Abstract
Background
Women ≥ 65 years of age are less likely to receive guideline-concordant breast cancer care. Given existing racial/ethnic disparities, older minority breast cancer patients may be especially prone to inequalities in care. How site of care impacts older breast cancer patients is not well defined. We sought to evaluate the association between race/ethnicity and breast cancer treatment delays in older women treated at minority-serving hospitals (MSHs) versus non-MSHs.
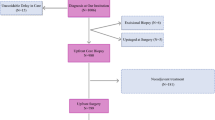
Methods
Women ≥ 65 years of age treated for non-metastatic breast cancer were identified in the National Cancer Database (2010–2017). Treatment delay was defined as > 90 days from diagnosis to initial treatment. MSHs were defined as the top decile of hospitals serving predominantly Black or Hispanic patients. Multivariable logistic regression models adjusted for patient, tumor, and hospital characteristics were used to determine the odds of treatment delay for women at MSHs versus non-MSHs across racial/ethnic groups.
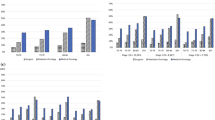
Results
Overall, 557,816 women were identified among 41 MSHs and 1146 non-MSHs. Average time to treatment was 33.71 days (standard deviation 26.92 days). Older women at MSHs were more likely to experience treatment delays than those at non-MSHs (odds ratio 1.28, 95% confidence interval 1.21–1.36). Regardless of where they received care, minorities were more likely to experience treatment delays than non-Hispanic White women.
Conclusions
Although 97% of older women treated at Commission on Cancer-accredited hospitals received timely breast cancer care, minorities and those treated at MSHs were more likely to experience treatment delays. Interventions addressing barriers to timely breast cancer care at MSHs may be an effective approach to reducing racial/ethnic disparities.



Similar content being viewed by others
References
DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–51. https://doi.org/10.3322/caac.21583.
Smith BD, Jiang J, McLaughlin SS, et al. Improvement in breast cancer outcomes over time: are older women missing out? J Clin Oncol. 2011;29:4647–53. https://doi.org/10.1200/JCO.2011.35.8408.
Freedman RA, Keating NL, Lin NU, et al. Breast cancer-specific survival by age: Worse outcomes for the oldest patients. Cancer. 2018;124(10):2184–91. https://doi.org/10.1002/cncr.31308.
Wheeler SB, Reeder-Hayes KE, Carey LA. Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist. 2013;18(9):986–93. https://doi.org/10.1634/theoncologist.2013-0243.
Yedjou CG, Sims JN, Miele L, et al. Health and racial disparity in breast cancer. Adv Exp Med Biol. 2019;1152:31–49. https://doi.org/10.1007/978-3-030-20301-6_3.
Jemal A, Robbins AS, Lin CC, et al. Factors that contributed to black-white disparities in survival among nonelderly women with breast cancer between 2004 and 2013. J Clin Oncol. 2018;36:14–24. https://doi.org/10.1220/JCO.2017.73.7932.
Kantor O, Wang ML, Bertrand K, Pierce L, Freedman RA, Chavez-MacGregor M, King TA, Mittendorf EA. Racial and socioeconomic disparities in breast cancer outcomes within the AJCC pathologic prognostic staging system. Ann Surg Oncol. 2022;29(1):686–96. https://doi.org/10.1245/s10434-021-10527-8.
Krimphove MJ, Fletcher SA, Cole AP, et al. Quality of care in the treatment of localized intermediate and high risk prostate cancer at minority serving hospitals. J Urol. 2019;201(4):735–41. https://doi.org/10.1016/j.juro.2018.10.024.
Cole AP, Nguyen D-D, Meirkhanov A, et al. Association of care at minority-serving vs non–minority-serving hospitals with use of palliative care among racial/ethnic minorities with metastatic cancer in the United States. JAMA Netw Open. 2019;2(2):e187633. https://doi.org/10.1001/jamanetworkopen.2018.7633.
