Abstract
Background
In older adults, skeletal muscle mass is an important factor for health and prognosis. The loss of SMM during neoadjuvant therapy affects the prognosis of patients with locally advanced esophageal cancer. However, information is limited regarding this possibility in older patients. This study aimed to establish the prognostic impact of SMM loss during neoadjuvant chemotherapy on older patients with locally advanced esophageal cancer.
Methods
This was a single-center retrospective cohort study. Patients age 65 years or older had undergone R0 curative esophagectomy after NAC. The skeletal muscle mass index before and after NAC was calculated from computed tomography images. The percentage change in the SMI during NAC (SMI%) was calculated from the SMI before and after NAC.
Results
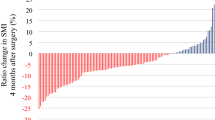
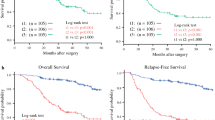
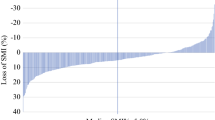
The study analyzed 150 patients with a mean age of 71.1 ± 3.7 years. The mean value of the SMI was 42.7 ± 7.2 cm2/m2 before NAC, and the SMI% was − 6.4% ± 5.9%. The cutoff of SMI% for overall survival was defined by the log-rank test as − 12%. The Cox proportional hazard model showed that major loss of the SMI (≥ 12%) significantly influenced OS (hazard ratio, 2.490; 95% confidence interval, 1.121–5.529; p = 0.025) independently of age, sex, pathologic T and N factors, or treatment regimen.
Conclusions
Major SMI loss has an impact on OS after R0 curative esophagectomy for older patients with locally advanced esophageal cancer.




Similar content being viewed by others
References
Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12:681–92.
Ando N, Kato H, Igaki H, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19:68–74. https://doi.org/10.1245/s10434-011-2049-9.
Kamangar F, Nasrollahzadeh D, Safiri S, et al. The global, regional, and national burden of oesophageal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:582–97.
Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36(22):2326–47.
Wildiers H, Heeren P, Puts M, et al. International society of geriatric oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol. 2014;32(24):2595–603.
National Comprehensive Cancer Network. Older Adult Oncology (version 1.2022). OAO-1. Retrieved from 29 Mar 2022 at https://www.nccn.org/professionals/physician_gls/pdf/senior.pdf.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Fulop T, Larbi A, Witkowski JM, et al. Aging, frailty, and age-related diseases. Biogerontology. 2010;11(5):547–63.
Extermann M, Brain E, Canin B, et al. Priorities for the global advancement of care for older adults with cancer: an update of the International Society of Geriatric Oncology Priorities Initiative. Lancet Oncol. 2021;22:e29–36.
Williams GR, Dunne RF, Giri S, Shachar SS, Caan BJ. Sarcopenia in the older adult with cancer. J Clin Oncol. 2021;39(19):2068–78.
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636–46.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Series A Biol Sci Med Sci. 2001;56:M146–57.
Jang MK, Park C, Hong S, Li H, Rhee E, Doorenbos AZ. Skeletal muscle mass change during chemotherapy: a systematic review and meta-analysis. Anticancer Res. 2020;40:2409–18.
Kamitani N, Migita K, Matsumoto S, et al. Association of skeletal muscle loss with the long-term outcomes of esophageal cancer patients treated with neoadjuvant chemotherapy. Surg Today. 2019;49:1022–8.
Järvinen T, Ilonen I, Kauppi J, Salo J, Räsänen J. Loss of skeletal muscle mass during neoadjuvant treatments correlates with worse prognosis in esophageal cancer: a retrospective cohort study. World J Surg Oncol. 2018;16:1–9.
Yoon HG, Oh D, Ahn YC, et al. Prognostic impact of sarcopenia and skeletal muscle loss during neoadjuvant chemoradiotherapy in esophageal cancer. Cancers. 2020;12:925.
Yokota T, Kato K, Hamamoto Y, et al. A 3-year overall survival update from a phase 2 study of chemoselection with DCF and subsequent conversion surgery for locally advanced unresectable esophageal cancer. Ann Surg Oncol. 2020;27(2):460–7. https://doi.org/10.1245/s10434-019-07654-8.
Nakashima Y, Saeki H, Nakanishi R, et al. Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Ann Surg. 2018;267:1100–4.
Yamashita K, Watanabe M, Mine S, et al. The impact of the Charlson Comorbidity Index on the prognosis of esophageal cancer patients who underwent esophagectomy with curative intent. Surg Today. 2018;48:632–9.
Matsuda S, Kawakubo H, Okamura A, et al. Prognostic significance of stratification using pathological stage and response to neoadjuvant chemotherapy for esophageal squamous cell carcinoma. Ann Surg Oncol. 2021;2:8438–47. https://doi.org/10.1245/s10434-021-10221-9.
