interventions trialed. Int J Gynecol Cancer. 2017;27(6):1274–82.
Hertlein L, Kirschenhofer A, Fürst S, et al. Malnutrition and clinical outcome in gynecologic patients. Eur J Obstet Gynecol Reprod Biol. 2014;174:137–40.
Melamed A, Bercow AS, Bunnell K, et al. Age-associated risk of 90-day postoperative mortality after cytoreductive surgery for advanced ovarian cancer. JAMA Surg. 2019;154(7):669–71.
Günakan E, Tohma YA, Tunç M, Akıllı H, Şahin H, Ayhan A. Factors associated with surgical morbidity of primary debulking in epithelial ovarian cancer. Obstet Gynecol Sci. 2020;63(1):64–71.
Boffa DJ, Rosen JE, Mallin K, et al. Using the national cancer database for outcomes research: a review. JAMA Oncol. 2017;3(12):1722–8.
National Cancer Database. Chicago, IL: American College of Surgeons; 2021.
Moss HA, Melamed A, Wright JD. Measuring cause-and-effect relationships without randomized clinical trials: Quasi-experimental methods for gynecologic oncology research. Gynecol Oncol. 2019;152(3):533–9.
Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401–2.
Fecho K, Lunney AT, Boysen PG, Rock P, Norfleet EA. Postoperative mortality after inpatient surgery: incidence and risk factors. Ther Clin Risk Manag. 2008;4(4):681–8.
Lee G, Dee EC, Orav EJ, et al. Association of medicaid expansion and insurance status, cancer stage, treatment and mortality among patients with cervical cancer. Cancer Rep (Hoboken). 2021;4(6):e1407.
Barrington DA, Sinnott JA, Calo C, Cohn DE, Cosgrove CM, Felix AS. Where you live matters: a National Cancer Database study of Medicaid expansion and endometrial cancer outcomes. Gynecol Oncol. 2020;158(2):407–14.
Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013;31(20):2607–18.
Mahdi H, Jernigan AM, Aljebori Q, Lockhart D, Moslemi-Kebria M. The impact of obesity on the 30-day morbidity and mortality after surgery for endometrial cancer. J Minim Invasive Gynecol. 2015;22(1):94–102.
Rauh-Hain JA, Rodriguez N, Growdon WB, et al. Primary debulking surgery versus neoadjuvant chemotherapy in stage IV ovarian cancer. Ann Surg Oncol. 2012;19(3):959–65.
Fagotti A, Ferrandina MG, Vizzielli G, et al. Randomized trial of primary debulking surgery versus neoadjuvant chemotherapy for advanced epithelial ovarian cancer (SCORPION-NCT01461850). Int J Gynecol Cancer. 2020;30(11):1657–64.
Pollack LM, Ekwueme DU, Hung MC, Miller JW, Chang SH. Estimating the impact of increasing cervical cancer screening in the National Breast and Cervical Cancer Early Detection Program among low-income women in the USA. Cancer Causes Control. 2020;31(7):691–702.
Miller JW, Plescia M, Ekwueme DU. Public health national approach to reducing breast and cervical cancer disparities. Cancer. 2014;120(Suppl16):2537–9.
Smith AJB, Fader AN. Association of the affordable care act with ovarian cancer care. Obstet Gynecol. 2020;135(2):257–65.
Temkin SM, Rimel BJ, Bruegl AS, Gunderson CC, Beavis AL, Doll KM. A contemporary framework of health equity applied to gynecologic cancer care: a Society of Gynecologic Oncology evidenced-based review. Gynecol Oncol. 2018;149(1):70–7.
Yang DX, Khera R, Miccio JA, et al. Prevalence of missing data in the national cancer database and association with overall survival. JAMA Netw Open. 2021;4(3):e211793.
SEER cancer stat facts: ovarian cancer. 2020. Available at: https://seer.cancer.gov/statfacts/html/ovary.html.
Acknowledgment
This work was supported in part by the National Institutes of Health. This work was supported in part by an MD Anderson Cancer Center Support Grant from the National Cancer Institute of the National Institutes of Health (NIH/NCI P30 CA016672, CA217685) and the T32 training grant CA101642. The NCDB is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC’s NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Funding
This work was supported in part by the National Institutes of Health and an MD Anderson Cancer Center Support Grant from the National Cancer Institute of the National Institutes of Health (NIH/NCI P30 CA016672, CA217685), as well as the T32 training Grant No. CA101642. LAM is supported by an NIH-NCIK07-CA201013 Grant No.; SHG is supported by CPRIT RP160674 and Komen SAC150061; and KMP is supported by CPRIT RP 170259.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Larissa A. Meyer reports consulting fees from Bristol Meyers Squibb, advisory board participation for GlaxoSmithKline, and stocks in Crisper, Invitae, and Bristol-Myers Squibb. Charlotte C. Sun reports partial research funding from AstraZeneca and stock in Inform Genomics. Sarah P. Huepenbecker, Shuangshuang Fu, Hui Zhao, Kristin M. Primm, and Sharon H. Giordano report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10434_2022_12663_MOESM1_ESM.docx
Supplementary 1 Database population selection. Supplementary 2 Parallel trends test for difference-in-difference baseline trend assumption – visual assessment of time plots in the pre-2014 study period. Supplementary 3 Parallel trends test for difference-in-difference baseline trend assumption – Cox regression model examining hazard ratios for expansion status, pre-2014 period, and the interaction term between expansion status and pre-2014 period: 30-day postoperative mortality. Supplementary 4 Parallel trends test for difference-in-difference baseline trend assumption – Cox regression model examining hazard ratios for expansion status, pre-2014 period, and the interaction term between expansion status and pre-2014 period: 90-day postoperative mortality (DOCX 39 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huepenbecker, S.P., Fu, S., Sun, C.C. et al. Medicaid Expansion and Postoperative Mortality in Women with Gynecologic Cancer: A Difference-in-Difference Analysis. Ann Surg Oncol 30, 1508–1519 (2023). https://doi.org/10.1245/s10434-022-12663-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12663-1