Joynt KE, Orav EJ, Jha AK. Patient race, site of care, and 30-day readmission rates among elderly Americans. JAMA. 2011;305(7):675–81. https://doi.org/10.1001/jama.2011.123.
Danziger J, de la Hoz MÁA, Li W, et al. Temporal trends in critical care outcomes in U.S. Minority-serving hospitals. Am J Respir Crit Care Med. 2020;201(6):681–7. https://doi.org/10.1164/rccm.201903-0623OC.
Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–82. https://doi.org/10.1001/archinte.167.11.1177.
Fletcher SA, Gild P, Cole AP, et al. The effect of treatment at minority-serving hospitals on outcomes for bladder cancer. Urol Oncol. 2018;36(5):238.e7-238.e17. https://doi.org/10.1016/j.urolonc.2018.01.010.
Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014;211(6):647.e1-16. https://doi.org/10.1016/j.ajog.2014.06.006.
Gaskin DJ, Spencer CS, Richard P, Anderson G, Powe NR, LaVeist TA. Do minority patients use lower quality hospitals? Inquiry. 2011;48(3):209–20. https://doi.org/10.5034/inquiryjrnl_48.03.06.
Bleicher RJ, Ruth K, Sigurdson ER, et al. Time to surgery and breast cancer survival in the United States [published erratum appears in JAMA Oncol. 2016. Sep; 2(9):1244]. JAMA Oncol. 2016;2(3):330–9. https://doi.org/10.1001/jamaoncol.2015.4508.
Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH. Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol. 2016;2(3):322–9. https://doi.org/10.1001/jamaoncol.2015.3856.
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI. Delay of adjuvant chemotherapy initiation following breast cancer surgery among elderly women. Breast Cancer Res Treat. 2006;99(3):313–21. https://doi.org/10.1007/s10549-006-9206-z.
de Melo Gagliato D, Lei X, Giordano SH, et al. Impact of delayed neoadjuvant systemic chemotherapy on overall survival among patients with breast cancer. Oncologist. 2020;25(9):749–57. https://doi.org/10.1634/theoncologist.2019-0744.
National College of Surgeons. 2021. Available at: https://www.facs.org/quality-programs/cancer/ncdb. Accessed 8 Sep 2021.
Facility Oncology Registry Data Standards (FORDS). 2016. Available at: https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/fords-2016.ashx. Accessed 21 Dec 2021.
Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med. 2006;166(20):2244–52. https://doi.org/10.1001/archinte.166.20.2244.
Polverini AC, Nelson RA, Marcinkowski E, et al. Time to treatment: measuring quality breast cancer care. Ann Surg Oncol. 2016;23(10):3392–402. https://doi.org/10.1245/s10434-016-5486-7.
Navarro S, Yang Y, Ochoa C, et al. Breast cancer surgical delays in a racially and ethnically diverse California cancer registry cohort. J Clin Oncol. 2021;39(15 Suppl):e12589. https://doi.org/10.1200/JCO.2021.39.15_suppl.e12589.
Champion CD, Thomas SM, Plichta JK, et al. Disparities at the intersection of race and ethnicity: examining trends and outcomes in Hispanic women with breast cancer. JCO Oncol Pract. 2020. https://doi.org/10.1200/OP.20.00381.
Adams SV, Bansal A, Burnett-Hartman AN, et al. Cancer treatment delays in American Indians and Alaska natives enrolled in medicare. J Health Care Poor Underserved. 2017;28(1):350–61. https://doi.org/10.1353/hpu.2017.0027.
Wilson RT, Adams-Cameron M, Burhansstipanov L, et al. Disparities in breast cancer treatment among American Indian, Hispanic and non-Hispanic white women enrolled in medicare. J Health Care Poor Underserved. 2007;18(3):648–64. https://doi.org/10.1353/hpu.2007.0071.
