Abstract
Background
Cancer-related fatigue (CRF) is the most distressing symptom in the overall cancer population. For patients with esophageal cancer, CRF may even be harder to predict and control due to its complicated and prolonged treatment. Moreover, communication difficulties due to disease progression or treatment may further diminish esophageal cancer patients’ ability to communicate about CRF. However, little research has addressed the trajectory and associating factors of CRF in this population, especially during the active treatment phase. The purpose of this study was (1) to evaluate and compare the level of CRF at three time points, namely before treatment, a month after concurrent chemoradiotherapy (CCRT), and a week after surgery, and (2) to identify associated factors of CRF.
Methods
This prospective cohort study used a questionnaire to evaluate esophageal cancer patients’ CRF at three time points. Repeated measures ANOVA and linear regression were used to analyze the data.
Results
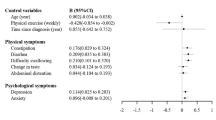
This study included 73 participants. The severity of all CRF aspects intensified significantly over the course of treatment, reaching the highest level after surgery (P < 0.001). Worries of physician invalidation at baseline (P < 0.05) and marital status associated with CRF after CCRT and after surgery.
Conclusions
This is the first study to demonstrate the relationship between CRF and physician invalidation. Clinicians must be aware of the intensifying trend of CRF and provide timely intervention when caring for patients with esophageal cancer during cancer treatment. Reducing the worries of physician invalidation may alleviate CRF.


Similar content being viewed by others
References
Cella D, Peterman A, Passik S, Jacobsen P, Breitbart W. Progress toward guidelines for the management of fatigue. Oncology (Williston Park, NY). 1998;12(11A):369–77.
Corbett T, Walsh JC, Groarke A, Moss-Morris R, Morrissey E, McGuire BE. Cancer-related fatigue in post-treatment cancer survivors: theory-based development of a web-based intervention. JMIR Cancer. 2017;3(2):e6987.
Jean-Pierre P, Figueroa-Moseley CD, Kohli S, Fiscella K, Palesh OG, Morrow GR. Assessment of cancer-related fatigue: implications for clinical diagnosis and treatment. Oncologist. 2007;12:11–21.
Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;12:4–10.
Lai S-C, Lin W-C, Chen C-H, Wu S-Y. Development of a Taiwan cancer-related fatigue cognition questionnaire: reliability and validity. Oncotarget. 2017;8(17):28880.
Stobäus N, Müller MJ, Küpferling S, Schulzke J-D, Norman K. Low recent protein intake predicts cancer-related fatigue and increased mortality in patients with advanced tumor disease undergoing chemotherapy. Nutr Cancer. 2015;67(5):818–24.
Kreissl S, Mueller H, Goergen H, et al. Cancer-related fatigue in patients with and survivors of Hodgkin’s lymphoma: a longitudinal study of the German Hodgkin Study Group. Lancet Oncol. 2016;17(10):1453–62.
Susanne K, Michael F, Thomas S, Peter E, Andreas H. Predictors of fatigue in cancer patients: a longitudinal study. Support Care Cancer. 2019;27(9):3463–71.
Inglis JE, Kleckner AS, Lin P-J, et al. Excess body weight and cancer-related fatigue, systemic inflammation, and serum lipids in breast cancer survivors. Nutr Cancer. 2020;6:1–11.
Hwang SS, Chang VT, Rue M, Kasimis B. Multidimensional independent predictors of cancer-related fatigue. J Pain Sympt Management. 2003;26(1):604–14.
Van Der Weijst L, Surmont V, Schrauwen W, Lievens Y. Predictors for cancer-related fatigue among patients with advanced lung cancer attending palliative care department: a prospective observational study.
Inglis JE, Lin P-J, Kerns SL, et al. Nutritional interventions for treating cancer-related fatigue: a qualitative review. Nutr Cancer. 2019;71(1):21–40.
Prip A, Møller KA, Nielsen DL, Jarden M, Olsen M-H, Danielsen AK. The patient–healthcare professional relationship and communication in the oncology outpatient setting: a systematic review. Cancer Nurs. 2018;41(5):E11.
Greville-Harris M, Dieppe P. Bad is more powerful than good: the nocebo response in medical consultations. Am J Med. 2015;128(2):126–9.
