Abstract
Background
Optimal management of stage II/III gastric cancer requires multidisciplinary care, often necessitating treatment at more than one facility. We aimed to determine patterns of “fragmented” care and its impact on outcomes, including concordance with National Comprehensive Cancer Network (NCCN) guidelines and overall survival.
Methods
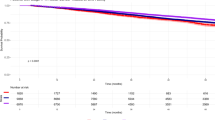
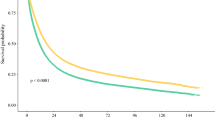
The 2006–2016 National Cancer Database was queried for patients with clinical stage II/III gastric adenocarcinoma who received preoperative therapy in addition to surgery. Patients were stratified based on whether surgery and chemotherapy/chemoradiation were performed at one versus multiple facilities (termed “coordinated” and “fragmented” care, respectively). Multivariable logistic regression was performed to identify factors associated with fragmented care. Survival was compared using Kaplan-Meier and Cox proportional hazards methods.
Results
Overall, 2033 patients met study criteria: 1043 (51.3%) received coordinated care and 990 (48.7%) fragmented care. There was no significant difference in time to surgery or pathologic upstaging by care structure. On adjusted analysis, factors associated with receipt of fragmented care included increasing age and distance traveled to the treating facility. Factors associated with coordinated care included metropolitan residence and treatment at academic and high-volume centers. Fragmented care was associated with a reduction in guideline-preferred perioperative chemotherapy (odds ratio [OR] 0.78, 95% confidence interval [CI] 0.63-0.97, p = 0.02) and increased mortality (HR 1.16, 95% CI 1.00-1.34, p = 0.05).
Conclusions
For patients with stage II/III gastric cancer, fragmented care is associated with inferior outcomes, including a reduction in preferred perioperative treatment and survival. Further work is needed to ensure equitable outcomes among patients as complex cancer care becomes more regionalized.



Similar content being viewed by others
References
Stitzenberg KB, Meropol NJ. Trends in centralization of cancer surgery. Ann Surg Oncol. 2010;17(11):2824–31. https://doi.org/10.1245/s10434-010-1159-0.
Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27(28):4671–8. https://doi.org/10.1200/jco.2008.20.1715.
Thiels CA, Hanson KT, Habermann EB, Boughey JC, Grotz TE. Integrated cancer networks improve compliance with national guidelines and outcomes for resectable gastric cancer. Cancer. 2020;126(6):1283–94. https://doi.org/10.1002/cncr.32660.
Hollenbeck BK, Miller DC, Wei JT, Montie JE. Regionalization of care: centralizing complex surgical procedures. Nat Clin Practice Urol. 2005;2(10):461–461. https://doi.org/10.1038/ncpuro0322.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37. https://doi.org/10.1056/NEJMsa012337.
Chhabra KR, Dimick JB. Hospital networks and value-based payment: fertile ground for regionalizing high-risk surgery. JAMA. 2015;314(13):1335–6. https://doi.org/10.1001/jama.2015.9803.
Tol JA, van Gulik TM, Busch OR, Gouma DJ. Centralization of highly complex low-volume procedures in upper gastrointestinal surgery. A summary of systematic reviews and meta-analyses. Dig Surg. 2012;29(5):374–83. https://doi.org/10.1159/000343929.
Mirza A, Pritchard S, Welch I. The postoperative component of MAGIC chemotherapy is associated with improved prognosis following surgical resection in gastric and gastrooesophageal junction adenocarcinomas. Int J Surg Oncol. 2013;2013:781742. https://doi.org/10.1155/2013/781742.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Gastric Cancer. website. https://www.nccn.org/professionals/physician_gls/pdf/gastric.pdf. Published 2021. Accessed 30 Dec 2021.
Al-Batran S-E, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393(10184):1948–57. https://doi.org/10.1016/S0140-6736(18)32557-1.
van Hagen P, Hulshof MCCM, van Lanschot JJB, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84. https://doi.org/10.1056/NEJMoa1112088.
Skolarus TA, Zhang Y, Hollenbeck BK. Understanding fragmentation of prostate cancer survivorship care: implications for cost and quality. Cancer. 2012;118(11):2837–45. https://doi.org/10.1002/cncr.26601.