Jacobson JS, Grann VR, Hershman D, Troxel AB, Li H, Neugut AI. Breast biopsy and race/ethnicity among women without breast cancer. Cancer Detect Prev. 2006;30(2):129–33. https://doi.org/10.1016/j.cdp.2006.02.002.
Chagpar AB, Dupont E, Chiba A, et al; SHAVE2 authors. Are we choosing wisely? Drivers of preoperative MRI use in breast cancer patients. Am J Surg. 2021. https://doi.org/10.1016/j.amjsurg.2021.10.028
Butler PD, Familusi O, Serletti JM, et al. Influence of race, insurance status, and geographic access to plastic surgeons on immediate breast reconstruction rates. Am J Surg. 2018;215(6):987–94. https://doi.org/10.1016/j.amjsurg.2017.09.037.
Chapman-Davis E, Zhou ZN, Fields JC, et al. Racial and ethnic disparities in genetic testing at a hereditary breast and ovarian cancer center. J Gen Intern Med. 2021;36(1):35–42. https://doi.org/10.1007/s11606-020-06064-x.
Santosa KB, Qi J, Kim HM, et al. Effect of patient age on outcomes in breast reconstruction: results from a multicenter prospective study. J Am Coll Surg. 2016;223(6):745–54. https://doi.org/10.1016/j.jamcollsurg.2016.09.003.
Boddicker NJ, Hu C, Weitzel JN, et al. Risk of late-onset breast cancer in genetically predisposed women. J Clin Oncol. 2021;39(31):3430–40. https://doi.org/10.1200/JCO.21.00531.
Thompson CA, Gomez SL, Hastings KG, et al. The burden of cancer in Asian Americans: a report of national mortality trends by Asian ethnicity. Cancer Epidemiol Biomark Prev. 2016;25(10):1371–82. https://doi.org/10.1158/1055-9965.EPI-16-0167.
Trinh QD, Nguyen PL, Leow JJ, et al. Cancer-specific mortality of Asian Americans diagnosed with cancer: a nationwide population-based assessment. J Natl Cancer Inst. 2015;107(6):djv054. https://doi.org/10.1093/jnci/djv054.
Zamora SM, Pinheiro PS, Gomez SL, et al. Disaggregating Hispanic American cancer mortality burden by detailed ethnicity. Cancer Epidemiol Biomark Prev. 2019;28(8):1353. https://doi.org/10.1158/1055-9965.EPI-18-0872.
National Quality Measures for Breast Centers. 2021. Available at: https://www.nqmbc.org/quality-measure-program/quality-measures.cms. Accessed 8 Sep 2021.
Commission on Cancer. 2019. Available at: https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/quality-measures.ashx. Accessed 22 Sep 2021.
Mohanty S, Bilimoria KY. Comparing national cancer registries: the national cancer data base (NCDB) and the surveillance, epidemiology, and end results (SEER) program. J Surg Oncol. 2014;109(7):629–30. https://doi.org/10.1002/jso.23568.
Acknowledgments
The authors would like to thank Rachel Freedman, MD, MPH, for her advice and support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Tari A. King is a speaker and advisory board member for Exact Sciences, formerly Genomic Health, and has served as a faculty member of PrecisCA cancer information service. Elizabeth A. Mittendorf has no relevant disclosures for this work but reports compensated service on scientific advisory boards for AstraZeneca, Exact Sciences, Merck, Roche/Genentech; uncompensated service on steering committees for Bristol Myers Squibb, Lilly, and Roche/Genentech; and institutional research support from Roche/Genentech (via SU2C grant) and Gilead. Julia H. Song, Olga Kantor, and Christina A. Minami have no disclosures to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Song, J.H., Kantor, O., Mittendorf, E.A. et al. Race and Site of Care Impact Treatment Delays in Older Women with Non-Metastatic Breast Cancer. Ann Surg Oncol 29, 4103–4114 (2022). https://doi.org/10.1245/s10434-022-11543-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11543-y