Abstract
Background
The incidence of hepatocellular carcinoma (HCC) has substantially increased over the last two decades within the Veteran Affairs Health System (VAHS). This study aims to describe the temporal trend of early-stage HCC (ES-HCC) treatment in the VAHS and identify patient/hospital factors associated with treatment disparities.
Patients and Methods
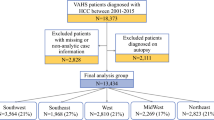
VA Corporate Data Warehouse was used to identify patients diagnosed with ES-HCC (stages I/II) from 2001 to 2015. Initial course of therapy was categorized as curative treatment (CT), noncurative treatment (NCT), or no treatment (NT). Univariate logistic regression and stepwise multivariate logistic regression models were used to analyze factors associated with receipt of treatment (CT/NCT) versus NT and receipt of CT versus NCT.
Results
Our study included 9504 patients (15% CT, 51% NCT, and 34% NT). During the study period, the rate of overall treatment increased, while the rate of CT decreased (p < 0.001). Stage II, age > 65 years, presence of non-alcoholic fatty liver disease (NAFLD), Child–Pugh C, higher Model for End-Stage Liver Disease (MELD) score, platelets < 100,000/mm3, low hospital complexity score, and Southwest location were significantly associated with higher rates of NT (all p < 0.05). Factors significantly associated with decreased utilization of CT included Hispanic race, lower hospital complexity score, and treatment in the Midwest, West, or Southeast regions (all p < 0.05).
Conclusions
There is a significant trend toward increased overall treatment utilization with decreased use of curative-intent approaches for ES-HCC in the national veteran population, and significant hospital and regional disparities exist. Further characterization and investigation of these factors may facilitate implementation of interventions to improve treatment utilization for the veteran population with HCC.




Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. 2018;394-424. https://doi.org/10.3322/caac.21492
Outcomes M. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level results from the global burden of disease study 2015. JAMA Oncol. 2017;98121(12):1683–91. https://doi.org/10.1001/jamaoncol.2017.3055.
Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001–2013. Gastroenterology. 2015;149(6):1471-1482.e5. https://doi.org/10.1053/j.gastro.2015.07.056.
Mittal S, El-Serag HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.e1. https://doi.org/10.1016/j.cgh.2015.07.019.
Mittal S, Sada YH, El-Serag HB, et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the veteran affairs population. Clin Gastroenterol Hepatol. 2015. https://doi.org/10.1016/j.cgh.2014.08.013.
Fisher ES, Welch HG. The future of the department of veterans affairs health care system. JAMA. 1995. https://doi.org/10.1001/jama.1995.03520320061042.
Serper M, Kaplan DE, Serper M, et al. Association of provider specialty and multidisciplinary care with hepatocellular carcinoma treatment and mortality. Gastroenterology. 2017. https://doi.org/10.1053/j.gastro.2017.02.040.
Huerta S, Pham T, Foster S, Livingston EH, Dineen S. Outcomes of emergent inguinal hernia repair in veteran octogenarians. Am Surg. 2014. https://doi.org/10.1177/000313481408000519.
Rodriguez Villalvazo Y, McDanel JS, Beste LA, Sanchez AJ, Vaughan-Sarrazin M, Katz DA. Effect of travel distance and rurality of residence on initial surveillance for hepatocellular carcinoma in VA primary care patient with cirrhosis. Health Serv Res. 2020. https://doi.org/10.1111/1475-6773.13241.
Davila JA, Kramer JR, Duan Z, et al. Referral and receipt of treatment for hepatocellular carcinoma in United States veterans: effect of patient and nonpatient factors. Hepatology. 2013;57(5):1858–68. https://doi.org/10.1002/hep.26287.
Zou WY, El-Serag HB, Sada YH, et al. Determinants and outcomes of hospice utilization among patients with advance-staged hepatocellular carcinoma in a Veteran affairs population. Dig Dis Sci. 2018. https://doi.org/10.1007/s10620-018-4989-4.
Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the veterans health administration. Health Aff. 2014. https://doi.org/10.1377/hlthaff.2014.0054.
Health Services Research and Development. Corporate Data Warehouse. US Department of Veterans Affairs.
Quan H, Fong A, Burnand B, Saunders LD, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005. https://doi.org/10.1016/j.aquaculture.2009.07.004.
Kaplan DE, Dai F, Aytaman A, et al. Development and performance of an algorithm to estimate the Child–Turcotte–Pugh score from a national electronic healthcare database. Clin Gastroenterol Hepatol. 2015;13(13):2333-2341.e6. https://doi.org/10.1016/j.cgh.2015.07.010.
Kamath PS, Kim WR. The model for end-stage liver disease (MELD). Hepatology. 2007;45(3):797–805. https://doi.org/10.1002/hep.21563.
Trombold J, Farmer RW, McCafferty M. The impact of colorectal cancer screening in a Veteran Hospital population. Am Surg. 2013. https://doi.org/10.1177/000313481307900330.
