Abstract
Background
The number of patients with esophageal cancer aged ≥ 70 years with a poor prognosis is increasing. In general patients with esophageal cancer, postoperative loss of skeletal muscle mass (SMM) is a prognostic factor. This study was designed to investigate the prognostic impact of postoperative loss of SMM in patients aged ≥ 70 years with esophageal cancer.
Methods
This study was a single-center, retrospective cohort study. Patients with esophageal cancer who underwent R0 esophagectomy between 2016 and 2020 were included. The percentage postoperative loss of skeletal muscle mass index (SMI%) was calculated using computed tomography images before and at 4 ± 2 months after surgery.
Results
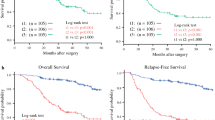
The number of subjects in the ≥ 70-year and < 70-year age groups was 166 and 218, respectively. The median SMI% was 5% in all patients; thus, 5% was defined as the cutoff point to define major loss of SMI. Major loss of SMI impacted 3-year overall survival (OS) in the ≥ 70-year age group, independent of age, sex, clinical stage, pathological T and N factors, Charlson comorbidity index, and length of hospital stay (adjusted hazard ratio [HR]: 4.400; 95% confidence interval: 1.202–16.105; P = 0.025). The adjusted HR of major loss of SMI in the ≥ 70-year age group was higher than in the < 70-year age group (adjusted HR: 4.400 vs. 2.388, respectively).
Conclusions
Postoperative loss of SMI in patients with esophageal cancer aged ≥ 70 years more strongly impacted 3-year OS than in patients aged < 70 years.



Similar content being viewed by others
References
Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive registry of esophageal cancer in Japan, 2009. Esophagus. 2016;13:110–37.
Poon RT, Law SY, Chu KM, Branicki FJ, Wong J. Esophagectomy for carcinoma of the esophagus in the elderly results of current surgical management. Ann Surg. 1998;227:357–64.
Cijs TM, Verhoef C, Steyerberg EW, et al. Outcome of esophagectomy for cancer in elderly patients. Ann Thorac Surg. 2010;90:900–7.
Tapias LF, Muniappan A, Wright CD, et al. Short and long-term outcomes after esophagectomy for cancer in elderly patients. Ann Thorac Surg. 2013;95:1741–8.
Kamangar F, Nasrollahzadeh D, Safiri S, et al. The global, regional, and national burden of oesophageal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(6):582–97.
Mohile SG, Dale W, Somerfield MR, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36:2326.
Wildiers H, Heeren P, Puts M, et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol. 2014;32:2595.
Extermann M, Brain E, Canin B, et al. Priorities for the global advancement of care for older adults with cancer an update of the International Society of Geriatric Oncology Priorities Initiative. Lancet Oncol. 2021;22:1005.
Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer. 2016;57:58–67.
Pamoukdjian F, Bouillet T, Lévy V, Soussan M, Zelek L, Paillaud E. Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: a systematic review. Clin Nutr. 2018;37:1101–13.
Kudou K, Saeki H, Nakashima Y, et al. Postoperative skeletal muscle loss predicts poor prognosis of adenocarcinoma of upper stomach and esophagogastric junction. World J Surg. 2019;43:1068–75.
Nakashima Y, Saeki H, Hu Q, et al. Skeletal muscle loss after esophagectomy is an independent risk factor for patients with esophageal cancer. Ann Surg Oncol. 2020;27:492–8.
Takahashi K, Watanabe M, Kozuki R, et al. Prognostic significance of skeletal muscle loss during early postoperative period in elderly patients with esophageal cancer. Ann Surg Oncol. 2019;26:3727–35.
Nakashima Y, Saeki H, Nakanishi R, et al. Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Ann Surg. 2018;267:1100–4.
Yang X, Huang Y, Feng JF, Liu JS. Prognostic significance of neutrophil-to-lymphocyte ratio in esophageal cancer: a meta-analysis. Oncol Targets Ther. 2015;8:789.