Huang Y, Feng JF, Liu JS, Chen QX. Prognostic role of serum C-reactive protein in esophageal cancer: a systematic review and meta-analysis. Therapeut Clin Risk Manage. 2015;11:89–94.
Yang X, Huang Y, Feng JF, Liu JS. Prognostic significance of neutrophil-to-lymphocyte ratio in esophageal cancer: a meta-analysis. OncoTargets Ther. 2015;8:789–94.
Bullock AF, Greenley SL, McKenzie GA, Paton LW, Johnson MJ. Relationship between markers of malnutrition and clinical outcomes in older adults with cancer: systematic review, narrative synthesis, and meta-analysis. Eur J Clin Nutr. 2020;74:1519–35.
Izaks GJ, Westendorp RG, Knook DL. The definition of anemia in older persons. JAMA. 1999;281:1714–7.
Katayama H, Kurokawa Y, Nakamura K, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
Prado CM, Lieffers JR, McCargar LJ, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9(7):629–35.
Stene GB, Helbostad JL, Amundsen T, et al. Changes in skeletal muscle mass during palliative chemotherapy in patients with advanced lung cancer. Acta Oncologica. 2015;54:340–8.
Reid KF, Pasha E, Doros G, et al. Longitudinal decline of lower extremity muscle power in healthy and mobility-limited older adults: influence of muscle mass, strength, composition, neuromuscular activation, and single fiber contractile properties. Eur J Appl Physiol. 2014;114:29–39.
Koster A, Ding J, Stenholm S, et al. Does the amount of fat mass predict age-related loss of lean mass, muscle strength, and muscle quality in older adults. J Gerontol Series A Biomed Sci Med Sci. 2011;66:888–95.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Makiura D, Ono R, Inoue J, et al. Impact of sarcopenia on unplanned readmission and survival after esophagectomy in patients with esophageal cancer. Ann Surg Oncol. 2018;25:456–64. https://doi.org/10.1245/s10434-021-10221-9.
Löfgren A, Åkesson O, Johansson J, Persson J. Hospital costs and health-related quality of life from complications after esophagectomy. Eur J Surg Oncol. 2021;47:1042–7.
Derogar M, Orsini N, Sadr-Azodi O, Lagergren P. Influence of major postoperative complications on health-related quality of life among long-term survivors of esophageal cancer surgery. J Clin Oncol. 2012;30:1615–9.
Kataoka K, Takeuchi H, Mizusawa J, et al. Prognostic impact of postoperative morbidity after esophagectomy for esophageal cancer: exploratory analysis of JCOG9907. Ann Surg. 2017;265:1152–7.
Hironaka S, Tsubosa Y, Mizusawa J, et al. Phase I/II trial of 2-weekly docetaxel combined with cisplatin plus fluorouracil in metastatic esophageal cancer (JCOG 0807). Cancer Sci. 2014;105:1189–95.
Takahashi H, Arimura Y, Yamashita K, et al. Phase I/II study of docetaxel/cisplatin/fluorouracil combination chemotherapy against metastatic esophageal squamous cell carcinoma. J Thorac Oncol. 2010;5:122–8.
Tamura S, Imano M, Takiuchi H, et al. Phase II study of docetaxel, cisplatin, and 5-fluorouracil (DCF) for metastatic esophageal cancer (OGSG 0403). Anticancer Res. 2012;32:1403–8.
Ando N, Iizuka T, Ide H, et al. Surgery plus chemotherapy compared with surgery alone for localized squamous cell carcinoma of the thoracic esophagus: a Japan Clinical Oncology Group Study–JCOG9204. J Clin Oncol. 2003;21(24):4592–6.
Liao CD, Chen HC, Huang SW, Liou TH. The role of muscle mass gain following protein supplementation plus exercise therapy in older adults with sarcopenia and frailty risks: a systematic review and meta-regression analysis of randomized trials. Nutrients. 2019;11:1713.
Katakami N, Uchino J, Yokoyama T, et al. Anamorelin (ONO-7643) for the treatment of patients with non-small cell lung cancer and cachexia: results from a randomized, double-blind, placebo-controlled, multicenter study of Japanese patients (ONO-7643-04). Cancer. 2018;124:606–16.
Maltoni M, Nanni O, Scarpi E, Rossi D, Serra P, Amadori D. High-dose progestins for the treatment of cancer anorexia–cachexia syndrome: a systematic review of randomized clinical trials. Ann Oncol. 2001;12:289–300.
Acknowledgment
The authors thank the members of the Departments of Rehabilitation Medicine, Esophageal Surgery, and Gastrointestinal Oncology for their support. This research would not have been possible without their cooperation. We thank Cathel Kerr, BSc, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harada, T., Tsuji, T., Ueno, J. et al. Prognostic Impact of the Loss of Skeletal Muscle Mass During Neoadjuvant Chemotherapy on Older Patients with Esophageal Cancer. Ann Surg Oncol 29, 8131–8139 (2022). https://doi.org/10.1245/s10434-022-12379-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12379-2