Edlund SM, Wurm M, Holländare F, Linton SJ, Fruzzetti AE, Tillfors M. Pain patients’ experiences of validation and invalidation from physicians before and after multimodal pain rehabilitation: associations with pain, negative affectivity, and treatment outcome. Scand J Pain. 2017;17(1):77–86.
Stauder M, Romero Y, Kabat B, et al. Overall survival and self-reported fatigue in patients with esophageal cancer. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. 2013;21(2):511–9.
Qureshi HA, Abouyared M, Barber B, Houlton JJ. Surgical options for locally advanced oropharyngeal cancer. Curr Treat Options Oncol. 2019;20(5):1–11.
Han-Markey TL. Examination of the association of diet and persistent cancer-related fatigue: a pilot study. Paper presented at: Oncology nursing forum 2013.
Miller M, Maguire R, Kearney N. Patterns of fatigue during a course of chemotherapy: results from a multi-centre study. Eur J Oncol Nurs. 2007;11(2):126–32.
Berger AM, Lockhart K, Agrawal S. Variability of patterns of fatigue and quality of life over time based on different breast cancer adjuvant chemotherapy regimens. Oncol Nurs Forum. 2009;5:49.
Derogar M, Orsini N, Sadr-Azodi O, Lagergren P. Influence of major postoperative complications on health-related quality of life among long-term survivors of esophageal cancer surgery. J Clin Oncol. 2012;30(14):1615–9.
Jacobs M, Macefield R, Elbers R, et al. Meta-analysis shows clinically relevant and long-lasting deterioration in health-related quality of life after esophageal cancer surgery. Qual Life Res. 2014;23(4):1097–115.
Hurmuzlu M, Aarstad H, Aarstad A, Hjermstad M, Viste A. Health-related quality of life in long-term survivors after high-dose chemoradiotherapy followed by surgery in esophageal cancer. Dis Esophagus. 2011;24(1):39–47.
Yang S, Chu S, Gao Y, et al. A narrative review of cancer-related fatigue (CRF) and its possible pathogenesis. Cells. 2019;8(7):738.
Jacobsen PB, Donovan KA, Vadaparampil ST, Small BJ. Systematic review and meta-analysis of psychological and activity-based interventions for cancer-related fatigue. Health Psychol. 2007;26(6):660.
Meneses-Echávez JF, González-Jiménez E, Ramírez-Vélez R. Effects of supervised multimodal exercise interventions on cancer-related fatigue: systematic review and meta-analysis of randomized controlled trials. BioMed Res Int. 2015;2:15.
Hagi T, Makino T, Yamasaki M, et al. Dysphagia score as a predictor of adverse events due to triplet chemotherapy and oncological outcomes in 434 consecutive patients with esophageal cancer. Ann Surg Oncol. 2019;26(13):4754–64.
Chen S-C, Yu P-J, Hong M-Y, et al. Communication dysfunction, body image, and symptom severity in postoperative head and neck cancer patients: factors associated with the amount of speaking after treatment. Support Care Cancer. 2015;23(8):2375–82.
Edmond SN, Shelby RA, Kimmick GG, Marcom PK, Peppercorn JM, Keefe FJ. Symptom communication in breast cancer: relationships of holding back and self-efficacy for communication to symptoms and adjustment. J Psychosoc Oncol. 2013;31(6):698–711.
Goldstein D, Bennett BK, Webber K, et al. Cancer-related fatigue in women with breast cancer: outcomes of a 5-year prospective cohort study. J Clin Oncol. 2012;30(15):1805–12.
Ruiz-Casado A, Álvarez-Bustos A, de Pedro CG, Méndez-Otero M, Romero-Elías M. Cancer-related fatigue in breast cancer survivors: a review. Clin Breast Cancer. 2020;6:108.
Larsen MK, Schultz H, Mortensen MB, Birkelund R. Patients’ experiences with illness, treatment, and decision-making for esophageal cancer: a qualitative study in a danish hospital setting. Global Qual Nurs Res. 2020;7:2333393620935098.
Acknowledgments
This work was supported by the National Taiwan University Hospital [grant number: 108-S4131]. The authors thank department of thoracic surgery of National Taiwan University Hospital in helping with patient recruitment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsou, YL., Lee, JM. & Tang, CC. The Trajectory of Cancer-Related Fatigue and Its Associating Factors in Patients with Esophageal Cancer Receiving Treatments: A Prospective Longitudinal Study. Ann Surg Oncol 29, 2784–2790 (2022). https://doi.org/10.1245/s10434-021-11294-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11294-2