Huang Y, Feng JF, Liu JS, Chen QX. Prognostic role of serum C-reactive protein in esophageal cancer: a systematic review and meta-analysis. Ther Clin Risk Manag. 2015;11:89.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Katayama H, Kurokawa Y, Nakamura K, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Yamashita K, Watanabe M, Mine S, et al. The impact of the Charlson comorbidity index on the prognosis of esophageal cancer patients who underwent esophagectomy with curative intent. Surg Today. 2018;48:632–9.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
Eilers PH, Marx BD. Flexible smoothing with B-splines and penalties. Stat Sci. 1996;11:89–121.
Renfro LA, Loupakis F, Adams RA, et al. Body mass index is prognostic in metastatic colorectal cancer: pooled analysis of patients from first-line clinical trials in the ARCAD database. J Clin Oncol. 2016;34:144.
Fried Linda P, Tangen Catherine M, Walston Jeremy, et al. Frailty in older adults: evidence for a phenotype. J Gerontol. 2001;56(3):146–57.
Rockwood K, Stadnyk K, MacKnight C, McDowell I, Hébert R, Hogan DB. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353:205–6.
Campbell AJ, Buchner DM. Unstable disability and the fluctuations of frailty. Age Ageing. 1997;26:315–8.
Buchner DM, Edward H. Preventing frail health. Clin Geriatr Med. 1992;8:1–18.
Auyeung TW, Lee SWJ, Leung J, Kwok T, Woo J. Age-associated decline of muscle mass, grip strength and gait speed: a 4-year longitudinal study of 3018 community-dwelling older Chinese. Geriatr Gerontol Int. 2014;14:76–84.
Matthew JD, Tamara BH, Marjolein V, et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90:1579–85.
Dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB. Sarcopenia and physical independence in older adults: the independent and synergic role of muscle mass and muscle function. J Cachexia Sarcopenia Muscle. 2017;8:245–50.
da Silva Alexandre T, Duarte YDO, Santos JF, Wong R, Lebrão ML. Sarcopenia according to the European Working Group on sarcopenia in older people (EWGSOP) versus dynapenia as a risk factor for disability in the elderly. J Nutr Health Aging. 2014;18:547–53.
Nelke C, Dziewas R, Minnerup J, Meuth SG, Ruck T. Skeletal muscle as potential central link between sarcopenia and immune senescence. EBioMedicine. 2019;49:381–8.
Afzali AM, Müntefering T, Wiendl H, Meuth SG, Ruck T. Skeletal muscle cells actively shape (auto) immune responses. Autoimmun Rev. 2018;17:518–29.
Feng X, Todd T, Lintzenich CR, et al. Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol. 2013;68:853–60.
Wakabayashi H, Matsushima M, Uwano R, Watanabe N, Oritsu H, Shimizu Y. Skeletal muscle mass is associated with severe dysphagia in cancer patients. J Cachexia Sarcopenia Muscle. 2015;6:351–7.
Couderc AL, Boulahssass R, Nouguerède E, et al. Functional status in a geriatric oncology setting: a review. J Geriatr Oncol. 2019;10:884–94.
Bruijnen CP, van Harten-Krouwel DG, Koldenhof JJ, Emmelot-Vonk MH, Witteveen PO. Predictive value of each geriatric assessment domain for older patients with cancer: a systematic review. J Geriatr Oncol. 2019;10:859–73.
Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95.
Jang MK, Park C, Hong S, Li H, Rhee E, Doorenbos AZ. Skeletal muscle mass change during chemotherapy: a systematic review and meta-analysis. Anticancer Res. 2020;40:2409–18.
Liao CD, Chen HC, Huang SW, Liou TH. The role of muscle mass gain following protein supplementation plus exercise therapy in older adults with sarcopenia and frailty risks: a systematic review and meta-regression analysis of randomized trials. Nutrients. 2019;11:1713.
Acknowledgments
The authors thank the members of the Department of Rehabilitation Medicine, Esophageal Surgery, for their support; this research would not have been possible without their cooperation. They also thank Emily Woodhouse, PhD, and Georgia Lenihan-Geels, PhD, from Edanz (https://jp.edanz.com/ac), for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no potential conflicts of interest with regard to the research, authorship, or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harada, T., Tatematsu, N., Ueno, J. et al. Prognostic Impact of Postoperative Loss of Skeletal Muscle Mass in Patients Aged 70 Years or Older with Esophageal Cancer. Ann Surg Oncol 29, 5638–5645 (2022). https://doi.org/10.1245/s10434-022-11801-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11801-z