N. T, P. R, D.L. W, et al. Evaluating screening approaches for hepatocellular carcinoma in a cohort of HCV related cirrhosis patients from the Veteran’s Affairs Health Care System. BMC Med Res Methodol. 2018. https://doi.org/10.1186/s12874-017-0458-6 LK - http://ucelinks.cdlib.org:8888/sfx_local?sid=&genre=&issn=&date=2018&volume=18&issue=1&spage=1&epage=&title=BMC+medical+research+methodology&atitle=Evaluating+screening+approaches+for+hepatocellular+carcinoma+in+a+cohort+of+HCV+related+cirrhosis+patients+from+the+Veteran%27s+Affairs+Health+Care+System&aulast=Tayob&aufirst=Nabihah&isbn=&id=DOI:10.1186%2Fs12874-017-0458-6&ABBR=&arnumber=&sid=EMBASE&issn=14712288&id=doi:10.1186%2Fs12874-017-0458-6&atitle=Evaluating+s
Tayob N, Christie I, Richardson P, et al. Validation of the hepatocellular carcinoma early detection screening (HES) algorithm in a cohort of veterans with cirrhosis. Clin Gastroenterol Hepatol. 2019. https://doi.org/10.1016/j.cgh.2018.12.005.
Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018. https://doi.org/10.1002/hep.29086.
Vitale A, Morales RR, Zanus G, et al. Barcelona clinic liver cancer staging and transplant survival benefit for patients with hepatocellular carcinoma: a multicentre, cohort study. Lancet Oncol. 2011. https://doi.org/10.1016/S1470-2045(11)70144-9.
Bruix J, Reig M, Sherman M. Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma. Gastroenterology. 2016. https://doi.org/10.1053/j.gastro.2015.12.041.
Shah SA, Smith JK, Li YF, Ng SC, Carroll JE, Tseng JF. Underutilization of therapy for hepatocellular carcinoma in the medicare population. Cancer. 2011;117(5):1019–26. https://doi.org/10.1002/cncr.25683.
Hoehn RS, Hanseman DJ, Jernigan PL, Wima K, Ertel AE, Abbott DE, Shah SA. Cincinnati research in outcomes and safety in surgery (CROSS). Disparities in care for patients with curable hepatocellular carcinoma. HPB (Oxford). 2015;17(9):747–52. https://doi.org/10.1111/hpb.12427.
Yopp AC, Mansour JC, Beg MS, et al. Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol. 2014. https://doi.org/10.1245/s10434-013-3413-8.
Chang TT, Sawhney R, Monto A, Davoren JBEN. Implementation of a multidisciplinary treatment team for hepatocellular cancer at a Veterans Affairs Medical Center improves survival. 2008. https://doi.org/10.1080/13651820802356572
Lau K, Salami A, Barden G, et al. The effect of a regional hepatopancreaticobiliary surgical program on clinical volume, quality of cancer care, and outcomes in the veterans affairs system. JAMA Surg. 2014. https://doi.org/10.1001/jamasurg.2014.1711.
Goldberg DS, Taddei TH, Serper M, et al. Identifying barriers to hepatocellular carcinoma surveillance in a national sample of patients with cirrhosis. Hepatology. 2017. https://doi.org/10.1002/hep.28765.
Singal AG, Yopp AS, Skinner C, Packer M, Lee WM, Tiro JA. Utilization of hepatocellular carcinoma surveillance among American patients: a systematic review. J Gen Intern Med. 2012. https://doi.org/10.1007/s11606-011-1952-x.
Hwa KJ, Dua MM, Wren SM, Visser BC. Missing the obvious: psychosocial obstacles in veterans with hepatocellular carcinoma. HPB. 2015. https://doi.org/10.1111/hpb.12508.
Shiina S, et al. Percutaneous ablation for hepatocellular carcinoma: comparison of various ablation techniques and surgery. Can J Gastroenterol Hepatol, 2018. 2018.
Putzer D, et al. Thermal ablation—an option in curative treatment of HCC. Memo Mag Eur Med Oncol. 2020;13(2):207–11.
Zhu F, Rhim H. Thermal ablation for hepatocellular carcinoma: what’s new in 2019. Chin Clin Oncol. 2019;8(6):58–58.
O’Leary C, Mahler M, Soulen MC. Curative-intent therapies in localized hepatocellular carcinoma. Curr Treat Options Oncol. 2020;21(4):1–14.
Funding
Dr. Polanco received financial support from the New Investigator Program of the Veterans Affairs North Texas Healthcare System for this project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception/design and preparation of the final manuscript. M.C. performed the statistical analysis.
Corresponding author
Ethics declarations
Disclosure
None of the authors has any conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Polanco, P.M., Ju, M.R., Chansard, M. et al. Trends and Disparities in Treatment Utilization for Early-Stage Hepatocellular Carcinoma in the Veteran Population. Ann Surg Oncol 29, 5488–5497 (2022). https://doi.org/10.1245/s10434-022-11897-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11897-3