Dreiher J, Comaneshter DS, Rosenbluth Y, Battat E, Bitterman H, Cohen AD. The association between continuity of care in the community and health outcomes: a population-based study. Isr J Health Policy Res. 2012;1(1):21. https://doi.org/10.1186/2045-4015-1-21.
Brauer DG, Wu N, Keller MR, et al. Care fragmentation and mortality in readmission after surgery for hepatopancreatobiliary and gastric cancer: a patient-level and hospital-level analysis of the healthcare cost and utilization project administrative database. J Am Coll Surg. 2021;232(6):921-32.e912. https://doi.org/10.1016/j.jamcollsurg.2021.03.017.
Brown ZJ, Labiner HE, Shen C, Ejaz A, Pawlik TM, Cloyd JM. Impact of care fragmentation on the outcomes of patients receiving neoadjuvant and adjuvant therapy for pancreatic adenocarcinoma. J Surg Oncol. n/a(n/a). https://doi.org/10.1002/jso.26706.
Cham S, Huang Y, Melamed A, et al. Fragmentation of surgery and chemotherapy in the initial phase of ovarian cancer care and its association with overall survival. Gynecol Oncol. 2021;162(1):56–64. https://doi.org/10.1016/j.ygyno.2021.04.032.
Freischlag K, Olivere L, Turner M, Adam M, Mantyh C, Migaly J. Does fragmentation of care in locally advanced rectal cancer increase patient mortality? J Gastrointest Surg. 2021;25(5):1287–96. https://doi.org/10.1007/s11605-020-04760-x.
Hester CA, Karbhari N, Rich NE, et al. Effect of fragmentation of cancer care on treatment use and survival in hepatocellular carcinoma. Cancer. 2019;125(19):3428–36. https://doi.org/10.1002/cncr.32336.
Doose M, Sanchez JI, Cantor JC, et al. Fragmentation of care among black women with breast cancer and comorbidities: the role of health systems. JCO Oncol Pract. 2021;17(5):e637–44. https://doi.org/10.1200/OP.20.01089.
Hussain T, Chang HY, Veenstra CM, Pollack CE. Fragmentation in specialist care and stage III colon cancer. Cancer. 2015;121(18):3316–24. https://doi.org/10.1002/cncr.29474.
Io Medicine. Delivering high-quality cancer care: charting a new course for a system in crisis. Washington: The National Academies Press; 2013.
Molina G, Qadan M. Addressing fragmentation of care requires strengthening of health systems and cross-institutional collaboration. Cancer. 2019;125(19):3296–8. https://doi.org/10.1002/cncr.32337.
Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20. https://doi.org/10.1056/NEJMoa055531.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683–90. https://doi.org/10.1245/s10434-007-9747-3.
Winchester DP, Stewart AK, Phillips JL, Ward EE. The National Cancer Data Base: past, present, and future. Ann Surg Oncol. 2010;17(1):4–7. https://doi.org/10.1245/s10434-009-0771-3.
Raval MV, Bilimoria KY, Stewart AK, Bentrem DJ, Ko CY. Using the NCDB for cancer care improvement: an introduction to available quality assessment tools. J Surg Oncol. 2009;99(8):488–90. https://doi.org/10.1002/jso.21173.
Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345(10):725–30. https://doi.org/10.1056/NEJMoa010187.
Acknowledgment
The American College of Surgeons is in a Business Associate Agreement that includes a data use agreement with each of its Commission on Cancer accredited hospitals. The data used in the study are derived from a deidentified National Cancer Data Base file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology used or the conclusions drawn from these data by the investigators. K. Rhodin, A. Eckhoff, and A. Liu are each supported by NIH 5T32CA093245-15 and acknowledge support from the Duke Cancer Institute as part of the P30 Cancer Center Support Grant (Grant ID: P30 CA014236).
Funding
K. Rhodin, A. Eckhoff, and A. Liu are each supported by NIH 5T32CA093245-15 and acknowledge support from the Duke Cancer Institute as part of the P30 Cancer Center Support Grant (Grant ID: P30 CA014236).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rhodin, K.E., Raman, V., Eckhoff, A. et al. Patterns and Impact of Fragmented Care in Stage II and III Gastric Cancer. Ann Surg Oncol 29, 5422–5431 (2022). https://doi.org/10.1245/s10434-022-12031-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12031-z